Abstract
Background
Anxiety and depression are common psychological comorbidities that impact the quality of life (QoL) of patients. In this systematic review, we 1) determined the impact of anxiety and depression on outcomes in patients with osteoarthritis (OA) and 2) summarized unique challenges these comorbidities present to current OA management.
Patients and methods
A systematic literature search was performed using the OVID Medline and EMBASE databases until April 2016. Full-text research articles published in English from the year 2000 onward with a sample size of >100 were included in this review. Eligible research articles were reviewed and the following data were extracted: study author(s), year of publication, study design, and key findings.
Results
A total of 38 studies were included in the present review. The present study found that both anxiety and/or depression were highly prevalent among patients with OA. Patients with OA diagnosed with these comorbidities experienced more pain, had frequent hospital visits, took more medication, and reported less optimal outcomes. Management strategies in the form of self-care, telephone support, audio/video education programs, and new pharmacotherapies were reported with favorable results.
Conclusion
Anxiety and depression adversely impact the QoL of patients with OA. Physicians/caregivers are highly recommended to consider these comorbidities in patients with OA. Ultimately, a holistic individualized management approach is necessary to improve patient outcomes.
Introduction
Osteoarthritis (OA) is the most common musculoskeletal disease worldwide.Citation1 It is characterized by degeneration of the articular cartilage, osteophyte formation, and asymmetric joint space narrowing.Citation2 These changes often lead to significant pain and disability and create a substantial individual, societal, and economic burden.Citation3,Citation4 Since the incidence and prevalence of OA increase with age, longer life expectancy will only increase these measures in the future.Citation5 Current management largely emphasizes on alleviating symptoms and improving function, but for many these interventions do not provide adequate symptom relief. This variability in symptoms and outcomes among individuals with OA cannot be explained by the disease pathology alone.
Several factors are being investigated to explain differences in patient-reported symptoms and outcomes, of which anxiety and depression have begun to emerge as strong candidates.Citation6,Citation7 Anxiety is defined as the presence of “fear or nervousness about what might happen”.Citation8 When this fear produces behavioral and physiological changes, the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V) denotes this as anxiety disorder.Citation9 Depression, on the other hand, is defined as the presence of sad, empty, or irritable mood. Both anxiety and depression are accompanied by somatic and cognitive changes that can significantly affect an individual’s capacity to function.Citation9 Outside of OA, studies have consistently reported that anxiety and depression have significant impacts on cardiovascular diseases, chronic respiratory disorders, and gastrointestinal conditions.Citation10–Citation12 Patients suffering from chronic painful disabling conditions frequently report anxiety and depression as comorbidities.Citation13 This may predispose patients to experience pain more often, as recent evidence suggests that anxiety and depression can alter pain threshold levels.Citation14 Since chronic pain in itself can cause or aggravate anxiety and depression,Citation15 a vicious cycle begins, which can significantly impact the course and management of these chronic diseases.
Several studies have evaluated the concordance between OA, anxiety, and depression. Although substantial work has been conducted to elucidate the role of anxiety and depression in patients with OA, this study seeks to provide a comprehensive understanding regarding the impact these comorbidities have on OA symptoms, patient outcomes, and challenges they prensent towards disease management.
Patients and methods
Eligibility criteria
Original studies of 1) human subjects that 2) assessed anxiety or depression during any time point of the 3) OA disease course 4) regarding its impact on patient-reported symptoms and outcomes along with 5) different interventions employed to manage these comorbidities were included for this review. We limited eligibility to studies that were only in English language. Review articles, letters to the editor, published abstracts, book series, short surveys, notes, editorials, and case series were excluded. It has been reported that even with statistically significant results, studies with low sample sizes are less likely to reflect a true effect;Citation16,Citation17 therefore, reports concerning <100 patients were excluded. Additionally, only articles with full-text versions published from the year 2000 onward were eligible for this review to focus on recent updates in OA, anxiety, and depression.
Search strategy and criteria
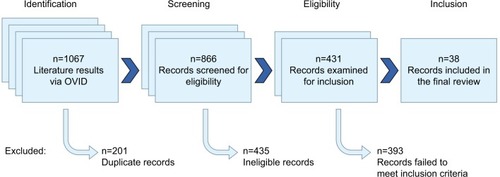
A manual electronic search of the OVID Medline (from 1996) and EMBASE (from 1974) databases was performed in duplicate by two authors (AS and PK) to identify studies published until April 2016 that assessed the impact or management of anxiety or depression in patients with OA. The following search string was used: “(osteoarthritis) and (anxiety or depression) and (impact or management)”. One thousand and sixty-seven records were identified after excluding non-English results. After performing automated deduplication using the OVID search interface, 866 studies remained.
