Abstract
Collagen cross-linking (CXL) is a relatively new conservative approach for progressive corneal ectasia, which is able to strengthen corneal tissue reforming new covalent bonds. Subjective and objective results following this method seem to be promising. In recent years, newer CXL protocols have been developed to perform more effective and less invasive procedures. The increasing diffusion of CXL in the corneal ectatic disease has increased the need to have actual indices regarding the efficacy of the treatment. Evaluation of demarcation line (DL), a transition zone between the cross-linked anterior corneal stroma and the untreated posterior corneal stroma, is considered a measurement of the depth of CXL treatment into the stroma. Some evidence in the literature emphasize that DL could be a measure of effectiveness of the CXL. On the contrary, some authors believe that the “the deeper, the better” principle is rather a simplistic approach for interpreting the clinical importance of the corneal stromal DL.
Introduction
Keratoconus is one of the leading causes of cornea transplant. Therapies based on the spectacles and contact lenses do not hinder the progression of the disease. Surgeries and corneal transplantation, though preserved as the first choice for the severe variants of the disease, have risks such as rejection of the transplanted cornea. Corneal cross-linking (CXL) is a noble strategy based on the underlying pathology of the disease. The main indication for CXL is to slow the progression of corneal ectatic diseases, such as keratoconus, pellucid marginal degeneration (PMD), and keratoglobus.Citation1,Citation2 In addition to these primary forms, there also exist forms related to refractive surgery.Citation3
Studies on keratoconus epidemiology reported an incidence of 1.3–22.3 cases per 100,000 and a prevalence of 0.4–86 cases per 100,000.Citation4 The incidence of keratectasia after laser in situ keratomileusis (LASIK) has been reported to be 0.04%–0.6%.Citation5–Citation7 Keratoconus is a progressive noninflammatory disease of the cornea distinguished by para-central corneal thinning and ectasia, resulting in irregular astigmatism with impaired vision. In most cases, it is bilateral but often asymmetrical and it usually begins sometime in puberty and it progresses until the fourth decade, when the corneal shape generally becomes stable.Citation8 The etiology of keratoconus is unknown including genetic, biochemical, and physical factors. There is no unique theory elucidating its range of clinical appearances, and it is probable that keratoconus is the manifestation for several different conditions. It usually appears as an isolated disease, but it has been associated with a number of ocular and systemic pathologies, including vernal disease, retinitis pigmentosa, blue sclera, atopy, magnesium deficiency, Down’s syndrome, Turner syndrome, and connective tissue disorders such as Marfan’s syndrome, Ehlers–Danlos syndrome, osteogenesis imperfecta, and pseudoxanthoma elasticum.Citation9 Genetic factors have an incidence of up to 10%.Citation10 In keratoconus corneas, the protease enzymes are upregulated while the activities of protease inhibitors are inhibited, involving an increasing digestion of stromal proteins with a consequent reduction in the biomechanical stability and corneal thinning.Citation11,Citation12 In diabetic patients, the severity of the pathology is inversely proportional.Citation13 Corneal alterations in keratoconus involve changes in basement membrane structure, stromal collagen fiber, morphology of keratocytes, and abnormal cell–matrix interactions.Citation14
Posterior keratoconus is a rare corneal anomaly, which is characterized by a total or localized noninflammatory thinning of the posterior stroma and a depression of the posterior corneal surface, whereas the anterior surface remains more regular.Citation15
Less common than keratoconus is PMD, which usually affects the para-central and the inferior peripheral cornea in ∼85% of cases, while the superior peripheral cornea in remaining 15%. It is a progressive noninflammatory disorder characterized by a band of thinning that usually involves the cornea between 4 o’clock and 8 o’clock positions, ie, 1 mm from the limbus. The etiology of PMD is not known. Corneal topography shows the typical “butterfly pattern” of an irregular astigmatism with a marked flattening along a vertical axis and a steepening of the inferior cornea.Citation2,Citation16
Corneal CXL
Corneal CXL with riboflavin and ultraviolet A (UV-A) is a technique to strengthen corneal tissue using riboflavin as a photosensitizer and UV-A to increase the formation of intra- and interfibrillar covalent bonds by photosensitized oxidation. This technique is able to flatten corneal steepening, stabilize the cornea, and reduce the refractive error improving the irregular astigmatism.Citation17 Several studies confirm the effectiveness and safety of conventional cross-linking procedure, which is also known as “Dresden protocol”,Citation18–Citation21 in which the interaction between 0.1% riboflavin molecules absorbed in corneal tissue and UV-A rays delivered at 3 mW/cm2 for 30 minutes (5.4 J/cm2 energy dose) releases reactive oxygen species that promote the formation of “molecular bridges” between and within collagen fibers.Citation17,Citation22
Riboflavin (vitamin B2), because of its alkylisoalloxazine structure, allows the absorption of a wide range of light spectrum, including an absorption peak in UV-A range, so it is the standard photoinducer in cross-linking. An effective cross-linking requires a considerable corneal absorption of riboflavin; therefore, the epithelium debridement in standard protocols (epithelium-off [epi-off] CXL) has the goal of overcoming the barrier formed by corneal epithelium tight junctions that would limit the penetration of macromolecule as vitamin B2 (molecular weight: 376.37 g/mol).Citation23 However, the epithelium debridement is not free from complications, where there is an increased risk of ulcers, infections, haze, scarring, infiltrates, longer recovery time, patient discomfort, and postoperative pain.Citation24 Thus, some effort has been put into the development of transepithelial (epithelium-on, epi-on) CXL. Since riboflavin cannot penetrate intact corneal epithelium due to its chemical properties, different strategies were studied to enhance transepithelial riboflavin penetration, such as increasing riboflavin imbibition time and new riboflavin solution formulations to facilitate its transepithelial penetration.
