Abstract
Purpose
To study the long-term visual and refractive outcomes and evaluate patient satisfaction after bilateral implantation of trifocal intraocular lenses (IOLs).
Setting
Nethradhama Superspeciality Eye Hospital, Bangalore.
Design
Prospective, nonrandomized study.
Methods
Eligible patients undergoing bilateral phacoemulsification with trifocal IOL implantation were included. Follow-up examinations were conducted at day 1, 1 week, 1 month, 6 months, and 12 months. Postoperatively, 1 month onward evaluation of uncorrected and distance-corrected far and near visual acuity; reading acuity and reading speeds (using Salzburg Reading Desk) at 70, 80, and 90 cm; contrast sensitivity; defocus curves; and patient satisfaction was carried out.
Results
Fifty eyes from 25 patients with a mean age of 58±13.44 years were included. All eyes showed significant improvement in spherical equivalent, uncorrected distance visual acuity, corrected distance visual acuity, uncorrected near visual acuity, and corrected near visual acuity at 1 month compared to preoperative values (P<0.05), with no significant change in these parameters thereafter until the last follow-up (P>0.05). At 12 months, mean uncorrected reading acuities and reading speeds at 70, 80, and 90 cm were in the range of 0.09–0.04 logMAR units and 153.6–169.0 words per minute, respectively, with significantly better results at 80 cm. Five eyes underwent YAG laser capsulotomy for early posterior capsule opacification (PCO) at a mean follow-up of 7.2±2.9 months. Contrast sensitivity scores at 12 months were comparable to 1 month (P>0.05 for all spatial frequencies). All patients reported good tolerance and 100% independence from spectacles for all activities.
Conclusion
Trifocal IOLs provided excellent unaided vision at all distances. Reading performance was good through the complete intermediate distance range. PCO occurrence and subsequent YAG capsulotomy did not affect the long-term visual outcomes.
Introduction
Recently, various multifocal intraocular lenses (IOLs) have been shown to reduce dependence on glasses after cataract surgery.Citation1–Citation4 These IOLs can be either refractive or diffractive in design or a combination of both. However, each of these may have potential disadvantages such as pupil dependence with refractive IOLs.Citation5,Citation6 However, on optical bench testing, diffractive multifocal IOLs have been shown to provide better optical quality, contrast sensitivity, and less photic phenomena than refractive IOLs.Citation7,Citation8
Traditional multifocal IOLs are bifocal and have two focal points for far and near distance, at which they produce a sharp image on the retina.Citation2 The introduction of a third focus with the aim of providing good intermediate vision, between the two focal points, has led to the development of trifocal IOLs. Recently, the safety and efficacy of these IOLs in providing good functional vision at intermediate distance have been evaluated.Citation9,Citation10
The aim of the present study was to evaluate visual and refractive outcomes with the AT LISA tri 839MP or Zeiss trifocal IOL, assess reading speeds using Salzburg Reading Desk (SRD), and evaluate patient satisfaction and spectacle independence in a long-term follow-up of 1 year after surgery.Citation11
Methods
This prospective, single-center study was approved by the hospital ethics committee of Nethradhama Superspeciality Eye Hospital and performed in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent.
Inclusion criteria were healthy eyes besides senile cataract, corneal astigmatism ≤0.75 diopters (D), IOL power calculation resulting in diopters between +10.00 D to +32.00 D, capsular bag IOL implantation, and ability to read English language fluently.
Exclusion criteria were patients with corneal astigmatism of >0.75 D, irregular astigmatism, corneal dystrophy, tear-film or pupillary abnormalities, history of glaucoma or intraocular inflammation, macular disease or retinopathy, neuro-ophthalmic diseases, and intraoperative or postoperative complications.
Preoperative assessment
Preoperatively, all patients underwent a complete ophthalmologic examination including uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), uncorrected near visual acuity (UNVA), distance-corrected near visual acuity (DCNVA) at 40 cm (all measured using log-MAR acuity charts under photopic conditions at 85 candelas [cd]/m2), manifest refraction, slit lamp biomicroscopy, non-contact tonometry, and dilated fundus examination.