Study selection
Citation records were extracted to Excel spreadsheet software (Microsoft Corp, Redmond, WA, USA) and sorted by publication-type metadata. No specialized systematic review software packages were used. Publication types not meeting inclusion criteria were removed (). These records were manually screened for eligibility by two authors (AS and PK), and any doubt regarding inclusion/exclusion of a particular study was addressed by discussion between the two authors. Unresolved conflicts were managed by discussion with two additional authors (QS and RG). Four hundred and thirty-five records were excluded as 233 were review articles, 174 were published abstracts, seven were conference papers, seven were notes, six were editorials, three were short surveys, two were letters, two were meta-analysis, and one was a book series. After excluding further 356 records based on title and abstract information, 21 records with a sample size of <100, and 16 records based on year of publication, 38 records were included in the final review.Citation18–Citation55 No systematic search of article bibliographies or conference proceedings was performed in an attempt to identify any additional unpublished or otherwise unidentified data. Full-length articles of the remaining 38 records were obtained and included in our final synthesis ().
Table 1 Final studies with authors, year of publication, design, and key findings
Data collection
Data extraction included the following elements: 1) authors, year of publication, 2) study design, and 3) key findings.
Study designs and study quality
Of all the final studies included in this review, six were randomized controlled trials,Citation18,Citation33,Citation39,Citation40,Citation52,Citation54 14 were prospec tive cohort studies,Citation20,Citation21,Citation30,Citation31,Citation34,Citation37,Citation41,Citation44,Citation46,Citation48,Citation49,Citation51,Citation55,Citation56 14 were cross-sectional studies,Citation19,Citation25–Citation29,Citation32,Citation36,Citation38,Citation43,Citation45,Citation47,Citation53,Citation57 one was a retro spective analysis,Citation35 and three were surveys.Citation23,Citation42,Citation50
Results
Sample and setting
Of the original 866 English articles, 38 articles fulfilled our aforementioned criteria and thus were included for analysis in this review.Citation18–Citation55 These 38 articles outline the impact of anxiety and/or depression on patients living with OA and the challenges these comorbidities present in OA management, wherein some studies also examined approaches on how to address these challenges. The age of patients analyzed in most of these studies was consistent with the age at which OA and depression are commonly diagnosed. However, one study specified a younger cutoff age range in their inclusion criteria.Citation45 Gignac et alCitation45 reported that middle-aged patients with OA (mean age 50.8 years) reported more depression compared to elderly subjects (mean age 67.8 years) having similar OA severity. This difference was attributed to role limitation and dissatisfaction among middle-aged OA individuals. Most studies included both male and female participants. However, in one study, sex was an eligibility criterion, as this study focused solely on female participants.Citation19 Studies were carried out in different settings viz university hospital, general practitioner (GP) clinics, and via telephone/mailed surveys. All studies published after year 2000 were analyzed ().
Anxiety and depression
All studies evaluated anxiety and/or depression either as a primary or a secondary objective. Various scoring methods were utilized, of which Centre for Epidemiological Studies Depression Scale (CES-D)Citation58 and Hospital Anxiety and Depression Scale (HADS) were most popular.Citation59 Both CES-D and HADS have been extensively used and studied, and are considered reliable and valid research tools.Citation60 Other scoring methods used were Composite International Diagnostic Interview,Citation13 36-Item or the 12-Item Short Form Health Survey (SF-12, SF-36),Citation61 Hopkins Symptom Checklist Depression Scale,Citation62 Patient Reported Outcome Measurement Information System,Citation63 Patient Health Questionnaire (PHQ),Citation64 visual analog scale, Arthritis Impact Measurement Scale,Citation65 Beck Depression Inventory,Citation66 and the Health Education Impact Questionnaire.Citation67 Apart from these scores, clinical diagnosis based on patient interviews was also utilized.