Therefore, some substances, such as benzalkonium chloride, ethylenediaminetetraacetic acid, and trometamol, were used to enhance the epithelial penetration of riboflavin with good results, allowing a transepithelial CXL. This technique was safe and effective especially in ultrathin keratoconic corneas (pachymetry <400 µm), to avoid CXL cytotoxic effect on endothelium, crystalline lens, and other intraocular tissue.Citation25 In fact, in transepithelial CXL, the epithelium acts as a UV filter because of the high absorption coefficient; in the absence of a photosensitizer, UV-A light at wavelengths of 350 nm and irradiance of 3 mW/cm2 would not cause significant cytotoxicity. The addition of riboflavin reduces the damage threshold compared with UV-A light alone and produces oxygen-free radicals inducing CXL.
In recent years, to perform less invasive procedures, attention has focused on the possibility to create new protocols to minimize UV exposure duration, reduce postoperative discomfort, and further decrease the complication rate.Citation3 In this direction, the accelerated, high-fluence CXL arises, based on the principle of photochemical reciprocity, known as the law of Bunsen–Roscoe, which states that in a system the same photochemical effect can be achieved through reduced irradiation interval while maintaining a constant total energy level by an increase in irradiation intensity.Citation26,Citation27
Ocular iontophoresis is a noninvasive protocol that uses the ions flow in an electric field to apply the negatively charged riboflavin within the stroma through the corneal epithelial barrier. In the most recent CXL protocols, it is a well-known method investigated to enhance the penetration of photosensitizer in the stroma. It has been evidenced that by using iontophoresis, a 5-minute imbibition achieves a sufficient riboflavin concentration in the corneal stroma for CXL treatment, preserving epithelial integrity.Citation28 Several ex vivo studies confirmed the effectiveness of iontophoresis imbibition in obtaining an adequate riboflavin concentration into the stroma and the induction of evident biomolecular and structural changes of the treated corneas.Citation29 To reduce the administration time, UV-A irradiation protocols that are different from the standard technique (3 mW/cm2 for 30 minutes) can be used. Literature shows, in ex vivo experiments, a similar increase in corneal biomechanical stiffness using 10 mW/cm2 illumination intensity for 9 minutes and the standard protocol (3 mW/cm2 for 30 minutes).Citation30 Preliminary clinical results of iontophoresis-assisted transepithelial (I-CXL) are very promising, reducing or blocking the progression of keratoconus without significant complications.Citation31,Citation32
CXL combined with other treatments
Corneal cross-linking has been used in combination with other treatments in keratoconic eyes and post-laser ectasia to optimize visual outcomes. Combined CXL and limited topography-guided photorefractive keratectomy in selected eyes with moderate ectasia and adequate corneal thicknesses have been evidenced to be effective with improvements in visual, refractive, and topographic data and stabilization of the ectatic disease in many eyes.Citation33–Citation35 Such different treatment modalities have been reported to be associated with significant improvements in the quality of life. However, the follow-up in these studies is limited to 1–3 years so that the long-term results are not known. In addition, significant corneal haze/scarring has been reported.Citation36 CXL has also been combined with intracorneal ring segment insertion, suggesting a potential additional effect of CXL.Citation37,Citation38 The transepithelial iontophoresis CXL has also been used in the treatment of PMD associated with sliding keratoplasty, proving to be safe and effective in the treatment of advanced PMD.Citation39
CXL has also been associated with refractive procedures such as photorefractive keratectomy and LASIK to improve the long-term stability and to reduce the possible occurrence of postoperative ectasia. Up to now, such studies are very limited in terms of eyes treated, efficacy, and long-term follow-up, although a study in CXL after hyperopic LASIK demonstrated less regression of refractive effects over the follow-up period.Citation40