Description of the study lens
AT LISA tri 839MP (Carl Zeiss Meditec, Jena, Germany) is a refractive–diffractive trifocal preloaded IOL with a 6.0 mm biconvex optic, an overall diameter of 11.0 mm, and a posterior surface with asphericity of −0.18 µ. It has a four-haptic design with an angulation of 0° and a new 360° square edge to prevent posterior capsule opacification (PCO). It is made of foldable hydrophilic acrylic material with a water content of 25%, a hydrophobic surface, and a refractive index of 1.46. This IOL is trifocal within an IOL diameter of 4.3 mm and has an outer bifocal ring from 4.3 and 6 mm. In the central 4.3 mm diameter, the IOL provides a near addition of +3.33 D and an intermediate addition of +1.66 D, both calculated at the IOL plane. The addition power between the diameters of 4.3 and 6 mm is +3.75 D (bifocal AT LISA model). The IOL is available in spherical powers from 0.0 to 32.0 D in 0.5-D increments. The company-labeled A constant for this IOL is 118.6.
IOL power was calculated by using three established formulae: SRK/T, Holladay II, and Haigis. The newer generation formulae – Haigis and Holladay II – performed well across a very wide range of axial lengths.Citation12 They were combined to calculate the IOL power in emmetropic eyes; the SRK/T was excellent for long myopic eyes, and Haigis formula for hyperopic eyes.Citation13 The refractive target was emmetropia to −0.25 D in all cases. All values were obtained by using partial coherence interferometry (IOLMaster 500; Carl Zeiss Meditec AG).
Surgical technique
All surgeries were performed by a single experienced surgeon (SG) under topical anesthesia. A standardized surgical technique was employed by using a 2.8 mm temporal clear corneal incision. After phacoemulsification, the foldable trifocal IOL was injected in the capsular bag through a 5.5 mm capsulorhexis. Postoperative topical therapy included a combination of antibiotic, steroidal, and nonsteroidal anti-inflammatory agents.
Postoperative examinations were performed at 1 day, 1 week, 1 month, 6 months, and 12 months and included the same tests performed as in the preoperative assessment. At every visit, logMAR acuity charts were used to evaluate distance visual acuity. Logarithmic visual acuity charts were used to assess near visual acuity at 40 cm.
Reading performance was evaluated by using the SRD (University Eye Clinic, Paracelsus Medical University of Salzburg, Austria), which provides for controlled reading distance and automated calculation of the reading speed and logarithmic reading acuity. At each postoperative follow-up from 1 month onward, reading acuity, reading speed (speed associated with maximum reading acuity), and the smallest print size that could be read with a minimum reading speed of 80 words per minute (wpm), which represents the lower limit for recreational sense-capturing reading, were evaluated.Citation14,Citation15 All measurements of reading performance were performed with and without distance correction.
Contrast sensitivity was tested from 1 month onward until the last visit binocularly with distance correction under mesopic conditions at spatial frequencies of 1.5, 3, 6, 12, and 18 cycles per degree using the functional acuity contrast rest (F.A.C.T. Stereo Optical Co., Inc., Chicago, IL, USA).
Preoperatively, patients were shown pictures representing dysphotopic phenomena, specifically halos, glare, and starbursts, and were informed about their occurrence and meaning. On all postoperative visits from 1 to 12 months, the same pictures were shown and the patients were asked to classify each of these three visual symptoms according to a 5-point scale (0= no trouble; 1= minimal trouble; 2= moderate trouble; 3= considerable trouble; 4= overwhelming trouble). Total score of all three complaints (halos, glare, and starbusts) was analyzed for each patient (maximum score =12, minimum =0). Also, at the same visit, all patients were asked to answer the question “Do you wear glasses or feel the need to wear glasses for activities like watching television, working on computer or reading?” They were asked to choose one of the responses – yes or no.
At the 12-month visit, the binocular defocus curve was evaluated under photopic conditions (85 cd/m2) by using defocusing lenses from +1.00 to −4.00 D in 0.50 D steps.
