 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
The aim of this study was to evaluate the impact of corneal cross-linking combined with photorefractive keratectomy (PRK) on blurring strength.
Methods
A total of 63 patients with keratoconus were recruited for this study, and two study groups were formed according to the therapeutic intervention: corneal collagen cross-linking (CxL) group (33 patients) received corneal cross-linking according to the Dresden protocol, while the rest additionally received topography-guided photorefractive keratectomy (tCxL). The impact of surgical procedure on blurring strength was assessed by power vector analysis. Potential association between blurring strength and vision-specific quality of life was assessed using the National Eye Institute Visual Function Questionnaire (NEI-VFQ) 25 instrument.
Results
Blurring strength presented excellent correlation with NEI-VFQ scores both preoperatively and postoperatively (all P<0.01). Both groups demonstrated nonsignificant changes in best-corrected visual acuity; however, only the tCxL group had significant reduction in blurring strength (13.48+10.86 [preoperative], 4.26+7.99 [postoperative], P=0.042).
Conclusion
Only the combined treatment (tCxL) resulted in significant reduction in blurring strength. Moreover, the excellent correlation of blurring strength with NEI-VFQ scores indicates its reliability as an index of self-reported quality of life in keratoconus, since it seems to address the nonsignificant changes in best-corrected visual acuity following CxL treatments that are conceived as subjective improvement by the patient.
Introduction
It is documented that keratoconus (KC) is associated with complex refractive errors that conventional refractive solutions (ie, spectacles or contact lenses) cannot fully address. In fact, KC’s complex refractive status is among the primary reasons for the overall reduction in visual capacity, even in the early stages of the disease.Citation1–Citation4 A series of methods have been proposed for the quantification of KC-associated refractive error in clinical settings. Among the prevalent ones is power vector analysis. Power vector analysis introduces a single measurable unit, the blurring strength (B), which is the outcome of the geometrical representation of spherocylindrical refractive errors in three fundamental dioptric components. The conceptual advantage of power vectors and especially of B is that as they simplify the changes in the optical characteristics of the eye due to either KC progress or a surgical intervention.Citation5–Citation7
Corneal collagen cross-linking (CxL) was recently developed in order to stabilize and strengthen the ectatic cornea by creating new covalent bonds between stromal collagen fibrils in the anterior 200–300 µm of the corneal stroma. Moreover, in an attempt to (partially) reverse KC’s impact on visual capacity, CxL has been combined with topography-guided photorefractive keratectomy (tCxL) with excellent results regarding safety and patients’ satisfaction.Citation8–Citation11
However, the additional beneficial impact of tCxL on the refractive status as reflected by power vectors has not been studied in clinical trials. Therefore, within this context, the primary objective of this study was to assess the impact of both CxL and tCxL on blurring strength in a sample of patients with KC. The objective of this study was to assess the correlation between (B) and vision-specific quality of life (VS-QoL) 5-list-item Greek version of the National Eye Institute Visual Function Questionnaire (NEI VFQ-25).Citation12
Patients and methods
Setting
This study was a prospective, observational, nonrandomized trial (ClinicalTrials.gov Identifier: NCT01527721). The study adhered to the tenets of the Declaration of Helsinki, and written informed consent was given by all participants. The institutional review board of the Democritus University of Thrace approved the protocol, and the study was conducted at the Eye Institute of Thrace, Alexandroupolis, Greece.
Participants
Patients with KC were recruited from the Outpatients Cornea service of the Eye Institute of Thrace, and two study groups were formed which are as follows: 1) tCxL (study) group and 2) CxL (control) group. All participants with KC with progressive KC in consecutive corneal topographies and changes in the refractive power had to present. Exclusion criteria included glaucoma, suspicion for glaucoma, intraocular pressure-lowering medications, central corneal thickness <400 µm, K-readings >60 D, history of herpetic keratitis, corneal scarring, severe eye dryness, pregnancy or nursing, current corneal infection, or underlying autoimmune disease. The tCxL group participants underwent combined tCxL with CxL, while the CxL group underwent standard CxL treatment according to the Dresden protocol. In order to be eligible for the tCxL group, participants should have central corneal thickness >450 µm.
Surgical procedure
The same surgical procedure was applied to all the patients with KC, which included instillation of proparacaine hydrochloride 0.5% drops (Alcaine®; Alcon, Inc., Hünenberg, Switzerland) for topical anesthesia, application of a sponge saturated with 10% alcohol to the central cornea for 30 seconds, and subsequent de-epithelialization by means of a hockey knife. Following de-epithelialization, a mixture of 0.1% riboflavin in 20% Dextran solution was instilled into the cornea for 30 minutes (two drops every 2 minutes) prior to the irradiation, until the stroma was completely penetrated and aqueous was stained yellow. The ultraviolet (UV) radiation source was UV-XTM (IROC AG, Zürich, Switzerland). In detail, an 8.0 mm diameter of central cornea was irradiated for 30 minutes by ultraviolet A (UVA) light with a wavelength of 370 nm and an irradiance of 3 mW/cm2. Instillation of riboflavin drops (one drop every 2 minutes) was continued during the irradiation, as well, in order to sustain the necessary concentration of the riboflavin. Moreover, balanced salt solution was applied every 6 minutes to moisten the cornea.
