Abstract
Purpose
To evaluate the association between the size of peripheral retinal nonperfusion and the number of intravitreal ranibizumab injections in patients with treatment-naïve central retinal vein occlusion (CRVO).
Methods
Fifty-four patients with treatment-naïve CRVO and macular edema were included. Each patient underwent a full ophthalmologic examination including optical coherence tomography imaging and ultrawide-field fluorescein angiography. Monthly intravitreal ranibizumab injections were applied according to the recommendations of the German Ophthalmologic Society. Two ophthalmologists quantified the areas of peripheral retinal nonperfusion (group 1= less than five disc areas, group 2= more than five disc areas). Correlation analyses between the size of nonperfusion with best-corrected visual acuity, central subfield thickness, and the number of intravitreal injections were performed.
Results
Best-corrected visual acuity improved significantly after intravitreal injections (P<0.001, both groups). Final central subfield thickness after treatment did not significantly differ between both groups (P=0.92, P=0.96, respectively). Mean number of injections in group 1 and group 2 was 4.12±2.73 and 9.32±3.84, respectively (P<0.001). There was a significant positive correlation between areas of nonperfusion and the number of injections in each group. (R=0.97, P<0.001; R=0.94, P<0.001, respectively).
Conclusion
Peripheral retinal nonperfusion in patients with CRVO correlates significantly with the number of needed intravitreal ranibizumab injections. Ultrawide-field fluorescein angiography is a useful tool for detection of peripheral retinal ischemia, which may have direct implications in the diagnosis, follow-up, and treatment of these patients.
Introduction
Central retinal vein occlusion (CRVO) is a common sight-threatening vascular disease with prevalence rates ranging from 0.1%Citation1 to 0.5%Citation2 in the older adult population. CRVO is characterized by occlusion of the central retinal vein and consecutive damming of the venous blood flow. The occlusion may occur at the level of or posterior to the lamina cribrosa.Citation3 Despite its prevalence, the pathogenesis of CRVO is not completely understood. A combination of vascular, anatomic, and inflammatory factors may contribute to its pathophysiology.Citation4 Current treatment options include intravitreal injections of steroidsCitation5 or anti-vascular endothelial growth factor (anti-VEGF) agents.Citation6–Citation8
Fluorescein angiographic (FA) assessment is the most important tool for an adequate evaluation of the disease severity and for proper classification between the two types of CRVO, ischemic and nonischemic. Ischemic CRVO is associated with a significant upregulation of VEGF, a poor prognosis for visual acuity, and has a higher incidence of secondary neovascular glaucoma (NVG) ranging from 20% to 60% compared to nonischemic CRVO with no risk of developing NVG.Citation9 Given these significant differences with various outcomes and risk profiles, it is crucial to differentiate between ischemic and nonischemic CRVO.
Conventional FA images the retinal circulation within the posterior pole. However, it is not known if conventional FA devices are able to capture areas of interest regarding the intraocular metabolism of VEGF, such as the peripheral retina. Earlier findings suggested an association between peripheral retinal ischemia and an increased production of VEGF.Citation10,Citation11 Currently, two ultrawide-field systems are commercially available to perform FA and image the peripheral retina. One method uses a wide-field contact lens system (Ocular Staurenghi 230 SLO Retina Lens; Ocular Instruments, Inc, Bellevue, WA, USA) with the Heidelberg retina angiograph (HRA; Heidelberg Engineering GmbH, Dossenheim, Germany).Citation12,Citation13 The second available system uses the Optos scanning laser ophthalmoscope (Optos PLC, Dunfermline, UK), which is a special non-contact-lens-based system that provides visualization up to the peripheral retina.Citation14–Citation16 It has been shown that ultrawide-field FA (UWFA) is useful for the assessment of several retinal pathologiesCitation17 including retinal vein occlusions,Citation18 diabetes,Citation19,Citation20 uveitis,Citation21 retinal vasculitis,Citation22 choroidal masses,Citation23,Citation24 retinal detachment,Citation25 and retinopathy of prematurity.Citation26
The aim of this study was to evaluate a possible association between peripheral retinal nonperfusion obtained with UWFA and the number of intravitreal ranibizumab injections needed in patients with CRVO.
