Abstract
Introduction
Colonic volvulus is an unusual cause of intestinal obstruction in pregnant women. Cecal volvulus, second only to sigmoid volvulus, accounts for 1–2% of all cases of intestinal obstruction. Due to its infrequent occurrence, only a few articles have documented its diagnosis and management among pregnant women, and we assume this to be the first reported case in Ethiopia, as per the authors’ knowledge.
Case Presentation
A 26-year-old Gravida 3, Para 2 mother who has had amenorrhea for the last five months presents with a complaint of upper abdominal cramps with associated vomiting, which is bilious, upper abdominal distension, and obstipation of five-hour duration. Her vital signs were in the normal range, and she had upper abdominal tenderness. Plain abdominal radiography suggested a cecal volvulus and exploratory laparotomy, a right hemicolectomy, and end-to-side ileotransverse colon anastomosis was performed. The postoperative course was uneventful.
Discussion
The cecal volvulus is an axial twist of the cecum, segment of the terminal ileum, and ascending colon along its mesentery, resulting in closed-loop obstruction with early vascular compromise and ischemia. It requires an anatomic prerequisite, which makes the cecum hypermobile, unlike the sigmoid volvulus. Diagnosis is challenging in pregnant women, as there are many differential diagnoses and a reluctance to request radiological imaging.
Conclusion
A high index of suspicion is of paramount importance whenever a pregnant woman comes with a complaint of persistent abdominal cramps and obstipation. Early diagnosis and management are crucial to improve patients’ outcome. Plain abdominal radiography is the safest option of imaging modality in low-resource areas where magnetic resonance imaging (MRI) is not available during pregnancy whenever intestinal obstruction is considered. Right hemicolectomy is the preferred surgical option.
Introduction
The cecal volvulus is the twisting of the cecum, part of the ascending colon, and terminal ileum around the ileocolic pedicle. It is a rare cause of intestinal obstruction, accounting for approximately 1–2% of cases.Citation1 It is second to sigmoid volvulus as a cause of colonic volvulus accounting for 25–40% of cases.Citation1
The incidence of intestinal obstruction during pregnancy is rare and varies widely, from 1:66,432 to 1:1500 deliveries; the latter approximates the incidence of appendicitis during pregnancy.Citation2,Citation3 In spite of this clinically significant frequency, there are only a few reports or series of patients that discuss the diagnosis and management of this unusual and catastrophic surgical and obstetric condition.Citation2,Citation4
Pregnancy has a particular effect by displacing the cecum from its location in the right iliac fossa and increasing mobility. Other predisposing factors include non-fixed mobile cecum, previous surgery, postoperative adhesion, pelvic mass, chronic constipation, megacolon, and a high-fiber diet.Citation4
As its presentation is vague and similar to other gastrointestinal conditions during pregnancy, such as hyperemesis gravidarum, preeclampsia, cholecystitis, and gastroesophageal reflux disease, delaying its diagnosis is not uncommon. Here, we present the case of a 26-year-old Gravida 3, Para 2 mother who presented with an acute intestinal obstruction. This study is in line with the Surgical CAse Report (SCARE) guideline.Citation5
Case Presentation
A 26-year-old Gravida 3, Para 2 mother who has had amenorrhea for the last five months presented with a complaint of central abdominal cramps associated with bilious vomiting and upper abdominal distension. The duration of her complaints was only five hours. The patient had no fever, chills, or rigor, and no history of vaginal discharge, bleeding, abdominal trauma, or abdominal surgery. She was neither a smoker nor an alcoholic. She had no past medical illnesses or comorbidities.
Physical examination revealed an acutely sick-looking patient, but vital signs were all within the normal range, with a pulse rate of 94 beats per minute, blood pressure of 100/70 mmHg, respiratory rate of 24 breaths per minute, and temperature of 37.2 °C. Her oxygen saturation was 96% with atmospheric oxygen. The pertinent physical findings were an abdominal examination, in which she had an 18-week-sized gravid uterus with a grossly distended upper abdomen, hyperactive bowel sounds, and mild tenderness over the upper abdomen. A digital rectal examination revealed an empty rectum. Possible differential diagnoses of dyspepsia, cholecystitis, intestinal obstruction, and other pregnancy-related conditions, such as preeclampsia with severity features, are considered, and obstetric units are also involved in the management.
