Abstract
Purpose
The purpose of this study was to monitor anti-vascular endothelial growth factor (anti-VEGF) treatment regimens for wet age-related macular degeneration (wAMD) in clinical practice and to determine how they impact the physician, patient, and caregiver treatment experience.
Materials and methods
This was a qualitative analysis based on semistructured interviews with 20 ophthalmologists who had practiced both pro re nata (PRN) and treat-and-extend (T&E) anti-VEGF regimens for wAMD. Interview questions were constructed to assess how the different regimens affected patient and caregiver experiences (in the opinion of the ophthalmologist) in addition to the ophthalmologist’s own experience. The interview included questions relating to 1) issues and benefits of PRN and T&E; 2) logistical and operational issues of introducing proactive therapy, especially T&E, to PRN practice; and 3) actions taken to handle the issues raised in 2).
Results
A total of 18 interview results were eligible for analysis. The study demonstrated that the benefits of T&E compared with PRN included decreased burden of patient consultations, decreased patient and caregiver emotional burden, and a sustained period of macular dryness. The issues associated with T&E were increased number of injections and financial burden from prolonged treatment duration. The ophthalmologists also experienced difficulty explaining the significance of proactive injections to patients. Countermeasures to operational issues experienced by ophthalmologists varied by practice.
Conclusion
Patients, caregivers, and the practicing ophthalmologists experienced benefits associated with a T&E regimen. However, in order to encourage better understanding of the T&E regimen, including its smooth implementation and significance for patients, a formal T&E treatment guideline providing standard practice should be considered.
Introduction
Wet age-related macular degeneration (wAMD) is a chronic disease and a leading cause of blindness in older patients.Citation1–Citation3 Following the recent introduction of anti-vascular endothelial growth factor (anti-VEGF) therapy, wAMD treatment has changed dramatically, with a switch to improving rather than maintaining visual acuity.Citation4
In Japan, after the launch of ranibizumab (Lucentis®; Novartis International AG) in 2009, the pro re nata (PRN) method of administration became the standard approach for anti-VEGF therapy in wAMD. The PRN regimen consists of as-needed injections (depending on patient symptoms) after an initial loading phase of three consecutive monthly injections, with monthly visits to monitor symptoms.Citation5,Citation6
The proactive regimen was introduced with the launch of intravitreal aflibercept (Eylea®; Bayer) in 2012. There are two approaches to proactive therapy: fixed-dosing and treat-and-extend (T&E). Fixed-dosing consists of injections at set intervals (eg, every 8 weeks) after an initial loading phase, regardless of patient symptoms.Citation7 By contrast, T&E does not have a defined injection interval. In general, after a loading phase, monthly injections are continued until no fluid is detected, followed by 2-week extension intervals until the next injection, which is done regardless of symptoms. When fluid is detected, the extension intervals are decreased depending on the severity. Unlike PRN, T&E does not require patients to make monthly visits for monitoring, but rather at intervals determined by the ophthalmologist.Citation5,Citation8
The effectiveness of proactive therapy has been widely reported, and improvements in visual acuity have been achieved with a fewer visits.Citation9–Citation12 Long-term data on anti-VEGF therapy and the various regimens are also becoming available.Citation13,Citation14 While the majority of research focuses on the clinical outcomes of anti-VEGF therapy regimens, several assessments have addressed the logistical difficulties of using anti-VEGF therapy in actual practice.Citation15–Citation18 However, none of these previous assessments address specific differences between the PRN and T&E regimens. With varying visit schedules and approaches to injection criteria, it can be assumed that differences between the two regimens would impact both ophthalmologist and patient treatment experience, ultimately influencing patient adherence to long-term treatment.
The aim of our research was to qualitatively assess the current issues and benefits of the PRN and T&E anti-VEGF therapy regimens and to focus on any issues associated with introducing T&E. Here, we report how proactive therapy is used to treat wAMD in clinical practices in Japan and how the different regimens impact patient, caregiver, and ophthalmologist experience.
Materials and methods
Qualitative assessment was performed using semistructured interviews conducted by IMS Consulting Group™, IMS Japan KK. Interviewees were ophthalmologists selected from a third-party panel by the IMS Consulting Group according to the selection criteria and based on their experience in treating wAMD. Ophthalmologists were required to have introduced proactive therapy for wAMD into their practice and to have current or previous experience with the PRN approach; this stipulation was intended to ensure that the interviewees had working experience with both types of anti-VEGF therapy regimens.