For the tCxL group, tCxL preceded the CxL. The epithelium was mechanically removed with a hockey knife, and ablation was performed in a 9.0 mm zone with a maximal intended depth of 50 µm. No adjuvant Mitomycin-C was applied in any case. For the photorefractive ablation, we used the Allegretto Wave 200 Hz (1.0071-1-0.81/1.208 software/WaveLight Laser Technologie, AG, Erlangen, Germany) with the T-CAT® ablation profile.
Postoperative management
After treatment, all patients were prescribed topical ofloxacin 0.3% drops qid (Exocin; Allergan, Inc., Irvine, CA, USA) and fluorometholone qid (Flucon; Alcon, Inc.), accompanied by frequent instillation of artificial tears (Tears Naturale II, Alcon, Inc.). Soft therapeutic lens was applied until complete re-epithelialization of the cornea was detected. Follow-up visits were performed on the first day, seventh day, first month, third month, sixth month, and 12th month after the operation.
Data collection
Regarding Scheimpflug camera (Pentacam Classic; OCU-LUS Optikgerate GmbH, Heidelberg, Germany; software version 1.14r04) measurements, acceptable maps had at least 10.0 mm of corneal coverage. Moreover, images with extrapolated data in the central 9.0 mm zone were excluded. Regarding the measuring procedure itself, patients were asked to blink and then look at the fixation device. In the case of low-quality image, the procedure was repeated until the acceptable criteria were met.
The impact of the surgical technique (either CxL or tCxL) on spherocylindrical error was evaluated by power vector analysis as described earlier.Citation6,Citation13 Power vectors are a geometrical representation of spherocylindrical refractive errors in three fundamental dioptric components. Manifest refractions comprising sphere (S), cylinder (C), and axis (φ) were converted into three dioptric powers (M, J0, and J45). Moreover, we calculated the overall blurring strength (B) of the spherocylindrical error by measuring the length of the produced vectorCitation14,Citation15 derived by the following formulas:
(1)
(2)
(3)
VS-QoL was obtained for all participants using the NEI VFQ-25. All data for analysis were obtained at the last follow-up visit.
Statistical analysis
Normality of the measured data was assessed using Kolmogorov–Smirnov test, and parametric or nonparametric tests were applied, as necessary. An a priori power analysis was performed. For an effect size of 0.74, 30 participants would be required in each group for the study to have a power of 0.8 at the significance level of 0.05. All statistical analysis was performed using the MedCalc statistical program (version 9.6.2.0; MedCalc Software, Mariakerke, Belgium).
Results
A total of 63 patients (29 females and 34 males) with progressive KC were included in the study. Of them, 33 patients underwent CxL treatment (CxL group), while the remaining 30 patients underwent combined CxL and tCxL (tCxL group). According to , study groups presented nonsignificant differences in age, best-corrected visual acuity (BCVA), defocus equivalent, mean power vectors, blurring strength, and subjective assessment of VS-QoL (P=0.404). Moreover, VS-QoL scores demonstrated excellent correlation with blurring strength for both study groups (CxL: R2: 0.679; tCxL: R2: 0.654, P<0.001).
Table 1 Preoperative patient characteristics
Regarding the impact of CxL and tCxL on spherocylindrical error (), power vector analysis indicated that tCxL reduced blurring strength (13.48+10.86 [preoperative], 4.26+7.99 [postoperative], P=0.042) primarily due to the reduction in the M component (−3.55+2.32 [preoperative], −1.30+2.67 [postoperatively], P=0.043). On the other hand, nonsignificant impact on the overall blurring strength could be detected in the CxL group, despite changes in the J0 component (P=0.418). Blurring strength continued to demonstrate excellent association with NEI-VFQ 25 scores (); however, R2 values were slightly reduced when compared to preoperative ones. Moreover, both groups had a significant improvement in VS-QoL (tCxL: 91.07±13.11, P<0.001; CxL: 89.95±15.68, P=0.045); however, a significant difference could be detected in VS-QoL postoperative intergroup comparison, as well (P=0.012). The latter finding suggests that the tCxL group perceives better the beneficial impact of the corresponding surgical technique.
Figure 1 Correlation chart of blurring strength and total NEI-VFQ 25 score for the tCxL group.