OA pathology and disease severity
Most studies focused on lower extremity OA (hip and knee), with one study examining hand OACitation38 patients. Diagnosis was based on clinical presentation or radiographs. Patients from the entire spectrum of disease severity were studied. The Kellgren and Lawrence (KL) radiographic grading system was most often used to report OA severity; however, some studies did not use any specific grading method. One study included patients with early (KL I, II) and late (KL III, IV) stage OA.Citation32 Pain was a consistent feature across most studies and was assessed primarily using the Western Ontario & McMaster Universities Osteoarthritis Index.Citation68 In addition to OA, two studies also assessed patients with rheumatoid arthritis.Citation19,Citation33
Epidemiology of anxiety and depression in patients with OA
Three studies reported on the prevalence of anxiety and depression in patients with OA.Citation24,Citation29,Citation41 Rosemann et alCitation29 conducted a cross-sectional survey in 1,021 patients with OA and reported that psychological factors (viz anxiety and depression) were highly prevalent among the patients (19.76% of male and 19.16% of female participants reported a PHQ-9 score of ≥15). Similar results were reported by Sale et alCitation24 in a cross-sectional study where 21.3% of 1,227 participants reported a CES-D score of ≥16. Likewise, Kirkness et alCitation41 reported that major depressive disorder was commonly prevalent in patients scheduled for total knee arthroplasty.
Impact
Impact of anxiety and depression on OA symptoms
Of the 38 studies included in our final analysis, 13 studies examined the impact of anxiety and depression on OA symptoms.Citation18,Citation19,Citation26,Citation31,Citation32,Citation38,Citation43,Citation45,Citation46,Citation48,Citation50,Citation55 There was a considerable overlap in reporting impact of these psychological conditions on patients with OA with pain being the key central element. Studies reported that the prevalence of anxiety and depression was interrelated to index joint pain,Citation55 pain at multiple sites,Citation31,Citation50 pain intensity,Citation25 and OA severity.Citation32 Pain was in turn associated with depression and its recurrence.Citation46 Hawker et alCitation43 also reported that current OA pain predicted future fatigue, disability, and depressed mood. In addition to its impact on OA pain, concurrent depression was also interrelated to significant participation restriction and physical limitation.Citation26,Citation45
Impact of anxiety and depression on OA outcomes
Nine studies examined the impact of anxiety and depression on the outcomes of patients with OA.Citation20,Citation27,Citation30,Citation34,Citation35,Citation37,Citation44,Citation52,Citation53 Studies reported that anxiety and depression increased GP visits,Citation52 health care utilization,Citation27 drug prescriptions,Citation53 adversely affected surgical outcomes,Citation30,Citation34,Citation35,Citation37,Citation44 and increased post-surgical pain.Citation20
Impact of anxiety and depression on patients with OA: sex differences
Our results indicate that anxiety and depression differentially impact lives of male and female patients with OA. Sale et alCitation24 reported that higher level of depressed mood was independently and significantly associated with the female sex.
Management challenges
Thirteen studies evaluated management challenges in patients with OA with comorbid anxiety and depression.Citation21–Citation23,Citation28,Citation33,Citation36,Citation39,Citation40,Citation42,Citation47,Citation49,Citation51,Citation54 The present study found that anxiety and depression posed unique challenges to physicians in 1) diagnosis, 2) structuring a proper management plan, and 3) effective pharmacotherapy.
Challenges in diagnosis of anxiety and depression
Primary care physicians or GPs infrequently considered or found it difficult to diagnose anxiety and/or depression in patients with OA.Citation28,Citation42
Challenges in self-care, collaborative care, social/phone support
Management regimes advocating self-care, social/phone support, and educational engagements in patients with OA with comorbid anxiety and depression were reported. Lin et alCitation39 reported that systematic depression management (antidepressant pharmacotherapy and/or problem-solving treatment) was more effective than usual care in decreasing pain severity among patients with arthritis with lower initial pain severity, but not among patients with higher initial pain severity. On the contrary, Buszewicz et alCitation52 reported that although self-management reduced anxiety, it had no significant effect on pain, physical functioning, or number of GP visits at 12 months.
Challenges in pharmacotherapy
Pharmacological challenges exist in managing patients with OA with comorbid anxiety and depression. These challenges juxtaposed with the demographics of this patient cohort (advanced age and presence of other medical comorbidities) make pharmacotherapy difficult. Therefore, it is vital to investigate new treatment modalities that could effectively manage these conditions with minimum adverse effects. The present study found that rofecoxib and tapentadol were reported to improve pain and depressive symptoms of patients with OA. Theiler et alCitation21 assessed the effects of rofecoxib on quality of life (QoL) in elderly patients with painful OA flares who were not responsive to or had adverse reactions to previous NSAID therapy. The authors reported that rofecoxib significantly improved QoL, as measured by the SF-12. Similarly, Collantes-Esteve and Fernandez-PerezCitation51 found rofecoxib to favorably influence patients with OA with self-reported depression. In addition to rofecoxib, use of tapentadol (prolonged and immediate release) has also been reported in patients with chronic painful knee OA. Steigerwald et alCitation22 evaluated effectiveness of tapentadol prolonged release in 195 patients with chronic OA knee pain and found significant improvement in pain intensity, QoL, SF-36, and HADS.