A total of 20 ophthalmologists were recruited from university hospitals, nonacademic hospitals, and ophthalmologist clinics; the ophthalmologists were recruited from the greater Tokyo area (50%), other regional cities (28%), and rural areas (22%). All interviewees were anonymous to the researchers. Interviews were conducted during the period of November 2014 through February 2015. Written informed consent was obtained from all interviewees, and with their consent, the interviews were recorded for transcripts to be used for analysis. All procedures performed in this study were approved and in accordance with the ethical standards of the institutional review board of Tokyo Women’s University Hospital and with the 1964 Declaration of Helsinki and its later amendments.
The interview questions consisted of three parts: 1) issues and benefits of PRN and T&E; 2) logistical and operational issues of introducing proactive therapy, especially T&E, to PRN practice; and 3) actions taken to handle the issues raised in 2).
Results
Interviewee background
During the interview process, it became clear that two interviewees had a different understanding of either the PRN or T&E treatment regimens, and their interviews were removed from the dataset. Background information on the remaining 18 interviewees is shown in and . The distribution of interviewees based on their institution types were as follows: university hospital: n=7, 39%; nonacademic hospital: n=7, 39%; and clinics: n=4, 22%.
Table 1 Background information of interviewees’ institutions
Table 2 Number of patients seen by the interviewees
Benefits and issues of T&E and PRN
The benefits and issues of PRN and T&E were evaluated from two perspectives: the patient or caregiver perspective as understood by the treating ophthalmologist and the treating ophthalmologist’s own perspective.
There were three main areas where the patient or caregiver experienced benefits with T&E, according to the ophthalmologists. These included the following: “Able to tangibly experience treatment efficacy through the sustained period of macular dryness”, “Decrease in emotional burden associated with receiving intraocular injections”, and “Decrease in patient/caregiver time burden” (). From the treating ophthalmologists’ perspective, the following three areas were identified: “Shorter consultation time per patient”, “Decrease in burden of developing patient specific treatment plans”, and “Decrease in overall psychological stress” ().
Table 3 Benefits and issues of T&E compared with PRN from the patient/caregiver perspective as understood by the treating ophthalmologist
Table 4 Benefits and issues of T&E compared with PRN from the treating ophthalmologist perspective
The issues surrounding T&E were those related to the increase in intravitreal injections and concerns arising from the long-term treatment. Concerns over financial burden associated with an increase in intravitreal injections were highlighted from both the patient/caregiver and treating ophthalmologist perspectives. For patients who achieved dryness of the macula and stabilization of symptoms, there appeared to be difficulty in getting them to understand the significance of continuing with proactive injections, which in effect prevent their symptoms from worsening.
Issues arising from the introduction of T&E and countermeasures
summarizes the different issues ophthalmologists faced when introducing T&E to their practice, according to their institution type. These issues can be possibly identified in two stages: the “patient explanation phase” and the “operational phase”. While university hospital ophthalmologists did not consider “Handling concerns of financial burden from long-term treatment” as an issue they faced during consultations, ophthalmologists based in clinics all raised this issue as a concern. Only university hospital ophthalmologists raised “Increased burden of managing appointments” as a concern.
Figure 1 Issues arising from the introduction of T&E categorized by institution type.
Abbreviations: PRN, pro re nata; T&E, treat-and-extend.
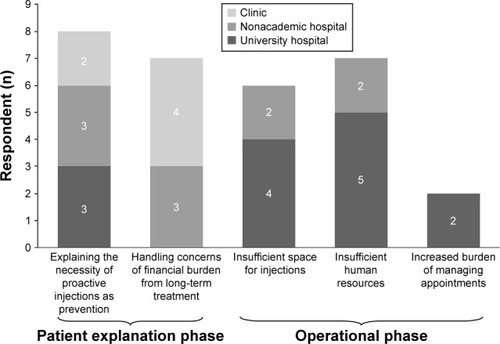
Specific examples of the issues raised in are shown in –, organized by institution type. University hospital ophthalmologists mainly raised four issues as difficulties of practicing T&E: “Explaining the necessity of proactive injections as prevention”, “Insufficient space for injections”, “Insufficient human resources”, and “Increased burden of managing appointments”. The following six countermeasures were provided as remedies implemented: “Explained the efficacy/effectiveness in a more tangible way to the patient”, “Strengthened cooperation with other local facilities and referred patients”, “Employed part-time ophthalmologists”, “Delegated tasks of the injection process and defined the roles of each ophthalmologist”, “Shortened the turn-around time of patients receiving injections”, and “Implemented a scheduling system to manage appointments”.