Demarcation line
After corneal CXL in keratoconic eyes, some confocal microscopic studies evidenced edema, rarefaction of keratocytes in the anterior and mid-stroma, nerve loss, and focal endothelial changes in the immediate postoperative period ().Citation41–Citation43 Ultrastructural study shows that changes in stromal keratocytes with cell and collagen fiber shrinkage, chromatin condensation, and apoptotic bodies are detectable within 60 minutes after UV-A–riboflavin treatment.Citation44 In the excited state, post UV-A exposure, riboflavin can produce radicals or singlet oxygen molecules that induce covalent bonds that can connect one polymer chain to another, causing in vivo cornea links in collagen fibers.Citation45 Photochemically induced cross-links in cornea can be detected through structural changes secondary to CXL. Ex vivo studies evidence an increased resistance to enzymatic degradation processes involved in progressive thinning of the cornea in keratoconus. Corneas that underwent CXL treatment present an inferior rate of enzymatic collagenasic degradation when compared with an untreated cornea. Corneal CXL acts unevenly within the corneal thickness; UV-A intensity is inversely proportional to deepening in stromal tissue for several reasons; and primarily riboflavin concentration decreases linearly with increasing of corneal depth, in accordance with diffusion gradient. Furthermore, according to Lambert–Beer law, 65% of UV radiation is absorbed in the first 200 µm. The consequence of a higher UV intensity in anterior cornea is a greater stiffening effect within first 250 µm.Citation28
Table 1 Comparative findings of corneal stromal DL depth after CXL
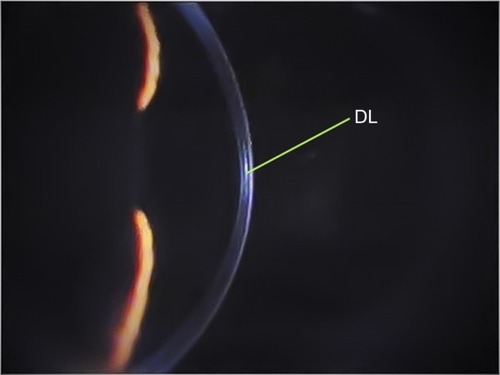
Corneal cross-linking causes a dose-dependent keratocytes damage. Wollensak et alCitation46 described cellular apoptosis to a depth of 300 µm radiating with UV-A at 3 mW/cm2. Histopathological studies showed an already complete keratocyte apoptosis limited to the anterior stroma within 24 hours.Citation46 An increased density of the extracellular matrix was evidenced to a depth of 300–350 µm. By using the slit-lamp examination, this appears as a “demarcation line” (DL), a transition zone between the cross-linked stroma and untreated tissue, which can be seen as early as 2 weeks (). It is an area of hyper-reflectivity due to different refractive indices or reflective properties of cross-linked vs untreated corneal stroma. Some authors characterized the corneal stromal DL as a clinical sign to evaluate the depth of the CXL treatment.Citation47,Citation48
Figure 1 Biomicroscopic image of keratoconus eye at slit lamp 6 months after epi-off standard corneal CXL.
Abbreviations: CXL, collagen cross-linking; DL, demarcation line; epi-off, epithelium-off.
Some studies hypothesize the role of the DL after CXL depth as representative of CXL effectiveness.Citation49–Citation51 Recently, the essential debate focused on whether the depth of the corneal stromal DL is indeed a true indicator of CXL efficacy. The main question is whether “the deeper, the better” principle can be applied to CXL. Actually, other confounding factors may interfere with the clinical interpretation of the depth of corneal DL after CXL. Therefore, some authors believe that the “the deeper, the better” principle is rather a simplistic approach for interpreting the clinical importance of the corneal stromal DL.Citation52
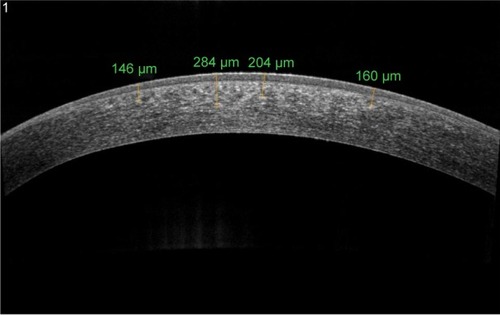
In recent years, anterior segment optical coherence tomography (AS-OCT) and confocal microscopy have been used as tools to assess the depth of DL and consequently the depth of the cross-linking effect (). Kymionis et alCitation53 compared the depth of stromal DL using both AS-OCT and confocal microscopy studying the transition area between the cellular and acellular zone, thereby showing no statistical significant differences between the two measurements.