Baseline laboratory examinations showed a white cell count of 10.4*103/µL with polymorph neutrophils accounting for 41.5%, hemoglobin of 10.2 g/dl, MCV of 76.5 FL, and a platelet count of 466 × 103/µL. Urine analysis and blood chemistry results were unremarkable.
Obstetric and abdominal ultrasound workups were also performed by obstetrics and gynecology residents and a consultant radiologist, respectively, and indicated a viable singleton intrauterine pregnancy with a gestational age of 18 weeks and 1 day, an EFW of 271 g, and a fundal placenta. It was difficult to evaluate bowel loops because they were gaseous and distended. Otherwise, liver, gallbladder, and other organs were normal, except for right moderate and left mild hydronephrosis. Since MRI was not available, a plain abdominal film was taken, which revealed a markedly air-filled, dilated large bowel extending from the right lower quadrant with maintained haustral markings and seen in the left upper quadrant, highly suggestive of cecal volvulus ().
Figure 1 Markedly air filled dilated large bowel extending from right lower quadrant to left upper quadrant, highly suggestive of cecal volvulus.

The patient was then kept nil by mouth and resuscitated with intravenous crystalloids; an indwelling urinary Foley catheter was inserted; and the patient was prepared for exploration after obtaining written informed consent.
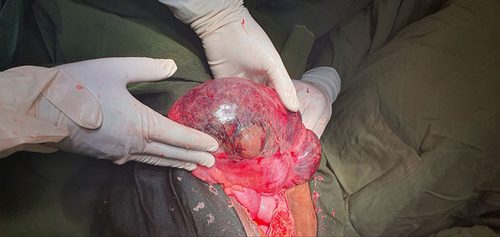
The patient was taken to the operating room, placed in the supine position under general anesthesia, and an endotracheal tube abdomen was prepared and draped. The abdomen was then entered through a vertical midline laparotomy incision, and the intraoperative findings were around 200 mL of reactive fluid, 540° clockwise twisted cecum together with ascending colon and proximal transverse colon; the wall of the cecum was thinned out and ischemic but not perforated; the cecum was not fixed to its usual right iliac fossa and was found to be higher in the right upper quadrant, with the duodenojejunal junction situated in the right midline ( and ). Otherwise, no other pathology was identified, the rotated segment was resected en bloc, a right hemicolectomy was performed, and bowel continuity was retained with an end-to-side ileotransverse colon anastomosis.
Figure 2 Intra-op finding showing markedly dilated, thinned out cecum with ischemic and necrotic changes over its anterior wall.
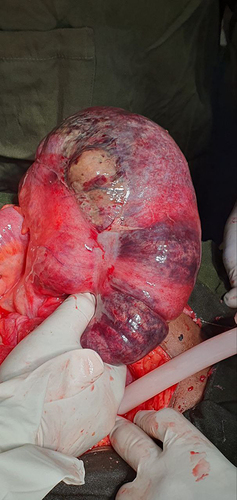
Figure 3 Axial twist of cecum along with its mesentery resulting in dilation, ischemia and necrosis of its anti-mesenteric surface.
The patient had an uneventful hospital course and was discharged after improvement following follow-up in the ward with intravenous antibiotics, analgesics, and a fetomaternal condition being followed by a biophysical profile. She resumed enteral feeding on the second postoperative day and stayed for a total of six days, which was a smooth postoperative course, and discharged improved. The patient was subsequently followed up at our referral clinic, and antenatal follow-up at our obstetrics unit had a smooth postoperative course. She has recently given birth to an alive female neonate in our hospital via spontaneous vaginal delivery, and the delivery was uneventful.