Statistical analysis
Statistical analysis was performed by using Excel spread-sheet software (Microsoft Corp., Redmond, WA, USA). The paired t-test was used to compare the mean preoperative and postoperative visual acuity. The statistical significance of any intergroup contrast sensitivity differences was assessed with a paired t-test at each frequency. A P-value of ≤0.05 was considered statistically significant.
Results
The study group comprised 50 eyes from 25 patients, with a mean age of 58±13.44 years, who underwent bilateral cataract surgery with implantation of trifocal IOL. There were 14 (56%) males and 11 (44%) females treated. All patients completed the 12-month follow-up. No eye was excluded from the analysis because of intraoperative or postoperative complications.
Distance visual acuity and refraction
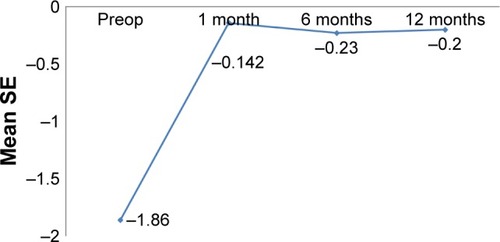
shows the postoperative visual and refractive outcomes at 1 month, 6 months, and 12 months. All patients had significant improvement in binocular UDVA and CDVA after surgery compared to preoperative values (P<0.01). Postoperatively, the UDVA and CDVA did not change significantly between 1 month, 6 months, and 12 months (P=0.07). shows the cumulative percentage of eyes with logMAR UDVA and CDVA, 12 months after the surgery, and 98% eyes (49/50) had UDVA of ≤0. The UDVA was ≤0.2 logMAR in all 50 (100%) eyes. All eyes achieved ≤0.1 logMAR CDVA. The UNVA and DCNVA at 40 cm also showed similar trends and was ≤0.1 logMAR in all 50 (100%) eyes at 12 months ().
Figure 1 Cumulative bar graph for distance visual acuity at 12 months.
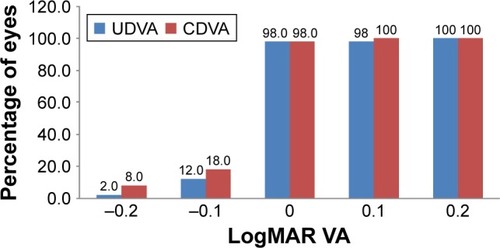
Figure 2 Cumulative bar graph for binocular near visual acuity at 12 months.
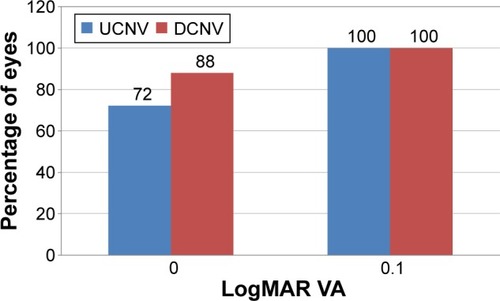
Table 1 Distant and near visual acuity at 1, 6, and 12 months postoperatively
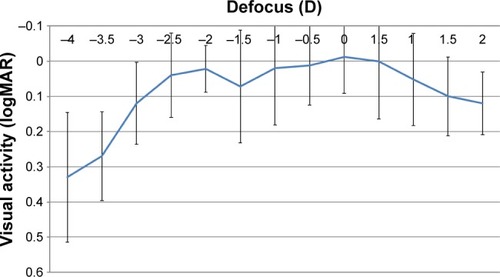
Stability of spherical equivalent (SE) refraction over time
There was a statistically significant reduction in SE after surgery (P<0.05). However, there were no statistically significant differences in SE between 1 month, 6 months, and 12 months postoperatively (P>0.05) ().