Methods
Patient selection
This prospective interventional study was performed between June 1, 2012, and February 1, 2014. The institutional Review Board of Ludwig-Maximilians University in Munich approved the study design, and patients’ care adhered to the tenets of the World Medical Association Declaration of Helsinki. All patients gave written informed consent for both participation in the study and for FA. Inclusion criteria were diagnosis of CRVO (as revealed by retinal hemorrhages and dilated retinal veins in all four quadrants of the fundus) with active center-involving macular edema and central subfield thickness >250 µm detected by spectral-domain optical coherence tomography (SD-OCT, Heidelberg Engineering, Heidelberg, Germany).
Patients without macular edema, with previous focal or panretinal photocoagulation, and with degenerative disorders of the posterior pole and/or retinal periphery were excluded. Additional intravitreal injections were administered in the presence of active center-involving macular edema and central subfield thickness >250 µm, as determined by SD-OCT. All patients underwent comprehensive ophthalmologic examination that included best-corrected visual acuity (BCVA) measurement, slit-lamp biomicroscopy, applanation tonometry, indirect ophthalmoscopy, and SD-OCT before injections and at each follow-up visit. UWFA using the Optos 200T× imaging system was obtained in each case before the first injection. All included patients received three intravitreal injections of 0.50 mg ranibizumab (Lucentis™, Genentech, Inc., South San Francisco, CA, USA and Novartis Pharma AG, Basel, Switzerland) every four weeks and then were examined monthly with follow-up OCT scans of the macula. They received additional intravitreal injections if macular edema was detected by SD-OCT scans at follow-up visits.
Image acquisition
SD-OCT volume scans (20°×15° with 19 horizontal sections, ART 9, SD-OCT, Heidelberg Engineering, Heidelberg, Germany) of the macula were obtained for each study eye to measure the central subfield thickness (CST) in µm by using Heidelberg SD-OCT software; significant macular ischemia was ruled out by UWFA. FA images were acquired approximately one minute (arteriovenous phase) and 4–5 minutes (late venous phase) after intravenous injection using the Optos 200T× scanning laser ophthalmoscope (Optos PLC) after standard intravenous infusion of 5 mL of sodium fluorescein (10%) by one experienced technician for all included cases.
Image processing and analysis
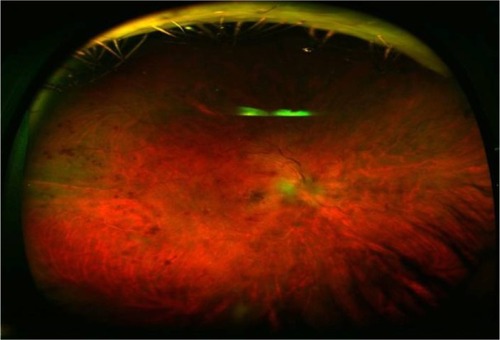
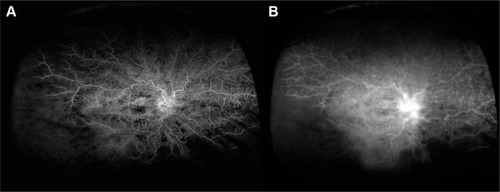
FA images were compressed into high-quality jpeg files ( and ) and analyzed for retinal nonperfusion by two experienced ophthalmologists (KAA and FS). The far peripheral retina was defined as the area between the ampullae of the vortex veins and the ora serrata. The wide-field color images and wide-field FA images were used to identify the vortex vein ampullae, which were located near the ocular equator.Citation27 Based on another published work, we defined retinal nonperfusion as at least five disc areas of hypofluorescenceCitation28 (representing retinal nonperfusion or capillary dropout) or areas of microvascular pathology (multiple microaneurysms and significant perivascular leakage) on UWFA. Five disc areas was also the mean size of peripheral retinal nonperfusion of all our patients with CRVO. Because of the effect of upper and lower eyelid and eyelashes, the far periphery in the horizontal plane alone (the nasal and temporal retina) was analyzed.
Data collection
Collected parameters included demographic information, previous ocular history, number and dates of intravitreal injections, central subfield thickness, peripheral retinal ischemia, central intraretinal fluid, visual acuity, and intraocular pressure (throughout the study period) as well as the occurrence of any complications.