Table 5 Issues arising from introducing T&E and their countermeasures as answered by university hospital ophthalmologists
Table 6 Issues arising from introducing T&E and their countermeasures as answered by nonacademic hospital ophthalmologists
Table 7 Issues arising from introducing T&E and their countermeasures as answered by clinic ophthalmologists
Specific issues raised by nonacademic hospital ophthalmologists were the same as those raised by university hospital ophthalmologists, except for “Increased burden of managing appointments”. A different countermeasure provided was “Provided injections in outpatient treatment rooms instead of operating rooms”, since operating rooms require reservations making scheduling complicated.
Clinic-based ophthalmologists raised two issues relating to “Explaining the necessity of proactive injections as prevention” and “Handling concerns of financial burden from long-term treatment”. The countermeasures implemented for these issues were “Explained the efficacy/effectiveness in a more tangible way to the patient” and “Prioritized patients who were referred from other hospitals and understood T&E”.
Discussion
Interviews with ophthalmologists revealed that compared with PRN, T&E decreased emotional burden for patients/caregivers and time burden for patients/caregivers and ophthalmologists. An additional patient benefit was the sustained period of macular dryness. The main issues raised were the increased number of injections and the associated financial burden from prolonged treatment duration. Issues arising from the introduction of T&E at the “patient explanation phase” or “operational phase” depended on practice type.
The analysis highlighted that predetermined scheduled injections (T&E) provided relief by ensuring that visits did not result in “bad news” and unforeseen injections compared with PRN; this decreased the emotional burden for patients and caregivers. Droege et alCitation19 revealed that patients were more afraid of receiving negative examination results than the actual intravitreal injections, indicating that worsening of symptoms impacts patient experience more than frequency of injections.
These interview results also revealed that T&E reduced time burden for patients and caregivers in clinical practice by decreasing the amount of necessary visits. This is important because monthly monitoring of PRN has been considered burdensome for ophthalmologists, patients, and caregivers in previous studies.Citation5,Citation9,Citation16 For example, Gohil et alCitation20 looked at caregiver burden of PRN in the UK and on average, 70% of caregivers spent at least half a day assisting their patients with clinic visits every 4–6 weeks, and about 25% took time off from work. According to Droege et al,Citation19 patients indicated that travel to and from visits was a major barrier to their wAMD treatment adherence. Combined with our results, it can be inferred that a fewer visits for T&E may result in better adherence by patients to long-term treatment.
The ophthalmologists also spoke of the reality of organizing PRN injections: once the patient was indicated for injection, the facility may not always be able to provide it on the same day, causing the patient to schedule another visit. If the caregiver was unable to accompany the patient for the rescheduled visit, the patient was subjected to even further delay in receiving timely treatment. This is an important issue for treating a time-sensitive condition such as wAMD. A study analyzing a hospital claims database in Japan showed that an average of 11.6 days elapsed between injections and the previous outpatient monitoring visits under PRN.Citation21 Likewise, Takahashi et alCitation22 analyzed two hospitals in Japan and found average injection delays under PRN of between 0 and 104 days. These studies further indicate that injection delays are not rare with PRN approaches in real-life settings. Takahashi et alCitation22 also revealed that visual acuity prognosis worsened with injection delays. Similarly, Rayess et alCitation12 found that patients receiving consecutive maintenance injections with T&E were less susceptible to recurrence of disease activity than PRN, where duration of consecutive injections tends to be prolonged. Previous studies reporting visual acuity outcomes with PRN dosing were conducted with patients receiving injections on the same day,Citation6,Citation14 which, compared with treatment pattern studies, may not reflect real-life clinical practice.Citation21,Citation22 As reported in our analysis, T&E is able to avoid such delays and missed injection opportunities by following a predetermined injection schedule, which leads to prolonged dryness of the macula and prevention of worsening of symptoms. While previous studies have focused on ophthalmologists’ experience of such clinical outcomes, our analysis reveals for the first time that patients (based on ophthalmologist feedback) are also able to tangibly experience the effectiveness of anti-VEGF treatment with T&E, which can be linked to increased treatment satisfaction and likely treatment adherence.