Binocular reading acuity and reading speeds at 70, 80, and 90 cm
Uncorrected and distance-corrected binocular reading acuity assessed at 1, 6, and 12 months showed best results at the distance of 80 cm compared with 70 and 90 cm at all visits. The differences were significant at 1-month follow-up, while at 6-month and 1-year follow-up, only the difference between reading acuity at 70 and 80 cm was found to be significant. Reading acuity improved over time, being best at 12 months, and this finding was statistically significant at 70 and 90 cm (). However, at 12 months through all distances, the range of uncorrected and distance-corrected visual acuity remained between 0.044±0.058 to 0.09±0.072 and 0.034±0.056 to 0.069±0.084 logMAR units, respectively. A similar trend was observed for the reading speeds, being best at 80 cm and improving over time. However, the changes were not statistically significant. At 6 months, there was a nonsignificant drop in both uncorrected reading acuity and reading speeds compared with 1 month for all distances which improved by 12 months.
Table 2 Reading acuity and reading speed over time
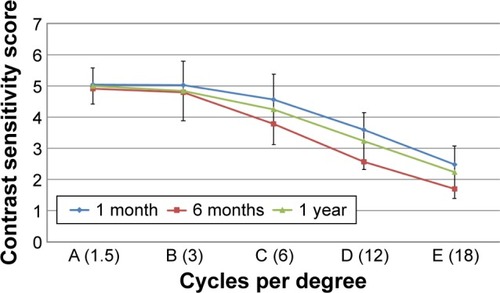
Defocus curves
shows the binocular mean defocus curves under mesopic conditions. The best visual acuity results were obtained at 0.00 D defocus equivalent to distance vision. A second peak was observed at −2.00 D, corresponding to good near vision. In the intermediate zone, no distinct peak was observed. However, in this interval, the curve was in the zone of 0.1 logMAR or better visual acuity without a sharp drop which corresponds to useful vision at intermediate distance.
Contrast sensitivity
shows the binocular contrast sensitivity under mesopic conditions at 1 month, 6 months, and 12 months postoperatively. At 6 months, slight reduction in contrast sensitivity was seen at higher spatial frequencies of 12 and 18 cpd; however, the difference was not statistically significant. At 12 months, the contrast sensitivity was comparable to 1-month values at all spatial frequencies (P>0.05).
Dysphotopic phenomena and spectacle independence evaluation
shows the mean dysphotopsia scores, which showed continuous improvement over time, being significantly lowest at 12 months (P<0.05). One patient reported a score of 3 (considerable trouble) for halos and glare each at 1 month which reduced at 6 months to 2 and 1, respectively. No patient reported a score of 4 (overwhelming trouble) for any visual symptoms evaluated. All patients reported 100% spectacle freedom for distance (watching television), intermediate (working on computer), and reading ().
Table 3 Patient satisfaction – dysphotopsia score and spectacle independence at 1, 3, and 12 months postoperatively
Long-term complications
Five out of the total 50 eyes developed PCO, requiring YAG capsulotomy at a mean follow-up time of 6.7 months. Three eyes had visually significant PCO, warranting YAG capsulotomy. However, in the remaining two eyes, the main indication of YAG capsulotomy was not the mild PCO, but a significant drop in contrast sensitivity, while the visual acuity in these eyes did not significantly change, compared to 1-month values. Apart from PCO, no other visually significant complications such as cystoid macular edema, post op uveitis, or glaucoma occurred in any of the study eyes at the end of 12 months.
Discussion
Visual and refractive outcomes of AT LISA trifocal IOLs have been evaluated in various studies. These IOLs provide three main foci in order to improve intermediate vision.Citation14,Citation15 Recently, Mojzis et al evaluated 1-year outcomes with AT LISA trifocal IOLs.Citation11 In their study, from 1 to 12 months, significant changes were observed in sphere showing slight but statistically significant hyperopic shift over time. In contrast, slight myopic shift of SE over time was observed; however, it was not statistically significant. These changes may also be explained by changes in effective lens position due to capsular contraction.Citation16
Posterior capsular opacification rate was similar in both studies (Mojzis et al – 15.8% and present study – 16%); however, the YAG capsulotomy rate in the present study was much higher (10% vs 3.3%). The possible reason could be that some patients required early YAG capsulotomy due to reduction in contrast, although the PCO was not clinically significant.