New management approaches: music, video, and yoga
In recent years, various new and innovative management methodologies have been investigated. Ayral et alCitation54 reported that advocating video education information on the planned procedure before surgery lowered perioperative anxiety. Music therapy and yoga have also been reported to help improve patient anxiety and depression; however, the sample sizes of their respective studies were small.Citation69,Citation70
Discussion
Psychological comorbidities (anxiety and depression) are highly prevalent among patients with OA.Citation24,Citation29,Citation41,Citation49 These comorbidities are frequently associated with higher pain and physical limitation,Citation18,Citation19,Citation26,Citation31,Citation32,Citation38,Citation43,Citation45,Citation46,Citation48,Citation50,Citation55 poor outcomes to both conservative and surgical interventions,Citation20,Citation30,Citation31,Citation34,Citation35,Citation37,Citation44,Citation47,Citation56 and increased pharmacotherapy and health care utilization.Citation23,Citation48 Our results indicate that standardized interventions to manage these comorbidities are lacking as a number of different self-care management programs, telephone support programs, video information support programs, and new drug treatments were reported in the literature with varied success.Citation21–Citation23,Citation28,Citation33,Citation36,Citation39,Citation40,Citation42,Citation47,Citation49,Citation51,Citation54 This variability in patient care highlights the complex relationship that exists between OA, anxiety, and depression (). Yet, these comorbidities are commonly overlooked by many primary care physicians and GPs who either solely focus on physical aspects of OA or simply fail to assess patients’ psychological state altogether.Citation71 It is imperative to recognize these comorbidities, as these can influence disease course and management, ultimately affecting functional outcomes.
Table 2 Summary of results
Anxiety and depression are interrelated with pain and physical limitation, the two key OA symptoms. Studies in our review have revealed that anxiety and depression can significantly impair QoL of patients by altering pain perception and functional capacity.Citation24 Therefore, educating physicians about timely identification of psychosocial factors such as anxiety and depression that may pre-date OA pathology or result as a consequence of the disease can improve the QoL of patients living with these comorbidities. The National Institute for Health and Care Excellence (NICE) has outlined recommendations regarding holistic assessment of patients with OA (https://www.nice.org.uk/guidance/cg177), which serves as an excellent starting point and it is highly recommended that physicians consult this document. Thus, implementation of appropriate screening questionnaires can help identify these psychological comorbidities at an earlier stage, which could in effect provide adequate lead time to implement a management plan that could improve outcomes and lower future health care burden and costs.
OA is a progressive disease and a large portion of patients with OA will, at some point, undergo surgery. Patients awaiting surgery can experience anxiety; however, educating them about the procedure and advocating a self-care plan can change health-directed behaviors. While surgery does improve QoL of patients, patients with OA with comorbid anxiety and depression may not experience similar favorable clinical outcomes following joint replacement surgery as seen in patients with OA without these comorbidities,Citation20,Citation30,Citation34,Citation35,Citation37,Citation44,Citation47,Citation56 even after a structured rehabilitation program.Citation72 Thus, surgical indications in patients with OA with comorbid anxiety and depression should be critically assessed as not all patients report similar benefits following surgery.