Figure 2 AS-OCT of keratoconus eye 6 months after epi-off corneal cross-linking radiating with UV-A at 3 mW/cm2.
Abbreviations: AS-OCT, anterior segment optical coherence tomography; DL, demarcation line; epi-off, epithelium-off; UV-A, ultraviolet A.
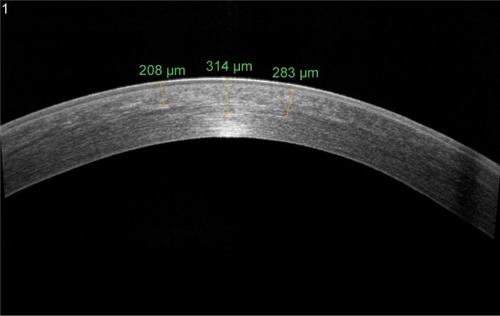
By using the AS-OCT, the stromal DL is detected within an enhanced image of the cornea in the horizontal meridian. The image is captured when the corneal reflex is visible, and the depth of DL is measured using the caliper tool provided by the manufacturer.
Doors et al described the best visibility of corneal stromal DL using AS-OCT at 1 month after CXL treatment, with an average DL depth of 313 µm; Yam et al measured the depth of DL at 6 months highlighting that the severity of ectasia and age may cause a worse DL visibility.Citation49,Citation51
A characteristic DL depth pattern, deeper centrally than peripherally has been observed in different studies; this is probably due to the top-hat beam profile of UV-A optical system that does not compensate for natural corneal curvature, so the UV-A beam enters the cornea at a non-orthogonal angle in the corneal periphery ().Citation54
DL in accelerated epi-off CXL
Corneal stromal DL after CXL using both the standard Dresden protocol (30 minutes with 3 mW/cm2) and a modified accelerated protocol (14 minutes with 9 mW/cm2) was evaluated according to the photochemical law of reciprocity (Bunsen–Roscoe law). There was no statistically significant difference in corneal stromal DL depth between the two groups, with a mean depth of 337 µm in the first group and 322 µm in the second group.Citation55 However, Kymionis et al evaluated the corneal stromal DL depth after very high-intensity (18 mW/cm2) UV-A irradiation for a 5-minute collagen CXL. Despite the easy identification of DL using AS-OCT, it seemed to be shallower when compared with the previously described 10-minute protocol and standard Dresden protocol ().Citation48,Citation56
Figure 3 AS-OCT of keratoconus eye 6 months after accelerated epi-off corneal cross-linking radiating with UV-A at 10 mW/cm2.
Abbreviations: AS-OCT, anterior segment optical coherence tomography; DL, demarcation line; epi-off, epithelium-off; UV-A, ultraviolet A.
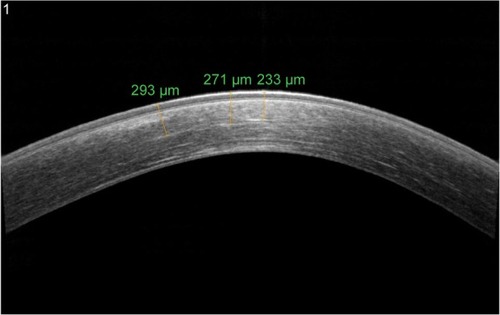
This confirms Shetty et al’sCitation57 findings comparing the clinical effect and DL using four different protocols; they have noticed the presence of a DL at a depth of 280±47 mm in 3 mW/cm2 irradiation for the 30-minute group, 292±73 µm in 9 mW/cm2 for the 10-minute group, 203±36 µm in 18 mW/cm2 for the 5-minute group, and 201±82 µm in 30 mW/cm2 for the 3-minute group. A deeper and well-defined DL was found in the 3 mW/cm2 and 9 mW/cm2 groups. However, a patchy and an incomplete DL was noted in the higher intensity groups.
Bunsen–Roscoe law may be valid for the certain dose range, meaning that corneal cross-linking effect may depend on a threshold that the increase in the illumination intensity is limited up to 40–45 mW and the decrease in the illumination time is limited from 30 minutes to 2 minutes.