As mentioned earlier, issues of introducing T&E into the clinical practice can be identified in two stages: the patient explanation phase and the operational phase. There were benefits associated with decreased emotional burden from simplified consultations with patients who already understood the necessity of receiving injections at their visits. However, ophthalmologists also had difficulties in explaining the preventive effect of T&E, which was identified in all institution types. They had difficulty convincing patients who had entered the maintenance phase of their treatment with stable disease activity to continue with proactive injections before any disease activity resumes. While this difficulty was common to ophthalmologists across all institution types, the management of this issue appeared to differ. This phenomenon may be attributed to the lack of a guideline for T&E articulating how to manage injections during the maintenance phase of a patient’s disease state. A literature review with consensus recommendations on T&E was published in 2015, but there remains a lack of evidence-based resource that can support Japanese practice.Citation8
Issues in the operational phase were raised mostly from university hospital ophthalmologists. University hospitals appear to be overburdened. They have a relatively greater number of wAMD patients compared with hospitals and clinics; T&E also results in increased injections per patient and a fewer dropouts, resulting in an increased number of total patients continuing anti-VEGF treatment. Rearranging the patient flow and dividing staff roles to improve efficiency were provided as effective actions. However, increased staff and space for administering injections seemed to be ultimately desired even after such measures. It should also be noted that issues with staff and spatial capacity have been reported in previous studies with PRN, and this could be an ongoing issue that is not unique to the practice of T&E.Citation15,Citation16,Citation18,Citation22
Strengthening local clinic and university hospital relations in order to increase referrals to clinics was also raised as a potential solution to the operational phase issues. It appears that this is currently practiced only in limited areas. Implementing integrated care pathways is still in its infancy in Japan, particularly in ophthalmology. At present, there have only been pilot trials with glaucoma and ophthalmologic care for patients with dementia.Citation23,Citation24 Disparity in care between practices is also an issue.Citation25 This was also observed by Takahashi et al.Citation22 This variation in care further reiterates the need for an evidence-based standardized method of practicing T&E that can be followed by ophthalmologists across practices.
There are several limitations to this qualitative analysis. First, interviewees were limited and lacked representativeness of a larger population. Second, interviewees were located primarily within the greater Tokyo metropolitan area or other regional cities, and their responses may not reflect the realities of other regional situations. We performed subgroup analyses by region and facility types (hospital vs clinic ophthalmologists) to see if there were any differences. It was revealed that there were no interesting/meaningful results by region (data not shown), but we did find a difference between hospital and clinic ophthalmologists. This is why we only reported the facility type differences in the manuscript.
Conclusion
This qualitative analysis demonstrated that the benefits of T&E compared with PRN as reported by ophthalmologists included decreased burden of patient consultations, decreased patient and caregiver emotional burden, and a sustained period of macular dryness. The analysis revealed that patient treatment satisfaction can be increased via T&E, and this may increase the potential for better adherence to long-term treatment. However, increased number of injections and financial burden from prolonged treatment duration remain issues associated with T&E. The ophthalmologists also experienced difficulty explaining the significance of proactive injections for prevention to patients. Countermeasures to operational issues experienced by ophthalmologists varied by practice. In order to encourage better understanding of the T&E regimen, including its smooth implementation and significance for patients, a formal T&E treatment guideline providing standard practice should be considered.
Acknowledgments
We are most grateful to the ophthalmologists who participated in the interviews. We thank Mr Satoru Ono of IMS Consulting Group™, IMS Japan KK, who was involved in the design of the interviews and analysis of the data. The manuscript was developed and authorized by the authors. The manuscript has also been authorized by Mr Ono as a member who partook in the analysis. This study was funded by Bayer Yakuhin, Ltd.
Disclosure
Tomohiro Iida has received research grants from Bayer Yakuhin, Ltd., Santen Pharmaceutical Co., Ltd., Novartis Pharmaceutical KK, and Alcon Japan Ltd. Keirei Ishii is an employee of Bayer Yakuhin, Ltd. The authors report no other conflicts of interest in this work.