As seen in our results, OA management strategies include self-care, collaborative care, social/phone support, pharmacotherapy, music, educational videos about OA procedures, and yoga. Self-care, collaborative care, and social/phone support should be integrated into OA management, as these strategies have been shown to alter comorbid anxiety and depression, as well as resulting physical and emotional pain. Similarly, pharmacotherapy should also be appropriately integrated into OA management; however, this should be done carefully, as the treatment of OA, depression, anxiety, and pain through pharmacotherapy carries the danger of drug interactions and adverse side effects. From our study, we can suggest rofecoxib and tapentadol to improve QoL and pain of patient with OA and encourage the development of new treatment modalities that work in tandem to treat OA symptoms, as well as comorbidities. Additionally, there is evidence that anti-depressant medications such as duloxetine can improve pain in patients with OA,Citation73 suggesting a central mechanism that may connect OA pain and depression. Therefore, it would be appropriate to consider implementing anti-depressant/anti-anxiety therapy in tandem with non-steroidal anti-inflammatory drugs and/or analgesic drugs to address these different pain pathways concurrently. This multi-faceted pharmacological approach can greatly benefit patients in this cohort. Other newer modalities such as music, videos, and yoga are management methods that have recently gained more attention, as they have been shown to improve patient outcomes. Music has been shown to reduce levels of anxiety, depression, and pain. Likewise, videos educating patients on their planned surgical procedures have lowered pre-operative anxiety. These modalities can act as adjuvants to current management strategies.
To create individualized OA management strategies, it is essential to recognize that patients with early OA disease experience less anxiety and depression compared to patients with late-stage disease.Citation32 Therefore, radiological severity of OA can serve as an indicative factor for intensity of depression in patients with OA. This concept should be further investigated. Similarly, sex differences are prevalent independently in OA, anxiety, and depression.Citation74,Citation75 Studies have reported that female patients with OA report greater anxiety and depressionCitation24,Citation76 and lower QoLCitation38 than males. Moreover, female patients with OA may have different expectations than their male counterparts and therefore may require a completely different management approach.
It is important to state that present literature fails to fully address the management strategies in dealing with psychological comorbidities seen in patients with OA. It is rather clear that one treatment does not fit all, as seen in the present review. On one end self-management interventions did not improve pain, QoL, or depression,Citation77 while on the other hand, self-management did produce improvement in exercise and relaxation activities in depressed patients although not as much as in patients without depression.Citation33 These conflicting results highlight the challenges present in the management of these comorbidities today. It should also be highlighted that recruiting and retaining patients in management programs is also challenging and should be further evaluated to increase patient compliance, as depressed patients tend to lack interest from the outset. Furthermore, another factor in need of consideration is age, and how reports of depression/anxiety can differ based on patients’ age group. To garner an accurate understanding of how depression/anxiety interacts with OA, it is important to consider the possibility that different age groups experience varying degrees of depression/anxiety, based on a diverse set of factors, such as socioeconomic status and health complications. Recent trends in depression suggest its high prevalence among individuals aged 40–59 years, which may thus affect the presentation of OA to a greater degree in middle-aged cohorts than younger or elderly cohorts.Citation78 Therefore, examining the impact and management challenges of anxiety and depression in an age-stratified OA cohort should be further investigated.
Although our results provide a comprehensive summary of the current state of literature, a considerable lack of studies originating from outside of North America and Europe is noted. This could be attributed to the fact that outpatient visits and in-patient admissions for mental health diseases are higher in the US and Europe,Citation79 or it could simply underscore a general lack of research initiatives in the developing world, or that psychological conditions largely remain under-recognized and/or under-diagnosed. Thus, the inclusion of studies from developing nations may provide a more detailed picture of the relationship between anxiety, depression, and OA. We also acknowledge that the exclusion of reports not published in English may have introduced institutional bias. Furthermore, in addition to the inherent weaknesses of the studies reviewed, our study may be skewed by publication bias, as there is a well-described prejudice toward the publication of positive findings. Nevertheless, we believe that the present review accurately presents the current state of evidence concerning the impact and management challenges of anxiety and depression encountered by patients with OA.
Conclusion
In summary, the majority of evidence regarding impact of anxiety and depression in patients with OA suggests reduced QoL and poor clinical outcomes. The current literature fails to lay a blueprint to tackle the management challenges seen. OA stage-specific stratification may help guide management. However, further studies are needed to formulate definitive management strategies to deal with OA-associated anxiety and depression and should focus on high-quality randomized controlled trials with patients stratified into non-operative, pre-operative/operative, and post-operative groups.
Acknowledgments
We thank Dr Jason Rockel, Research Associate at Krembil Research Institute, for comments that greatly improved the manuscript.