However, no statistically significant increase can be achieved for higher intensities ranging from 50 mW to 90 mW (illumination times of <2 minutes) probably due to complex biochemistry that is not completely understood until now. As the anterior stroma is more important in terms of biomechanical stability of the cornea, despite a significantly less DL depths after accelerated CXL, the cross-linking effect may also be strong enough to stop the progression of corneal ectasia which however must be validated by future long-term clinical studies.Citation58
Kymionis et alCitation56 suggested that Bunsen–Roscoe law of reciprocity may not directly apply to CXL in living corneal tissue; thus, an increased total energy dose should probably be applied to the keratoconic cornea to achieve a treatment effect comparable with the already proven effective standard Dresden CXL protocol.
A study using confocal microscopy and AS-OCT after epi-off pulsed light (1 second on/1 second off) accelerated collagen cross-linking (PL-ACXL) and epi-off continuous light accelerated collagen cross-linking (CL-ACXL) evidenced a deeper DL in the PL-ACXL group. This could be probably due to an additional oxygen re-diffusion during pauses allowing more singlet oxygen release for the cross-linking of collagen molecules.Citation59 Moramarco et alCitation50 showed a mean depth of DL of 149 µm in the CL-ACXL group and 213 µm in the PL-ACXL group noting the importance of performing AS-OCT no later than 1 month after CXL to obtain the most accurate measure of the depth of DL.
Oxygen is essential for the photochemical polymerization reaction in CXL and is probably the limiting factor; it is theoretically possible that increasing fluence in an attempt to accelerate photopolymerization will not allow sufficient time for oxygen to diffuse and participate in the reaction, limiting the procedure.Citation60
DL in transepithelial epi-on CXL
Transepithelial CXL with substances such as benzalkonium chloride, ethylenediaminetetraacetic acid, and trometamol to enhance the epithelial permeability of riboflavin has been developed as an alternative technique for thin corneas.Citation25 In epi-on CXL, OCT analysis after 2 weeks of CXL treatment shows a dense area in the corneal stroma (not present before CXL) that was linear in shape and positioned ∼100 µm from the corneal epithelial layer, slightly beneath Bowman’s membrane (). These observations appear to highlight the possible role of the epithelium (also containing riboflavin) in shielding UV light.Citation61 It is unclear whether the shallower DL using the epi-on approach is due to the limited penetration of riboflavin into the stroma, or it is a result of reduced UV-A light penetration by shielding from riboflavin-impregnated intact corneal epithelium.Citation62
Figure 4 AS-OCT of keratoconus eye 6 months after epi-on corneal cross-linking radiating with UV-A at 3 mW/cm2.
Abbreviations: AS-OCT, anterior segment optical coherence tomography; DL, demarcation line; epi-on, epithelium-on; UV-A, ultraviolet A.
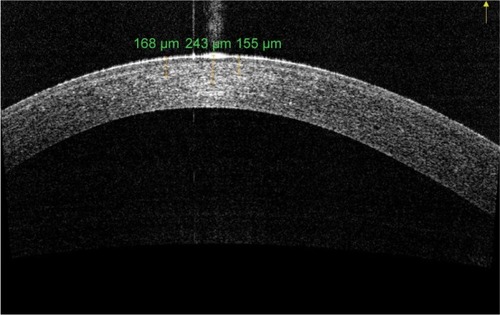
Bottos et alCitation63 recognized the cause of different corneal stromal DL depth in decreased penetration of riboflavin into the stroma rather than the result of reduced UV-A light penetration through epithelium barrier. Furthermore, biomechanical effects of corneal CXL are closely related to oxygen supply, and the intact epithelium acts as a barrier to rapid oxygen diffusion into the corneal stroma and results in suboptimal cross-linking. These findings underscore, at a clinical level, the importance of corneal tissue oxygenation for effective CXL, as suggested by Richoz et al.Citation60
DL in transepithelial epi-on iontophoresis CXL
I-CXL, when compared with transepithelial CXL, increases the penetration of riboflavin through intact epithelium enhancing the stromal amount of riboflavin while reporting lower photosensitizer amounts rather than standard epi-off protocols.Citation32
I-CXL creates a DL that can be visualized with AS-OCT, which seems less easily distinguishable and shallower than in conventional CXL, with a particular OCT appearance (). However, its depth and visualization seem to be more similar to conventional CXL than transepithelial CXL.Citation64 Confocal microscopy noted loss of keratocytes in the anterior and intermediate corneal stroma. DL was detected, ∼150–210 µm, in the I-CXL group with a characteristic pattern of “honeycomb” structure, which was less homogeneous compared with standard CXL. Bikbova and BikbovCitation65 evidenced that a DL was not clearly measurable over time in patients who underwent I-CXL. They showed that a DL was observed in only 45% patients 1 month after transepithelial I-CXL and was completely absent in all these patients for 3 months post CXL. Vinciguerra et alCitation32 described that, as in I-CXL, it is possible to detect an increase in reflectance in AS-OCT scans; however, no DL was visible and this finding could be explained by either the different concentration gradient induced by iontophoresis or a reduced CXL effect. Zhang et alCitation66 showed that the epithelial cells are not enriched with riboflavin. For this reason, only a small part of the UV light should be absorbed by the epithelium (∼15%–20%).