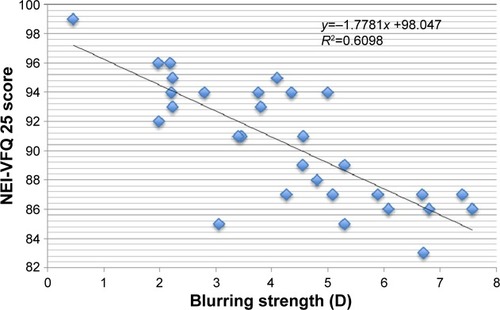
Table 2 Postoperative clinical data
Discussion
CxL treatment has been proven to be an effective therapeutic approach for progressive KC, leading to stabilization of corneal ectasia by enhancing corneal rigidity.Citation16–Citation18 However, the technique aims in the stabilization of the progressive ectasia and does not address any preexisting poor visual performance due to the high irregularity of the ectatic cornea. Therefore, a series of refractive therapeutic techniques were combined with CxL in an attempt to address both the progression and the underlying complex refractive error. Among these combined treatments are: CxL combined with intracorneal ring segments,Citation19,Citation20 CxL combined with conductive keratoplasty,Citation21 and CxL combined with PRK.Citation22,Citation23 Recently, CxL was combined with both intracorneal rings and PRK.Citation24
In fact, the tCxL component of the combined CxL-PRK treatment only partially addresses the complex refractive error, primarily due to the limitations of the preoperative pachymetry,Citation25,Citation26 the necessary residual bed for safe CxL,Citation27 and eventually due to the fact that specific guidelines are yet to be introduced. Despite these limitations, recent studies indicated the additional beneficial impact over conventional CxL in terms of visual recovery and subjective improvement in the quality of vision.Citation10,Citation11,Citation23
Further to the prevalent indexes of visual performance (ie, UVA, BCVA, and spherical equivalent) which are frequently used in CxL studies, we attempted to explore the impact of CxL and CxL combined with PRK on blurring strength. It is known that power vector analysis is an efficient method for evaluating refractive surgery outcomes with the transformation of manifest and topographic refractions into power vectors. Power vectors allow us to directly evaluate the impact of an intervention on refraction by mathematically comparing the impact on its independent components (M, J0, J45).Citation5–Citation7 Regarding our study, all participants underwent either CxL or combined CxL with tCxL treatments, with no signs of disease progression for the first year of follow-up. Moreover, both groups presented nonsignificant improvement in BCVA. Therefore, in clinical terms, both treatments were considered satisfactory. However, tCxL participants experienced an additional significant reduction in blurring strength and improvement in UVA that CxL participants did not. The clinical importance of this finding is that even though tCxL targets to a maximal depth of 50 µm and cannot address the underlying refractive error as a whole, it has a significant beneficial impact on blurring strength, since the latter is comprised by the square root of the powers of the individual components (M, J0, J45). In simple words, minor treatment changes of the axis and power of astigmatism and of the spherical component induce major changes on the blurring strength.
Former publications from our group indicated the significant beneficial impact of CxL (either stand-alone CxL or combined with tCxL) on self-perceived, VS-QoL.Citation10,Citation23 In this study, we confirmed the former results; moreover, we identified blurring strength as an excellent index of the efficacy of both approaches (CxL and tCxL) since it demonstrated excellent correlation with NEI-VFQ scores. Our findings are consistent with former studies that identified dioptric blur’s impact on reading ability and contrast sensitivity.Citation28 Within this context, the prospective clinical usefulness of blurring strength in tCxL treatments becomes apparent. Preoperative calculation of the potential postoperative blurring strength provides essential information regarding the exact parameters of an individualized tCxL treatment of an ectatic cornea aiming primarily to improved VS-QoL scores. The fact that BCVA remained unaffected in both study groups suggests that conventional correction methods such as spectacles or contact lenses addressed the remaining refractive error. However, clinical experience suggests that patients with KC tend to develop intolerance especially after chronic use of semi-hard or hard contact lenses and nonspecific disturbances in spectacle corrections.Citation29 Therefore, any possible improvement in the dioptric blur during the surgical management of patients with KC should be attempted in order to minimize poor visual performance if or when conventional correction methods fail in the future due to intolerance.
Conclusion
In summary, to our knowledge, this is the first study to report on the effect of CxL and CxL combined with tCxL on the blurring strength. Moreover, it is the first study to explore the excellent association between blurring strength and self-perceived quality of life in patients with KC. Our results suggest that tCxL’s beneficial impact on blurring strength is significant; therefore, the treatment should be delivered immediately when progression is established and safety issues are resolved. Moreover, preoperative calculation of blurring strength could be a valuable adjuvant index for the PRK in combined treatments.
Disclosure
The authors report no conflicts of interest in this work.