Statistical analysis
Data were collected and analyzed using SPSS software (version 20.0, IBM Corporation, Armonk, NY, USA). Each graded variable was tested for normal distribution. Nonparametric tests were used to analyze nonnormally distributed data. Paired-sample Wilcoxon signed rank test was used for within group analysis. Mann–Whitney U-test was used for intergroup comparison. Spearman rho test was used for correlation analysis. A P-value of <0.05 was considered statistically significant. Mean ± standard deviation were used to report the results.
Results
Fifty-four eyes of fifty-four consecutive patients with treatment-naïve CRVO were enrolled in this study. The average patient age was 74±11.81 years (range, 24–86 years). Twenty-eight patients (52%) were male, and twenty-three eyes (42.6%) were located on the right side. Seven patients (12.9%) had known glaucoma, 36 patients (66.6%) had systemic hypertension, and 22 patients (40.7%) were pseudophakic. Mean follow-up time was 16±3 months. All patients had center-involving macular edema confirmed by macular leakage seen in FA and retinal thickening in SD-OCT images. and show the baseline and final BCVA and CST. As shown in the tables, there were significant improvements in the visual acuity within and between groups, whereas changes in CST were not significant. The mean number of intravitreal injections for each patient was 6.64±3.84. Twenty-four eyes (44%) showing less than five disc areas of retinal nonperfusion (group 1) that received a mean number of 4.12±2.73 intravitreal ranibizumab injections. Thirty eyes (56%) showed more than five disc areas (group 2) of retinal nonperfusion in UWFA and received a mean number of 9.32±3.84 intravitreal ranibizumab injections (P<0.001, Mann–Whitney U-test). There was a significant positive correlation between the size of peripheral retinal nonperfusion measured in terms of disc areas and the number of injections in each group. (R=0.97, P<0.001, R=0.94, P<0.001, respectively). There was also a significant correlation between the size of retinal nonperfusion and final BCVA in each group. (R=0.85, P=0.01, R=0.84, P<0.001, respectively). There was no significant correlation between the size of retinal nonperfusion and final CST in each group. (R=0.2, P=0.78, R=0.1, P=0.5, respectively). We did not observe any eye with neovascularization of the disc or neovascularization elsewhere during the observation period; therefore, panretinal photocoagulation was not performed during this study. Furthermore, no cases of injection-related adverse events like retinal detachment or endophthalmitis were encountered.
Table 1 Changes in visual acuity within and between groups
Table 2 Changes in central subfield thickness within and between groups
Discussion
Venous occlusive disease of the retina is the second most common retinal vascular disorder after diabetic retinopathy.Citation29 It typically affects patients between 40 and 80 years of age.Citation30 Usually, a decrease of visual acuity is the result of macular edema, which can lead to permanent visual loss and even legal blindness in severe cases.
Applying UWFA, we found a significant correlation between the total number of intravitreal ranibizumab injections and the size of nonperfusion in the peripheral retina: CRVO patients with peripheral retinal nonperfusion received more intravitreal injections for treatment of their macular edema than patients without peripheral retinal nonperfusion. We hypothesized that nonperfused peripheral retina could be a source of increased intraocular VEGF levels with consecutive macular edema. This observation could explain the requirement for more frequent intravitreal anti-VEGF injections of in CRVO patients with macular edema and peripheral retinal nonperfusion. This finding is important because an evaluation of the peripheral retina using UWFA may be a prognostic factor and allows the ophthalmologists to estimate the requirement for more or fewer intravitreal injections based on the peripheral retinal perfusion status. Looking at the perfusion of the peripheral retina in those patients, a more precise evaluation of the estimated treatment costs within a defined health care system may be feasible, including a better evaluation of injection-related complications such as endophthalmitis or other complications.
Interestingly, the lack of observed neovascularizations in any of the patients even with extended areas of peripheral retinal nonperfusion might be attributed to good patient compliance, strict follow-up visits every 4 weeks, and immediate treatment in case of detected macular edema.