Figure 5 AS-OCT of keratoconus eye 6 months after epi-on corneal cross-linking with iontophoresis imbibition radiating with UV-A at 10 mW/cm2.
Abbreviations: AS-OCT, anterior segment optical coherence tomography; DL, demarcation line; epi-on, epithelium-on; UV-A, ultraviolet A.
Conclusion
Corneal cross-link is a strategy based on the underlying pathology of the corneal ectatic diseases. After corneal CXL procedures, a stromal DL can be observed within the corneal stroma at 1 month postoperatively. It would be unreasonable to disagree with the interpretation of the depth of DL as an indirect measurement of CXL penetration within the stroma, but the current knowledge suggests that the “the deeper, the better” principle is rather a simplistic approach for interpreting the clinical importance of the corneal stromal DL.
We can conclude that there is still much to understand about the changes of corneal structure after the photochemical CXL reaction. Experimental and clinical researchers on CXL have proven a good effectiveness in stabilizing keratoconus and iatrogenic keratectasia. Moreover, the constant aim of basic and clinical research will be the identification of the best strategies of treatment that is able to obtain the best clinical efficacy together with the maximum safety profile with very few side effects.
Disclosure
The authors report no conflicts of interest in this work.
References
- WollensakGSpoerlESeilerTRiboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconusAm J Ophthalmol2003135562062712719068
- SpadeaLCorneal collagen cross-linking with riboflavin and UV-A irradiation in pellucid marginal degenerationJ Refract Surg201026537537720128533
- ZiaeiMBarsamAShamieNASCRS Cornea Clinical CommitteeReshaping procedures for the surgical management of corneal ectasiaJ Cataract Refract Surg201541484287225840308
- Gordon-ShaagAMillodotMShneorELiuYThe genetic and environmental factors for keratoconusBiomed Res Int2015201579573826075261
- BinderPSAnalysis of ectasia after laser in situ keratomileusis: risk factorsJ Cataract Refract Surg20073391530153817720066
- SpadeaLCanteraECortesMConocchiaNEStewartCWCorneal ectasia after myopic laser in situ keratomileusis: a long-term studyClin Ophthalmol201261801181323152659
- KirwanCO’MalleyDO’KeefeMCorneal hysteresis and corneal resistance factor in keratoectasia: finding using the Reichert ocular response analyzerOphthalmologica2008222533433718628636
- VaziraniJBasuSKeratoconus: current perspectivesClin Ophthalmol201372019203024143069
- O’BrartDPCorneal collagen cross-linking: a reviewJ Optom20147311312425000866
- HammersteinWZur genetic des keratoconus [The genetics of keratoconus]Albrecht Von Graefes Arch Klin Exp Ophthalmol197419042933084547927
- ZhouLSawaguchiSTwiningSSSugarJFederRSYueBYExpression of degradative enzymes and protease inhibitors in corneas with keratoconusInvest Ophthalmol Vis Sci1998397111711249620070
- AndreassenTSimonsenAHOxlundHBiomechanical properties of keratoconus and normal corneasExp Eye Res19803144354417449878
- KuoICBromanAPirouzmaneshAMeliaMIs there an association between diabetes and keratoconusOphthalmology2006113218419016368147
- CannonDJFosterCSCollagen crosslinking in keratoconusInvest Ophthalmol Vis Sci19781716365621128
- SpadeaLMaraoneGCaginiCA case of unilateral circumscribed posterior keratoconus evaluated by three different imaging tools: optical coherence tomography, videokeratography, and Scheimpflug corneal tomographyInt Ophthalmol15 Epub513201626758069
- PanosGDHafeziFGatzioufasZPellucid marginal degeneration and keratoconus; differential diagnosis by corneal topographyJ Cataract Refract Surg201339696823688900
- SpoerlEHuhleMSeilerTInduction of cross-links in corneal tissueExp Eye Res1998661971039533835
- Raiskup-WolfFHoyerASpoerlEPillunatLECollagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term resultsJ Cataract Refract Surg200834579680118471635
- CaporossiAMazzottaCBaiocchiSCaporossiTLong-term results of riboflavin ultraviolet A corneal collagen crosslinking for keratoconus in Italy: the Siena eye cross studyAm J Ophthalmol2010149458559320138607