References
- FriedmanDSO’ColmainBJMunozBEye Diseases Prevalence Research GroupPrevalence of age-related macular degeneration in the United StatesArch Ophthalmol2004122456457215078675
- WongWLSuXLiXGlobal prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysisLancet Glob Health201422e106e11625104651
- KawasakiRYasudaMSongSJThe prevalence of age-related macular degeneration in Asians: a systematic review and meta-analysisOphthalmology2010117592192720110127
- SivaprasadSHykinPWhat is new in the management of wet age-related macular degeneration?Br Med Bull201310520121123393060
- HatzKPrunteCTreat and extend versus pro re nata regimens of ranibizumab in neovascular age-related macular degeneration: a comparative 12 month studyActa Ophthalmol Epub2016324
- MartinDFMaguireMGFineSLRanibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year resultsOphthalmology201211971388139822555112
- HeierJSBrownDMChongVVIEW 1 and VIEW 2 Study GroupsIntravitreal aflibercept (VEGF trap-eye) in wet age-related macular degenerationOphthalmology2012119122537254823084240
- FreundKBKorobelnikJFDevenyiRTreat-and-extend regimens with anti-VEGF agents in retinal diseases: a literature review and consensus recommendationsRetina20153581489150626076215
- GuptaOPShienbaumGPatelAHFecarottaCKaiserRSRegilloCDA treat and extend regimen using ranibizumab for neovascular age-related macular degeneration clinical and economic impactOphthalmology2010117112134214020591490
- ArnoldJJCampainABarthelmesDTwo-year outcomes of “treat and extend” intravitreal therapy for neovascular age-related macular degenerationOphthalmology201512261212121925846847
- HomerNGrewalDSMirzaRGLyonATGillMKTransitioning to intravitreal aflibercept following a previous treat-and-extend dosing regimen in neovascular age-related macular degeneration: 24-month resultsEye (Lond)20152991152115526021870
- RayessNHoustonSK3rdGuptaOPHoACRegilloCDTreatment outcomes after 3 years in neovascular age-related macular degeneration using a treat-and-extend regimenAm J Ophthalmol201515913825217859
- RofaghaSBhisitkulRBBoyerDSSaddaSRZhangKSeven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP)Ophthalmology2013120112292229923642856
- Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research GroupMaguireMGMartinDFYingGSFive-year outcomes with anti-vascular endothelial growth factor treatment of neovascular age-related macular degeneration: the comparison of age-related macular degeneration treatments trialsOphthalmology201612381751176127156698
- AmoakuWBlakeneySFreemanMAction on AMD GroupAction on AMD. Optimising patient management: act now to ensure current and continual delivery of best possible patient careEye (Lond)201226suppl 1S2S2122302094
- Casaroli-MaranoRRouraMGrupo de Estudio OptimalDisponibilidad de recursos para pacientes con degeneración macular asociada a la edad de tipo húmedo. Estudio Optimal [Availability of resources for patients with wet age-related macular degeneration. Optimal study]Arch Soc Esp Oftalmol201388830731223886362
- MichelottiMMAbugreenSKellySPTransformational change: nurses substituting for ophthalmologists for intravitreal injections – a quality-improvement reportClin Ophthalmol2014875576124790403
- PrennerJLHalperinLSRycroftCHogueSWilliamsLZSeibertRDisease burden in the treatment of age-related macular degeneration: findings from a time-and-motion studyAm J Ophthalmol2015160472573126142721
- DroegeKMMuetherPSHermannMMAdherence to ranibizumab treatment for neovascular age-related macular degeneration in real lifeGraefes Arch Clin Exp Ophthalmol201325151281128423086225
- GohilRCrosby-NwaobiRForbesABurtonBHykinPSivaprasadSCaregiver burden in patients receiving ranibizumab therapy for neovascular age related macular degenerationPLoS One2015106e012936126056840
- IidaTNarimatsuAAdachiKWangECYAnti-vascular endothelial growth factor outpatient treatment patterns in patients with exudative age-related macular degeneration from a Japanese hospital claims databaseJHEOR2014214152
- TakahashiHOhkuboYSatoARelationship between visual prognosis and delay of intravitreal injection of ranibizumab when treating age-related macular degenerationRetina20153571331133825719984
- KashiwagiKより質の高い緑内障診療を目指して [Toward a high quality glaucoma care]Nippon Ganka Gakkai Zasshi2012116326929622568104
- MiyamuraYSotozonoCHigashiharaHHoshiSKinoshitaS認知症を伴う高齢者の重症眼感染症 [Severe ocular infection in elderly patients with dementia: a case study]Nippon Ganka Gakkai Zasshi20151191286386726817134
- SutoSHiraokaTOkamotoYOkamotoFOshikaTスマートフ ォンによる前眼部および眼底撮影 [Photography of anterior eye segment and fundus with smartphone]Nippon Ganka Gakkai Zasshi2014118171424505930