Disclosure
The authors report no conflicts of interest in this work
References
- JohnsonVLHunterDJThe epidemiology of osteoarthritisBest Pract Res Clin Rheumatol201428151524792942
- LoriesRJLuytenFPThe bone-cartilage unit in osteoarthritisNat Rev Rheumatol201171434921135881
- HunterDJSchofieldDCallanderEThe individual and socioeconomic impact of osteoarthritisNat Rev Rheumatol201410743744124662640
- LitwicAEdwardsMHDennisonEMCooperCEpidemiology and burden of osteoarthritisBr Med Bull201310518519923337796
- LawrenceRCFelsonDTHelmickCGNational Arthritis Data WorkgroupEstimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part IIArthritis Rheum2008581263518163497
- AxfordJButtAHeronCPrevalence of anxiety and depression in osteoarthritis: use of the Hospital Anxiety and Depression Scale as a screening toolClin Rheumatol201029111277128320721594
- van BaarMEDekkerJLemmensJAOostendorpRABijlsmaJWPain and disability in patients with osteoarthritis of hip or knee: the relationship with articular, kinesiological, and psychological characteristicsJ Rheumatol19982511251339458215
- Merriam-Webster.com [homepage on the Internet]Anxiety2016 Available from: http://www.merriam-webster.com/Accessed September 16, 2016
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental DisordersWashington, DCAPA2013
- MaurerJRebbapragadaVBorsonSACCP Workshop Panel on Anxiety and Depression in COPDAnxiety and depression in COPD: current understanding, unanswered questions, and research needsChest20081344 suppl43S56S18842932
- JanuzziJLJrSternTAPasternakRCDeSanctisRWThe influence of anxiety and depression on outcomes of patients with coronary artery diseaseArch Intern Med2000160131913192110888966
- Mikocka-WalusAATurnbullDAMouldingNTWilsonIGAndrewsJMHoltmannGJControversies surrounding the comorbidity of depression and anxiety in inflammatory bowel disease patients: a literature reviewInflamm Bowel Dis200713222523417206706
- HeYZhangMLinEHMental disorders among persons with arthritis: results from the World Mental Health SurveysPsychol Med200838111639165018298879
- NeogiTNevittMCYangMCurtisJRTornerJFelsonDTConsistency of knee pain: correlates and association with functionOsteoarthritis Cartilage201018101250125520708003
- HansenGRStreltzerJThe psychology of painEmerg Med Clin North Am200523233934815829386
- ButtonKSIoannidisJPMokryszCPower failure: why small sample size undermines the reliability of neuroscienceNat Rev Neurosci201314536537623571845
- NueschETrelleSReichenbachSSmall study effects in meta-analyses of osteoarthritis trials: meta-epidemiological studyBMJ2010341c351520639294
- ZulligLLBosworthHBJeffreysASThe association of comorbid conditions with patient-reported outcomes in Veterans with hip and knee osteoarthritisClin Rheumatol20153481435144124916605
- YılmazHKaracaGDemir PolatHAAkkurtHEComparison between depression levels of women with knee osteoarthritis, rheumatoid arthritis, and fibromyalgia syndrome: a controlled studyTurk J Phys Med Rehab201561197202
- WyldeVDixonSBlomAWThe role of preoperative self-efficacy in predicting outcome after total knee replacementMusculoskeletal Care201210211011822368121
- TheilerRBischoffHAGoodMUebelhartDRofecoxib improves quality of life in patients with hip or knee osteoarthritisSwiss Med Wkly200213239–4056657312571763
- SteigerwaldIMullerMKujawaJBalblancJCCalvo-AlenJEffectiveness and safety of tapentadol prolonged release with tapentadol immediate release on-demand for the management of severe, chronic osteoarthritis-related knee pain: results of an open-label, phase 3b studyJ Pain Res2012512113822792000
- StammTAPieberKBlascheGDornerTEHealth care utilisation in subjects with osteoarthritis, chronic back pain and osteoporosis aged 65 years and more: mediating effects of limitations in activities of daily living, pain intensity and mental diseasesWien Med Wochenschr20141647–816016624468829
- SaleJEGignacMHawkerGThe relationship between disease symptoms, life events, coping and treatment, and depression among older adults with osteoarthritisJ Rheumatol200835233534218203312
- RosemannTLauxGSzecsenyiJWensingMGrolRPain and osteoarthritis in primary care: factors associated with pain perception in a sample of 1,021 patientsPain Med20089790391018702636
- RosemannTLauxGKuehleinTOsteoarthritis and functional disability: results of a cross sectional study among primary care patients in GermanyBMC Musculoskelet Disord200787917686172