- Wittig-SilvaCWhitingMLamoureuxELindsayRGSullivanLJSnibsonGRA randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary resultsJ Refract Surg2008247S720S72518811118
- CaporossiAMazzottaCBaiocchiSCaporossiTDenaroRAge-related long-term functional results after riboflavin UV A corneal crosslinkingJ Ophthalmol2011201160804121837270
- SpoerlESeilerTTechniques for stiffening the corneaJ Refract Surg199915671171310590015
- RandlemanJBKhandelwalSSHafeziFCorneal cross-linkingSurv Ophthalmol201560650952325980780
- SpadeaLSalvatoreSParoliMPVingoloEMRecovery of corneal sensitivity after collagen crosslinking with and without epithelial debridement in eyes with keratoconusJ Cataract Refract Surg201541352753225648281
- SpadeaLMencucciRTransepithelial corneal collagen cross-linking in ultrathin keratoconic corneasClin Ophthalmol201261785179223152657
- GatzioufasZRichozOBrugnoliEHafeziFSafety profile of high-fluence corneal collagen cross-linking for progressive keratoconus: preliminary results from a prospective cohort studyJ Refract Surg201329284684824168788
- BeshtawiIMAkhtarRHillarbyMCBiomechanical changes after repeated collagen cross-linking on human corneas assessed in vitro using scanning acoustic microscopyInvest Ophthalmol Vis Sci20145531549155424508795
- RaiskupFSpoerlECorneal crosslinking with riboflavin and ultraviolet A. I. PrinciplesOcul Surf2013112657423583042
- MastropasquaLLanziniMCurcioCStructural modifications and tissue response after standard epi-off and iontophoretic corneal crosslinking with different irradiation proceduresInvest Ophthalmol Vis Sci20145542526253324667859
- MencucciRAmbrosiniSPaladiniIEarly effects of corneal collagen cross-linking by iontophoresis in ex vivo human corneasGraefes Arch Clin Exp Ophthalmol2015253227728625363654
- BikbovaGBikbovMTransepithelial corneal collagen cross-linking by iontophoresis of riboflavinActa Ophthalmol20149213034
- VinciguerraPRandlemanJBRomanoVTransepithelial iontophoresis corneal collagen cross-linking for progressive keratoconus: initial clinical outcomesJ Refract Surg2014301174675325375847
- KanellopoulosAJBinderPSManagement of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocolJ Refract Surg201127532333121117539
- KymionisGDPortaliouDMDiakonisVFManagement of post laser in situ keratomileusis ectasia with simultaneous topography guided photorefractive keratectomy and collagen cross-linkingOpen Ophthalmol J20115111321399769
- SpadeaLParoliMSimultaneous topography-guided PRK followed by corneal collagen cross-linking after lamellar keratoplasty for keratoconusClin Ophthalmol201261793180023152658
- KymionisGDPortaliouDMDiakonisVFPosterior linear stromal haze formation after simultaneous photorefractive keratectomy followed by corneal collagen cross-linkingInvest Ophthalmol Vis Sci201051105030503320463316
- ErtanAKaracalHKamburogluGRefractive and topographic results of transepithelial cross-linking treatment in eyes with intacsCornea200928771972319574920
- Renesto AdaCMeloLAJrSartori MdeFCamposMSequential topical riboflavin with or without ultraviolet a radiation with delayed intracorneal ring segment insertion for keratoconusAm J Ophthalmol2012153598299322265143
- SpadeaLMaraoneGCaginiCSliding keratoplasty followed by transepithelial iontophoresis collagen cross-linking for pellucid marginal degenerationJ Refract Surg2016321475026812714
- KanellopoulosAJLong-term safety and efficacy follow-up of prophylactic higher fluence collagen cross-linking in high myopic laser-assisted in situ keratomileusisClin Ophthalmol201261125113022888210
- CroxattoJOTytiunAEArgentoCJSequential in vivo confocal microscopy study of corneal wound healing after cross-linking in patients with keratoconusJ Refract Surg201026963864519928694
- MazzottaCBalestrazziATraversiCTreatment of progressive keratoconus by riboflavin UVA induced cross linking of corneal collagen: ultrastructural analysis by Heidelberg retinal tomography II in vivo confocal microscopy in humansCornea200726439039717457184
- MazzottaCBalestrazziABaiocchiSTraversiCCaporossiAStromal haze after combined riboflavin-UVA corneal collagen cross-linking in keratoconus: in vivo confocal microscopic evaluationClin Experiment Ophthalmol200735658058217760642