In their study, they did not find significant differences for intermediate visual acuity between 66 and 80 cm; however, in this study, reading acuity was significantly better at 80 cm compared with 70 and 90 cm.Citation11 These differences could be explained by the fact that in the present study, reading acuity was assessed with SRD, which is proposed to be a more realistic method compared with the conventional Early Treatment Diabetic Retinopathy study charts as used in their study.Citation17
Previously, this instrument has been used to compare bilateral reading performance within the first 6 months after implantation of four IOL models.Citation18,Citation19 It was found that multifocal IOLs with a diffractive component provided a comparable reading performance that was significantly better than the one obtained with refractive multifocal and monofocal IOLs. Although the visual and refractive outcomes of AT LISA tri 839MP IOL have been compared with other trifocal IOLs, the functional vision and reading speeds between the two models were not compared.Citation20
Intermediate visual acuity was not recorded using the conventional charts since they assess reading visual acuity only, which is a limited predictor of performance of real-world tasks. This was the reason leading to the development of reading performance, based on tests such as SRD, which are designed to simultaneously measure reading acuity and speed.
Attia et al recently evaluated reading acuity and reading speeds with the Physiol Fine vision trifocal IOL using the SRD.Citation21 In their study, binocular uncorrected reading acuity and reading speed at 80 cm was 0.11 logMAR and 98 wpm, respectively, whereas in the present study both the reading acuity and reading speed at 80 cm showed better results (reading acuity 0.044 logMAR and reading speed 169 wpm). However, they also evaluated reading acuity and speed at preferred distances and found the preferred distance at 64 cm. In this study, reading speeds and acuity at 70 cm are comparable to their preferred distance; however, best results were obtained at 80 cm. This may be attributed to differences in design of the IOLs and difference in the light distribution at near intermediate and distance and variation in amount of near addition. Also, the sample size in their study was 11 patients in contrast to the present study (25 patients), leading to variability in the interpretation of statistical results.
This study did not evaluate reading acuity and speed at preferred distances, which may be a potential limitation of this study. However, Attia et al did not evaluate the effect of PCO and incidence of YAG in their study, which had a mean follow-up of 15.77 months. Occurrence of PCO may affect the reading performance as observed in our study, where reading performance improved after YAG capsulotomy. Mild, nonsignificant drop in the reading acuity, reading speeds, and contrast sensitivity scores was observed at all distances at a mean follow-up period of 6 months, which were attributed to the development of mild PCO. However, after YAG capsulotomy, all eyes showed improvement in these parameters and subjective symptoms at the end of 1-year follow-up. Improvement in the maximum corrected reading acuity and reading speed with time was also observed, both being highest at the end of 12 months. This can partially be attributed to neural adaptation to the multiple foci generated by the trifocal IOL and the learning curve effect that occurs when patients take the same test again.
At 1 year, all patients achieved excellent reading acuities and reading speeds at 70, 80, and 90 cm corresponding to the usual intermediate distances. These parameters at 70, 80, and 90 cm distances to account for most of the intermediate range activities were evaluated, such as working on computer, in the kitchen, and other household tasks, and also inter-person differences in body height and arm length. The uncorrected reading function was best at 80 cm; however, it was 0.09 to 0.04 logMAR units for 70 and 90 cm, suggesting the excellent performance of the IOL over complete range of intermediate distance. These findings support the claim of better intermediate visual performance with diffractive-based trifocal IOLs.Citation19
One potential limitation of the study could be that the pupil size before and after the surgery was not measured while performing postoperative tests. However, pupil size has a direct influence on the outcomes with full-refractive IOLs.Citation5,Citation6 AT LISA TRI being a diffractive and pupil independent IOL provided excellent outcomes across all range of distances in the current study.Citation14
Conclusion
The AT LISA trifocal IOLs seemed to provide excellent distance, intermediate, and very good near vision in the long-term follow-up. Yag capsulotomy for early PCO and drop in contrast sensitivity did not seem to have affected visual outcomes significantly. Standardized measurement of reading performance by using the SRD allowed more realistic and practical assessment of patient’s acceptance to trifocal IOL implantation after cataract surgery.