The results of our study differ from those published by SpaideCitation31 and Singer et al.Citation32 Spaide evaluated 22 patients treated with ranibizumab for CRVO and found that the area of peripheral nonperfusion was not correlated with the number of injections. The follow-up time of his study was longer than ours, but the sample size was smaller. Singer et alCitation32 evaluated 32 patients with retinal vein occlusion and refractory macular edema using SD-OCT and UWFA. Those patients were retreated with intravitreal injections with anti-VEGF and with dexamethasone intravitreal implant. There was no significant difference in the number of anti-VEGF (1.8 vs 1.6, P=0.438) or dexamethasone implant (1.4 vs 1.6, P=0.364) treatments given between the >10% and ≤10% nonperfusion groups, nor was there any difference regarding the time to recurrence (3.4 vs 4.3 months, P=0.440). In Singer et al’s series, there were 13 CRVO patients with previously failed contiguous therapy with intravitreal ranibizumab and dexamethasone implant. In contrast, we enrolled previously untreated (treatment-naïve) patients; furthermore, the number of our cases was higher than in the abovementioned studies. We previously reported that peripheral retinal nonperfusion correlates significantly with intravitreal ranibizumab injections in patients with BRVO and macular edema.Citation33 Rehak et alCitation34 evaluated 22 CRVO patients in a randomized clinical trial and suggested the selective laser photocoagulation of peripheral areas of nonperfusion may further improve the visual outcome and decrease the number of needed ranibizumab reinjections in CRVO patients.
This study has some limitations. There are only few published articles regarding the size of peripheral retinal nonperfusion using UWFA. We calculated the mean size of peripheral retinal nonperfusion for all enrolled patients, which was five disc areas, and then the patients were divided into two groups according to that cut-off point. However, the authors totally agree that this approach is not an established step due to lack of evidence. Moreover, there are several problems in the interpretation of fluorescein angiograms. The grading of the ultrawide-field angiograms is not uniform because there are eyelash artifacts that influence the entire amount of interpretable fundus, and the graders can also change the clarity of the images that may cause intergrader variability. Another drawback of our study design was that we performed UWFA for each patient at only one single time point. Thus, we were not able to demonstrate potential dynamic angiographic changes in nonperfusion areas over the follow-up time.
Conclusion
In conclusion, UWFA is a precise tool for the detection and quantification of retinal nonperfusion which correlated with the number of needed intravitreal ranibizumab injections in our patients with CRVO. Retinal nonperfusion could be considered as a prognostic factor for a more precise patient management.
Disclosure
The authors report no conflicts of interest in this work.
References
- KleinRKleinBEMossSEMeuerSMThe epidemiology of retinal vein occlusion: the Beaver Dam Eye StudyTrans Am Ophthalmol Soc20009813314111190017
- MitchellPSmithWChangAPrevalence and associations of retinal vein occlusion in Australia. The Blue Mountains Eye StudyArch Ophthalmol1996114124312478859084
- HayrehSSPrevalent misconceptions about acute retinal vascular occlusive disordersProg Retin Eye Res200524449351915845346
- GreenWRChanCCHutchinsGMTerryJMCentral retinal vein occlusion: a prospective histopathologic study of 29 eyes in 28 casesTrans Am Ophthalmol Soc1981793714227342407
- RamchandranRSFekratSStinnettSSJaffeGJFluocinolone acetonide sustained drug delivery device for chronic central retinal vein occlusion: 12-month resultsAm J Ophthalmol200814628529118533125
- HeierJSCampochiaroPAYauLRanibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trialOphthalmology201211980280922301066
- BrownDMCampochiaroPASinghRPRanibizumab for macular edema following central retinal vein occlusion: six-month primary end point of a phase III studyOphthalmology20101171124113320381871
- HolzFGRoiderJOguraYVEGF Trap-Eye for macular oedema secondary to central retinal vein occlusion: 6-month results of the phase III GALILEO studyBr J Ophthalmol20139727828423298885
- TsuiIKainesAHavunjianMAIschemic index and neovascularization in central retinal vein occlusionRetina20113110511021099454