Discussion
Though there are limitations to the data on the incidence of cecal volvulus in East Africa, the prevalence of sigmoid volvulus is higher.Citation6 Intestinal obstruction complicating pregnancy is an uncommon phenomenon, with significant morbidity and mortality in both the mother and developing fetus occurring in 1:66,432 to 1:1500 deliveries.Citation2
The most common causes of intestinal obstruction during pregnancy are adhesions (58%), volvulus (25%), and intussusception (5%).Citation4 However, small bowel volvulus, intussusception, adhesion, and hernia account for the most frequent causes of intestinal obstruction in the general population in Ethiopia.Citation7
Cecal volvulus, the second most common cause of colonic volvulus, results from non-fixation of the right colon with an axial twist and closed-loop obstruction.Citation3,Citation8 It occurs in 1:2500 to 1:3500 pregnancies and accounts for 1–2% of all intestinal obstructions.Citation1,Citation3,Citation9 This condition was initially described by Rokitansky in 1837.Citation10 It has a slight female predominance in its frequency and a peculiar congenital anatomic variant involving incomplete peritoneal fixation of the right colon and associated heightened cecal mobility.Citation11,Citation12
Cecal hypermobility due to incomplete fixation or malrotation is evident in about 20–25% of cadaveric studies.Citation11 However, there is a marked discordance between the incidence of mobile cecum and the occurrence of cecal volvulus, signifying the presence of other factors contributing to its development.
Some studies have reported that approximately 23–53% of patients with cecal volvulus have a history of prior abdominal surgery, leading to postoperative adhesion and resulting in the formation of fixation points and a fulcrum of rotation for the mobile right colon.Citation12,Citation13
It has two variants, the first and most common being an axial twist over the ileocolic vessels with early ischemic changes and gangrene, which occurred in our patient. The second variant is the cecal base, which involves only the anterior folding of the cecum to the ascending colon. This rarely results in a vascular compromise.Citation11
The incidence of cecal volvulus during pregnancy increases with gestational age and rapid changes in the size of the uterus, particularly between 16 and 20 weeks of gestation, when the uterus becomes intra-abdominal, from 32 to 34 weeks, when the fetus descends, and in the puerperium, when uterine size changes rapidly.Citation9 Our patient had the two most important prerequisites for the development of cecal volvulus: a non-fixed mobile cecum and a typical gestational age of 16–20 weeks. Female sex and a relatively younger age are additional factors consistent with the evidence we have regarding the condition.
The clinical presentation of patients with such conditions can be grouped into three categories.Citation11,Citation13 The first group of patients presented with an intermittent, recurrent pattern of obstruction, referred to as “mobile cecum syndrome”.Citation13 These patients manifest episodes of localized or generalized pain, distension, and vomiting, which are relieved by the passage of the flatus. This presentation is usually confused with normal gastrointestinal conditions during pregnancy, such as hyperemesis gravidarum, dyspepsia, cholecystitis, and preeclampsia and results in a delayed diagnosis.
The second category presents with an acute obstructive pattern that, if left untreated, progresses to third and highly lethal condition of strangulation and perforation, leading to peritonitis.Citation11,Citation13 Again, our patient’s early presentation with an obstructive pattern and persistent pain with intraoperative findings of ischemic and gangrenous distended cecum with early vascular compromise is consistent with other studies.
In a case reported by Xh Draçini, the initial presentation was similar to that of our patient, but in the case they reported, the patient was in septic shock. The fetus was dead intrauterine and the cecum, part of the ascending colon and terminal ilium were gangrenous.Citation14 They performed a right hemicolectomy and a lower uterine transverse cesarean section to deliver the dead fetus, and the patient was discharged on the 9th postoperative day. In our particular case, the obstetric side was involved, and the fetomaternal status was assessed prior to taking the patient to operating room as well as in the postoperative follow-ups.
Kreinces et al also reported the other type of cecal volvulus, which is the cecal bascule in a 36-year-old woman at 36 weeks of gestational age.Citation15 In their case, the diagnosis was made by MRI, and cesarean section and abdominal exploration were performed. They found cecal bascule and deserosalized cecum and performed right hemicolectomy and ileocolic anastomosis.