- RosemannTJoosSSzecsenyiJLauxGWensingMHealth service utilization patterns of primary care patients with osteoarthritisBMC Health Serv Res2007716917956605
- RosemannTGensichenJSauerNLauxGSzecsenyiJThe impact of concomitant depression on quality of life and health service utilisation in patients with osteoarthritisRheumatol Int200727985986317242902
- RosemannTBackenstrassMJoestKRosemannASzecsenyiJLauxGPredictors of depression in a sample of 1,021 primary care patients with osteoarthritisArthritis Rheum200757341542217394226
- PintoPRMcIntyreTFerreroRAlmeidaAAraujo-SoaresVPredictors of acute postsurgical pain and anxiety following primary total hip and knee arthroplastyJ Pain201314550251523541065
- PerruccioAVPowerJDEvansHMMultiple joint involvement in total knee replacement for osteoarthritis: effects on patient-reported outcomesArthritis Care Res (Hoboken)201264683884622570306
- OzcakirSRaifSLSivriogluKKucukcakirNRelationship between radiological severity and clinical and psychological factors in knee osteoarthritisClin Rheumatol201130121521152621556778
- NourKLaforestSGauvinLGignacMBehavior change following a self-management intervention for housebound older adults with arthritis: an experimental studyInt J Behav Nutr Phys Act200631216734904
- MontinLLeino-KilpiHKatajistoJLepistoJKettunenJSuominenTAnxiety and health-related quality of life of patients undergoing total hip arthroplasty for osteoarthritisChronic Illn20073321922718083678
- MarksRComorbid depression and anxiety impact hip osteoarthritis disabilityDisabil Health J200921273521122740
- MarksRPhysical and psychological correlates of disability among a cohort of individuals with knee osteoarthritisCan J Aging200726436737718304923
- Lopez-OlivoMALandonGCSiffSJPsychosocial determinants of outcomes in knee replacementAnn Rheum Dis201170101775178121791452
- LiuRDammanWBeaart-van de VoordeLAesthetic dissatisfaction in patients with hand osteoarthritis and its impact on daily lifeScand J Rheumatol201645321922326471328
- LinEHTangLKatonWHegelMTSullivanMDUnutzerJArthritis pain and disability: response to collaborative depression careGen Hosp Psychiatry200628648248617088163
- LinEHKatonWVon KorffMIMPACT InvestigatorsEffect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trialJAMA2003290182428242914612479
- KirknessCSMcAdam-MarxCUnniSCharacterization of patients undergoing total knee arthroplasty in a real-world setting and pain-related medication prescriptions for management of postoperative painJ Pain Palliat Care Pharmacother201226432633323216171
- KingsburySRConaghanPGCurrent osteoarthritis treatment, prescribing influences and barriers to implementation in primary carePrim Health Care Res Dev201213437338122464219
- HawkerGAGignacMABadleyEA longitudinal study to explain the pain-depression link in older adults with osteoarthritisArthritis Care Res (Hoboken)201163101382139020662042
- HanuschBCO’ConnorDBIonsPScottAGreggPJEffects of psychological distress and perceptions of illness on recovery from total knee replacementBone Joint J201496-B221021624493186
- GignacMABackmanCLDavisAMLacailleDCaoXBadleyEMSocial role participation and the life course in healthy adults and individuals with osteoarthritis: are we overlooking the impact on the middle-aged?Soc Sci Med201381879323312300
- GerritsMMvan OppenPLeoneSSvan MarwijkHWvan der HorstHEPenninxBWPain, not chronic disease, is associated with the recurrence of depressive and anxiety disordersBMC Psychiatry20141418724965597
- EllisHBHowardKJKhaleelMABucholzREffect of psychopathology on patient-perceived outcomes of total knee arthroplasty within an indigent populationJ Bone Joint Surg Am20129412e8422717836
- DieppePCushnaghanJTuckerMBrowningSShepstoneLThe Bristol ‘OA500 study’: progression and impact of the disease after 8 yearsOsteoarthritis Cartilage200082636810772234
- DailianaZHPapakostidouIVaritimidisSPatient-reported quality of life after primary major joint arthroplasty: a prospective comparison of hip and knee arthroplastyBMC Musculoskelet Disord20151636626612135
- CroftPJordanKJinksC“Pain elsewhere” and the impact of knee pain in older peopleArthritis Rheum20055282350235416052574
- Collantes-EstevezEFernandez-PerezCImproved control of osteoarthritis pain and self-reported health status in non-responders to celecoxib switched to rofecoxib: results of PAVIA, an open-label post-marketing survey in SpainCurr Med Res Opin200319540241013678477