- BoydSRZacharyIChakravarthyUCorrelation of increased vascular endothelial growth factor with neovascularization and permeability in ischemic central vein occlusionArch Ophthalmol20021201644164512470137
- NomaHFunatsuHMimuraTHarinoSHoriSVitreous levels of interleukin-6 and vascular endothelial growth factor in macular edema with central retinal vein occlusionOphthalmology20091161879319118700
- StaurenghiGViolaFMainsterMAGrahamRDHarringtonPGScanning laser ophthalmoscopy and angiography with a wide-field contact lens systemArch Ophthalmol200512324425215710823
- NoyoriKSChinoKDeguchiTWide field fluorescein angiography by use of contact lensRetina198331311346878900
- WitmerMTParlitsisGPatelSKissSComparison of ultra-widefield fluorescein angiography with the Heidelberg Spectralis® noncontact ultra-widefield module versus the Optos® Optomap®Clin Ophthalmol2013738939423458976
- ManivannanAPlskovaJFarrowAUltra-wide-field fluorescein angiography of the ocular fundusAm J Ophthalmol2005140352552716139004
- FribergTRGuptaAYuJUltrawide angle fluorescein angiographic imaging: a comparison to conventional digital acquisition systemsOphthalmic Surg Lasers Imaging20083930431118717436
- WitmerMKissSWide-field imaging of the retinaSurv Ophthalmol201358214315423369515
- PrasadPSOliverSCCoffeeREHubschmanJPSchwartzSDUltra wide-field angiographic characteristics of branch retinal and hemicentral retinal vein occlusionOphthalmology2010117478078420045570
- WesselMMAakerGDParlitsisGChoMD’amicoDJKissSUltra-wide-field angiography improves the detection and classification of diabetic retinopathyRetina201232478579122080911
- WesselMMNairNAakerGDEhrlichJRD’AmicoDJKissSPeripheral retinal ischaemia, as evaluated by ultra-widefield fluorescein angiography, is associated with diabetic macular oedemaBr J Ophthalmol201296569469822423055
- MudvariSSViraschVVSingaRMMacCumberMWUltra-wide-field imaging for cytomegalovirus retinitisOphthalmic Surg Lasers Imaging201041331131520507014
- ChoMKissSDetection and monitoring of sickle cell retinopathy using ultra wide-field color photography and fluorescein angiographyRetina201131473874721836403
- Pe’erJSanchoCCantuJMeasurement of choroidal melanoma basal diameter by wide-angle digital fundus camera: a comparison with ultrasound measurementOphthalmologica2006220319419716679796
- ShieldsCLMaterinMShieldsJAPanoramic imaging of the ocular fundusArch Ophthalmol2003121111603160714609919
- WitmerMTChoMFavaroneGChanRVD’AmicoDJKissSUltra-wide-field autofluorescence imaging in non-traumatic rhegmatogenous retinal detachmentEye (Lond)20122691209121622722489
- FungTHYusufIHSmithLMBrettJWestonLPatelCKOutpatient Ultra wide-field intravenous fundus fluorescein angiography in infants using the Optos P200MA scanning laser ophthalmoscopeBr J Ophthalmol20149830230424338087
- KanekoYMoriyamaMHiraharaSOguraYOhno-MatsuiKAreas of nonperfusion in peripheral retina of eyes with pathologic myopia detected by ultra-widefield fluorescein angiographyInvest Ophthalmol Vis Sci20145531432143924526439
- SuñerIJPedenMCHammerMEGrizzardWSTraynomJCousinsSWRaScaL: a pilot study to assess the efficacy, durability, and safety of a single intervention with ranibizumab plus peripheral laser for diabetic macular edema associated with peripheral nonperfusion on ultrawide-field fluorescein angiographyOphthalmologica20152338995
- KolarPRisk factors for central and branch retinal vein occlusion: a meta-analysis of published clinical dataJ Ophthalmol2014201472478025009743
- ZhouJQXuLWangSThe 10-year incidence and risk factors of retinal vein occlusion: the Beijing eye studyOphthalmology2013120480380823352194
- SpaideRFPeripheral areas of nonperfusion in treated central retinal vein occlusion as imaged by wide-field fluorescein angiographyRetina201131582983721487338
- SingerMTanCSBellDSaddaSRArea of peripheral retinal non-perfusion and treatment response in branch and central retinal vein occlusionRetina20143491736174224732695
- Abri AghdamKReznicekLSoltan SanjariMPeripheral retinal non-perfusion and treatment response in branch retinal vein occlusionInt J Ophthalmol20169685886227366688
- RehakMTilgnerEFrankeAAuscherFGBrosteanuOWiedemannPEarly peripheral laser photocoagulation of nonperfused retina improves vision in patients with central retinal vein occlusion (Results of a proof of concept study)Graefes Arch Clin Exp Ophthalmol2014252574575224346235