Diagnosis of cecal volvulus in pregnancy is challenging, often delayed, and intraoperatively confirmed.Citation1,Citation12,Citation16 Laboratory tests are neither specific nor sensitive but may suggest secondary complications following intestinal obstruction, such as fluid and electrolyte abnormalities. Imaging studies with plain abdominal film have a sensitivity of 95%.Citation9,Citation13 A typical “coffee bean” appears to be directed to the upper-left quadrant.Citation13 The mobile cecum can reach different locations in the abdomen, but the single most important radiographic finding is the presence of a large, dilated cecum.Citation11 However, physicians are reluctant to send pregnant patients to the radiology department because of the fear of the teratogenic potential of radiation on the developing fetus.Citation1,Citation12,Citation13 The fact that carcinogenic and teratogenic effects of radiation occur after 1 and 20 Rads, respectively, makes abdominal films the safest imaging modality for the diagnosis of cecal volvulus in pregnant women, provided that it is only 182 mRad, which is the total dose from the three abdominal films.Citation13 The effect of radiation exposure on the developing fetus also depends on the gestational age. As the gestational age advances, the fetus will be more resistant to radiation, especially during the second and third trimesters.Citation17 It is also evidenced that radiation doses of less than 10 Rads are safe during pregnancy.Citation17 Other imaging modalities, such as contrast studies, are also important for the diagnosis of volvulus. Abdominal CT revealed a classic “whirl sign” in the right abdomen. Furthermore, CT is excellent for localizing the site of obstruction and for early detection of ischemia and perforation despite the fact that it has more ionizing radiation than that of plain abdominal radiography images.Citation11 MRI is a superior diagnostic modality for any type of bowel obstruction due to its excellent soft tissue contrast, and it also avoids ionizing radiation. It is also the choice of imaging in most institutions for pregnant mothers for acute abdomen. The limitations are mainly long scanning times, high cost, and availability.Citation18 In low-resource areas where a plain abdominal film is not available and there is a strong clinical suspicion for intestinal obstruction, early surgical exploration is also both diagnostic and therapeutic. Considering the setup of our hospital and the condition of the patient, the authors believe that it was an appropriate decision to send this patient to radiography and diagnose this rare but morbid condition early, with typical imaging findings suggestive of cecal volvulus.
The management of cecal volvulus is mainly surgical in most cases, and the success of nonsurgical and non-resective techniques is dismal. Unlike sigmoid volvulus, cecal volvulus cannot be detorsed endoscopically.Citation3 Treatment is generally aimed at removing devitalized, non-viable tissue, untwisting the bowel if viable, decompressing the distended bowel segment, and ultimately reducing recurrence.Citation13,Citation16 In addition, management is highly influenced by intraoperative findings, whether ischemic or gangrenous with or without perforation, and hemodynamic status of the patient. Operative derotation, right hemicolectomy, cecopexy, and tube cecostomy are surgical options that we have whenever we approach such patient.Citation1 Right hemicolectomy is the preferred surgical option to fulfill these management goals. This significantly reduces recurrence rate.Citation1,Citation3,Citation11,Citation16 En-bloc resection of the volvulated segment of bowel together with a segment of the terminal ileum with end ileostomy or retention of bowel continuity with ileocolic anastomosis is highly dependent on the overall physiology of the patient. However, the mortality rate is high, ranging from 0% to 22%.Citation11
Non-resectional methods, provided that the cecum is viable, such as cecopexy, which involves anchoring the cecum to the parietal peritoneum in the right iliac fossa, are associated with increased recurrence 13–28.5%, with mortality rate steeping up to 18%.Citation11,Citation16 Cecostomy, a non-resectional technique, is performed by placing a tube into the distended cecum through a small incision on the cecal wall, the tube through the abdominal wall, and making a small incision on the skin. It has a decompressing effect on the significantly dilated cecum.Citation13,Citation16 This procedure has the disadvantage of subsequent leakage, either para-tubal or intra-peritoneal, due to difficulty in obtaining a secured suture through the edematous or atrophic tissue.Citation16 It also has a high recurrence rate compared to the above two techniques.
We did right hemicolectomy, since there were necrotic and non-viable parts of the involved bowel. In addition to this, there was a thinned-out and significantly dilated cecum. The bowel integrity was maintained with primary ileocolic anastomosis. Right hemicolectomy is the safest procedure for reducing recurrence during pregnancy, as the pregnancy state per se is a risk factor for cecal volvulus.
Conclusion
Cecal volvulus is a rare cause of intestinal obstruction with early vascular compromise and complicated obstruction. Pregnancy poses a particular risk factor by exaggerating the hypermobility state and challenging diagnosis, because the symptoms of presentation might be attributed to other diagnoses. A high index of suspicion and low threshold for requesting plain abdominal films or MRI, whenever the diagnosis is entertained is of paramount importance. Right hemicolectomy is the surgery of choice whenever cecal volvulus is diagnosed, with a mortality rate comparable to that of other non-resective methods but a significantly low or zero recurrence rates.
Abbreviations
SCARE, Surgical CAse Report; MRI, Magnetic Resonant Imaging.