- BuszewiczMRaitGGriffinMSelf management of arthritis in primary care: randomised controlled trialBMJ2006333757487917040926
- BlagestadTNordhusIHGronliJPrescription trajectories and effect of total hip arthroplasty on the use of analgesics, hypnotics, antidepressants, and anxiolytics: results from a population of total hip arthroplasty patientsPain2016157364365126588693
- AyralXGicquereCDuhaldeABouchenyDDougadosMEffects of video information on preoperative anxiety level and tolerability of joint lavage in knee osteoarthritisArthritis Rheum200247438038212209483
- AxfordJHeronCRossFVictorCRManagement of knee osteoarthritis in primary care: pain and depression are the major obstaclesJ Psychosom Res200864546146718440398
- RiddleDLKongXFitzgeraldGKPsychological health impact on 2-year changes in pain and function in persons with knee pain: data from the Osteoarthritis InitiativeOsteoarthritis Cartilage20111991095110121723400
- KimKWHanJWChoHJAssociation between comorbid depression and osteoarthritis symptom severity in patients with knee osteoarthritisJ Bone Joint Surg Am201193655656321411706
- RadloffLSThe CES-D Scale: a self-report depression scale for research in the general populationAppl Psychol Measurement19771385401
- ZigmondASSnaithRPThe hospital anxiety and depression scaleActa Psychiatr Scand19836763613706880820
- BjellandIDahlAAHaugTTNeckelmannDThe validity of the Hospital Anxiety and Depression Scale. An updated literature reviewJ Psychosom Res2002522697711832252
- WareJJrKosinskiMKellerSDA 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validityMed Care19963432202338628042
- DerogatisLRLipmanRSRickelsKUhlenhuthEHCoviLThe Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensionsMod Probl Pharmacopsychiatry197470791104607278
- CellaDRileyWStoneAPROMIS Cooperative GroupThe patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008J Clin Epidemiol201063111179119420685078
- SpitzerRLKroenkeKWilliamsJBValidation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health QuestionnaireJAMA1999282181737174410568646
- MeenanRFGertmanPMMasonJHMeasuring health status in arthritis. The arthritis impact measurement scalesArthritis Rheum19802321461527362665
- BeckATWardCHMendelsonMMockJErbaughJAn inventory for measuring depressionArch Gen Psychiatry1961456157113688369
- OsborneRHElsworthGRWhitfieldKThe Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditionsPatient Educ Couns200766219220117320338
- BellamyNThe WOMAC knee and hip osteoarthritis indices: development, validation, globalization and influence on the development of the AUSCAN Hand Osteoarthritis IndicesClin Exp Rheumatol2005235 suppl 39S148S15316273799
- MiddletonKRWardMMHaazSA pilot study of yoga as self-care for arthritis in minority communitiesHealth Qual Life Outcomes2013115523548052
- OttavianiSBernardJLBardinTRichettePEffect of music on anxiety and pain during joint lavage for knee osteoarthritisClin Rheumatol201231353153422207250
- TurnerJKellyBEmotional dimensions of chronic diseaseWest J Med2000172212412810693376
- von der HoehNHVoelkerAGulowJUhleUPrzkoraRHeydeCEImpact of a multidisciplinary pain program for the management of chronic low back pain in patients undergoing spine surgery and primary total hip replacement: a retrospective cohort studyPatient Saf Surg201483425473419
- Abou-RayaSAbou-RayaAHelmiiMDuloxetine for the management of pain in older adults with knee osteoarthritis: randomised placebo-controlled trialAge Ageing201241564665222743149
- McLeanCPAsnaaniALitzBTHofmannSGGender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illnessJ Psychiatr Res20114581027103521439576
- O’ConnorMISex differences in osteoarthritis of the hip and kneeJ Am Acad Orthop Surg200715suppl 1S22S2517766785
- TheisKAHelmickCGHootmanJMArthritis burden and impact are greater among U.S. women than men: intervention opportunitiesJ Womens Health (Larchmt)200716444145317521246
- CrottyMPrendergastJBattersbyMWSelf-management and peer support among people with arthritis on a hospital joint replacement waiting list: a randomised controlled trialOsteoarthritis Cartilage200917111428143319486959
- PrattLABrodyDJDepression in the U.S. Household Population, 2009–2012Hyattsville, MDNational Center for Health Statistics2014
- WHOMental Health Atlas 2014GenevaWHO2015