- DhaliwalJSKaufmanSCCorneal collagen cross-linking: a confocal, electron, and light microscopy study of eye bank corneasCornea2009281626719092408
- KamaevPFriedmanMDSherrEMullerDPhotochemical kinetics of corneal cross-linking with riboflavinInvest Ophthalmol Vis Sci20125342360236722427580
- WollensakGSpoerlEWilschMSeilerTKeratocyte apoptosis after corneal collagen cross-linking using riboflavin/UVA treatmentCornea2004231434914701957
- SeilerTHafeziFCorneal cross-linking-induced stromal demarcation lineCornea20062591057105917133053
- KymionisGDTsoulnarasKILiakopoulosDASkatharoudiCAGrentzelosMATsakalisNGCorneal stromal demarcation line depth following standard and a modified high intensity corneal cross-linking protocolJ Refract Surg201632421822227070227
- YamJCChanCWChengACCorneal collagen cross-linking demarcation line depth assessed by Visante OCT after CXL for keratoconus and corneal ectasiaJ Refract Surg201228747548122767165
- MoramarcoAIovienoASartoriAFontanaLCorneal stromal demarcation line after accelerated crosslinking using continuous and pulsed lightJ Cataract Refract Surg201541112546255126703505
- DoorsMTahzibNGEgginkFABerendschotTTWebersCANuijtsRMUse of anterior segment optical coherence tomography to study corneal changes after collagen cross-linkingAm J Ophthalmol2009148684485119781685
- GatzioufasZBalidisMKozeisNIs the corneal stromal demarcation line depth a true indicator of corneal collagen crosslinking efficacy?J Cataract Refract Surg201642580427255259
- KymionisGDGrentzelosMAPlakaADCorrelation of the corneal collagen cross-linking demarcation line using confocal microscopy and anterior segment optical coherence tomography in keratoconic patientsAm J Ophthalmol2014157111011524200235
- MaltaJBRenestoACMoscoviciBKSoongHKCamposMStromal demarcation line induced by corneal cross-linking in eyes with keratoconus and non keratoconic asymmetric topographyCornea201534219920325514703
- KymionisGDTsoulnarasKIGrentzelosMAEvaluation of corneal stromal demarcation line depth following standard and a modified-accelerated collagen cross-linking protocolAm J Ophthalmol2014158467167525034113
- KymionisGDTsoulnarasKIGrentzelosMACorneal stroma demarcation line after standard and high-intensity collagen crosslinking determined with anterior segment optical coherence tomographyJ Cataract Refract Surg201440573674024630796
- ShettyRPahujaNKNuijtsRMCurrent protocols of corneal collagen crosslinking – visual, refractive and tomographic outcomesAm J Ophthalmol2015160224324926008626
- OzgurhanEBSezgin AkcayBIYildirimYKaratasGKurtTDemirokAEvaluation of corneal stromal demarcation line after two different protocols of accelerated corneal collagen cross-linking procedures using anterior segment optical coherence tomography and confocal microscopyJ Ophthalmol2014201498189325485145
- MazzottaCTraversiCCaragiuliSRechichiMPulsed vs continuous light accelerated corneal collagen crosslinking: in vivo qualitative investigation by confocal microscopy and corneal OCTEye (Lond)201428101179118325060847
- RichozOHammerATabibianDGatzioufasZHafeziFThe biomechanical effect of corneal collagen cross-linking (CXL) with riboflavin and UV-A is oxygen dependentTransl Vis Sci Technol201327624349884
- FilippelloMStagniEO’BrartDTransepithelial corneal collagen crosslinking: bilateral studyJ Cataract Refract Surg201238228329122104644
- ChenXStojanovicAEidetJRUtheimTPCorneal collagen cross-linking (CXL) in thin corneasEye Vis (Lond)201521526605368
- BottosKMSchorPDreyfussJLNaderHBChamonWEffect of corneal epithelium on ultraviolet-A and riboflavin absorptionArq Bras Oftalmol201174534835122183995
- BonnelSBerguigaMDe RivoyreBDemarcation line evaluation of iontophoresis-assisted transepithelial corneal collagen cross-linking for keratoconusJ Refract Surg2015311364025599541
- BikbovaGBikbovMStandard corneal collagen crosslinking versus transepithelial iontophoresis-assisted corneal crosslinking, 24 months follow-up: randomized control trialActa Ophthalmol Epub201644
- ZhangYSukthankarPTomichJMConradGWEffect of the synthetic NC-1059 peptide on diffusion of riboflavin across an intact corneal epitheliumInvest Ophthalmol Vis Sci20125362620262922447859