Highlights
Intestinal obstruction is one of the life threatening causes of acute abdomen in pregnancy.
Cecal volvulus is a rare cause of intestinal obstruction.
Pregnancy poses a particular risk factor for the cecal volvulus.
Limited X-ray films are safe during pregnancy.
Right hemicolectomy is considered best surgical option as it eliminates the recurrence rate.
Ethical Approval
No institutional review board approval was required.
Informed Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent form is available for review by the Editor-in-Chief of this journal upon request.
Author Contributions
All authors contributed to the data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval or the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgment
Mursal Ibrahim, MD, Obstetrics and Gynecology resident, Department of Obstetrics and Gynecology, Jigjiga University, Ethiopia: involved in evaluation and management of the patient.
Data Sharing Statement
All the generated data are included in this article.
Additional information
Funding
References
- Narjis Y, Rabbani K, Largab S, Soumani A, Finech B, El Idrissi Dafali A. Coecal volvulus: an acute complication of pregnancy. J Emerg Trauma Shock. 2010;3(4):426–427. doi:10.4103/0974-2700.70771
- Coughlan B, O’herlihy C. Acute intestinal obstruction during pregnancy. J R Coll Surg Edinb. 1978;23(3):175–177.
- Charles Brunicardi F, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery. 11th ed. New York: McGraw Hill; 2019:2319.
- Hamlin E, Bartlett MK, Smith JA. Acute surgical emergencies of the abdomen in pregnancy. N Engl J Med. 1950;244(4):128–131. doi:10.1056/NEJM195101252440402
- Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A. The SCARE 2020 guideline: updating Consensus Surgical Case Report (SCARE) Guidelines. Int J Surg. 2020;84:226–230. doi:10.1016/j.ijsu.2020.10.034
- Wismayer R. Study about caecal volvulus in East Africa: a rare cause of bowel obstruction. Curr Pract Med Sci. 2022;10:133–141.
- Fekadu G, Tolera A, Beyene Bayissa B, Merga BT, Edessa D, Lamessa A. Epidemiology and causes of intestinal obstruction in Ethiopia: a systematic review. SAGE Open Med. 2022;10:20503121221083207. doi:10.1177/20503121221083207
- Sylvester KR, Ooko PB, Mwachiro MM, Parker RK. Cecal volvulus in rural Kenya: delayed presentation contributes to high mortality. BMC Surg. 2021;21(1):430. doi:10.1186/s12893-021-01416-8
- Perdue PW, Johnson HW, Stafford PW. Intestinal obstruction complicating pregnancy. Am J Surg. 1992;164(4):384–388. doi:10.1016/S0002-9610(05)80910-9
- Solis Rojas C, Vidrio Duarte R, García Vivanco DM, Montalvo-Javé EE. Cecal volvulus: a rare cause of intestinal obstruction. Case Rep Gastroenterol. 2020;14(1):206–211. doi:10.1159/000506933
- Gordon PH. Principles and Practice of Surgery for Colon, Rectum and Anus. 3rd ed. Nivatvongs S, editor. CRC Press; 2007:1330.
- Montes H, Wolf J. Cecal volvulus in pregnancy. Am J Gastroenterol. 1999;94(9):2554–2556. doi:10.1111/j.1572-0241.1999.01394.x
- Chihaka OB. Cecal volvulus in pregnancy: a case report. Cent Afr J Med. 2011;57(5–8):32–35.
- Draçini X, Dibra A, Celiku E. Cecal volvulus during pregnancy. Case report. G Chir. 2012;33(4):129–131.
- Kreinces J, Robbins AI, Kim DE. Cecal bascule in pregnancy: a case report and review of the literature. J Surg Case Rep. 2023;2023(5):rjad287. doi:10.1093/jscr/rjad287
- Madiba TE, Thomson SR, Church JM. The management of cecal volvulus. Dis Colon Rectum. 2002;45(2):264–267. doi:10.1007/s10350-004-6158-4
- Slesinger TL, Yoon I. Radiation Exposure in Pregnancy. Treasure Island (FL): StatPearls Publishing; 2023.
- Shen J, Teng X, Chen J, Jin L, Wang L. Intestinal obstruction in pregnancy-A rare presentation of uterine perforation. BMC Pregnancy Childbirth. 2023;23(1):507. doi:10.1186/s12884-023-05827-8