Disclosure
This investigator led study was partly supported by Carl Zeiss Meditec AG, ZEISS Group. The authors report no other conflicts of interest in this work.
References
- AlioJLMontalbanRPena-GarciaPSoriaFAVega-EstradaAVisual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgeryJ Refract Surg2013291175676124203807
- VoskresenskayaAPozdeyevaNPashtaevNBatkovYTreushnicovVCherednikVInitial results of trifocal diffractive IOL implantationGraefes Arch Clin Exp Ophthalmol201024891299130620526609
- JavittJCSteinertRFCataract extraction with multifocal intraocular lens implantation: a multinational clinical trial evaluating clinical, functional, and quality-of-life outcomesOphthalmology2000107112040204811054329
- JavittJBrauweilerHPJacobiKWCataract extraction with multifocal intraocular lens implantation: clinical, functional, and quality-of-life outcomes. Multicenter clinical trial in Germany and AustriaJ Cataract Refract Surg20002691356136611020621
- SalatiCSalvetatMLZeppieriMBrusiniPPupil size influence on the intraocular performance of the multifocal AMO-array intraocular lens in elderly patientsEur J Ophthalmol200717457157817671933
- ArtigasJMMenezoJLPerisCFelipeADíaz-LlopisMImage quality with multifocal intraocular lenses and the effect of pupil sizeJ Cataract Refract Surg200733122111211718053913
- MaxwellWALaneSSZhouFPerformance of presbyopia-correcting intraocular lenses in distance optical bench testsJ Cataract Refract Surg200935116617119101440
- MesciCErbilHOzdokerLKarakurtYBilgeADVisual acuity and contrast sensitivity function after accommodative and multifocal intraocular lens implantationEur J Ophthalmol20102019010019882523
- GatinelDHoubrechtsYComparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical benchJ Cataract Refract Surg20133971093109923692884
- JonkerSMRBauerNJCMakhotkinaNYBerendschotTTJMvan den BiggelaarFJHMNuijtsRMMAComparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trialJ Cataract Refract Surg20154181631164026432120
- MojzisPMajerovaKHrckovaLPineroDPImplantation of a diffractive trifocal intraocular lens: one-year follow-upJ Cataract Refract Surg2015411623163026432119
- DonosoRMuraJJLopezMPapicAEmmetropization at cataract surgery. Looking for the best IOL power calculation formula according to the eye lengthArch Soc Esp Oftalmol2003789477480 Spanish14517733
- GhanemAAEl-SayedHMAccuracy of intraocular lens power calculation in high myopiaOman J Ophthalmol20103312613021120048
- GatinelDPagnoulleCHoubrechtsYGobinLDesign and qualification of a diffractive trifocal optical profile for intraocular lensesJ Cataract Refract Surg201137112060206722018368
- Madrid-CostaDRuiz-AlcocerJFerrer-BlascoTGarcia-LazaroSMontes-MicoROptical quality differences between three multifocal intraocular lenses: bifocal low add, bifocal moderate add, and trifocalJ Refract Surg2013291174975424203806
- NanavatyNARajSMVasavadaVAVasavadaAVasavadaARAnterior capsule cover and axial movement of intraocular lensEye2008221015102317464305
- DexlAKSchlögelHWolfbauerMGrabnerGDevice for improving quantification of reading acuity and reading speedJ Refract Surg20102668268819968188
- RaspMBacherneggASeyeddainOBilateral reading performance of 4 multifocal intraocular lens models and a monofocal intraocular lens under bright lighting conditionsJ Cataract Refract Surg201238111950196123079311
- AlioJLGrabnerGPlaza-PucheABPostoperative bilateral reading performance with 4 intraocular lens models: six-month resultsJ Cataract Refract Surg201137584285221511152
- MarquesEFFerreiraTBComparison of visual outcomes of 2 diffractive trifocal intraocular lensesJ Cataract Refract Surg201541235436325661129
- AttiaMSAuffarthGUKhoramniaRLinzKKretzFTNear and intermediate reading performance of a diffractive trifocal intraocular lens using a reading deskJ Cataract Refract Surg2015412707271426796451