References
- CampsVJPiñeroDPCaravaca-ArensEde FezDPérez-CambrodíRJArtolaANew approach for correction of error associated with keratometric estimation of corneal power in keratoconusCornea201433996096725090162
- PiñeroDPAlióJLAlesónAEscafMMirandaMPentacam posterior and anterior corneal aberrations in normal and keratoconic eyesClin Exp Optom200992329730319243389
- PiñeroDPCampsVJCaravaca-ArensEPérez-CambrodíRJArtolaAEstimation of the central corneal power in keratoconus: theoretical and clinical assessment of the error of the keratometric approachCornea201433327427924452214
- RavikumarAMarsackJDBedellHEShiYApplegateRAChange in visual acuity is well correlated with change in image-quality metrics for both normal and keratoconic wavefront errorsJ Vis201313132
- BlendowskeRUnaided visual acuity and blur: a simple modelOptom Vis Sci2015926e121e12525955640
- ThibosLNHornerDPower vector analysis of the optical outcome of refractive surgeryJ Cataract Refract Surg2001271808511165859
- ThibosLNWheelerWHornerDGPower vectors: an application of Fourier analysis to the description and statistical analysis of refractive errorOptom Vis Sci1997743673759255814
- ParkerJSvan DijkKMellesGRTreatment options for advanced keratoconus: a reviewSurv Ophthalmol201560545948026077628
- RandlemanJBKhandelwalSSHafeziFCorneal cross-linkingSurv Ophthalmol201560650952325980780
- LabirisGGiarmoukakisASideroudiHGkikaMFanariotisMKozobolisVImpact of keratoconus, cross-linking and cross-linking combined with photorefractive keratectomy on self-reported quality of lifeCornea201231773473922236781
- Ortiz-ToqueroSPerezSRodriguezGde JuanVMayo-IscarAMartinRThe influence of the refractive correction on the vision-related quality of life in keratoconus patientsQual Life Res2015 Epub201593
- LabirisGKatsanosAFanariotisMPsychometric properties of the Greek version of the NEI-VFQ 25BMC Ophthalmol20088418325083
- LabirisGGatzioufasZGiarmoukakisASideroudiHKozobolisVEvaluation of the efficacy of the Allegretto Wave and the Wavefront-optimized ablation profile in non-anterior astigmatismsActa Ophthalmol2012906e442e44622690672
- HarrisWFDioptric strength: a scalar representation of dioptric powerOphthalmic Physiol Opt1994142162188022607
- RaaschTWSpherocylindrical refractive errors and visual acuityOptom Vis Sci1995722722757609953
- WollensakGSpoerlESeilerTRiboflavin/ultraviolet-A–induced collagen crosslinking for the treatment of keratoconusAm J Ophthalmol200313562062712719068
- WollensakGCross inking treatment of progressive keratoconus: new hopeCurr Opin Ophthalmol20061735636016900027
- Wittig-SilvaCWhitingMLamoureuxELindsayRGSullivanLJSnibsonGRA randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary resultsJ Refract Surg2008247720725
- El-RaggalTMSequential versus concurrent KERARINGS insertion and corneal collagen cross-linking for keratoconusBr J Ophthalmol2011951374120584709
- SaelensIEBartelsMCBleyenIVan RijGRefractive, topographic, and visual outcomes of same-day corneal cross-linking with Ferrara intracorneal ring segments in patients with progressive keratoconusCornea201130121406140821993465
- KymionisGDKontadakisGANaoumidiTLKazakosDCGiapitzakisIPallikarisIGConductive keratoplasty followed by collagen cross-linking with riboflavin-UV-A in patients with keratoconusCornea201029223924320023583
- KanellopoulosAJAsimellisGKeratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens protocol)J Refract Surg2014302889324763473
- LabirisGGiarmoukakisASideroudiHKozobolisVImpact of keratoconus, cross-linking and cross-linking combined with photorefractive keratectomy on self-reported quality of life: a 3-year updateCornea2013329e186e18823807006
- IovienoALégaréMERootmanDBYeungSNKimPRootmanDSIntracorneal ring segments implantation followed by same-day photorefractive keratectomy and corneal collagen cross-linking in keratoconusJ Refract Surg2011271291591822074467
- KruegerRRKanellopoulosAJStability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reportsJ Refract Surg20102610S827S83220954679
- KymionisGDPortaliouDMKounisGALimnopoulouANKontadakisGAGrentzelosMASimultaneous topography-guided photorefractive keratectomy followed by corneal collagen cross-linking for keratoconusAm J Ophthalmol2011152574875521794846
- SpoerlEHoyerAPillunatLERaiskupFCorneal cross-linking and safety issuesOpen Ophthalmol J20115141621399770
- ChungSTJarvisSHCheungSHThe effect of dioptric blur on reading performanceVision Res200747121584159417442363
- DanaMRPutzJLVianaMASugarJMcMahonTTContact lens failure in keratoconus managementOphthalmology1992998118711921513569
