Abstract
Purpose
The purpose of this study was to compare the short-term changes in retina and choroidal tissue after femtosecond laser-assisted cataract surgery (FLACS) and standard phacoemulsification (PE) surgery.
Methods
In all, 25 eyes undergoing FLACS and 27 eyes undergoing PE surgery were included in this nonrandomized, retrospective, cross-sectional study. Central retinal thickness (CRT) and choroidal thickness (CT) were measured pre- and postoperatively (at day 1, 1 week later, and after 1 month) with spectral domain optical coherence tomography (OCT) in all patients and were compared. For group comparisons, chi-square test and independent t-test were used. Postoperative values were compared to the baseline using a paired t-test. The magnitude of the change from baseline to the peak was analyzed by multiple regression models in an attempt to explain possible influence variables.
Results
Pre and postoperative CRT measurements were similar in both groups. The mean subfoveal CT at day 1, after 1 week, and 1 month were significantly higher than baseline CT measurements in the PE group.
Conclusion
FLACS might have an advantage in regard to postoperative choroidal changes.
Introduction
Phacoemulsification (PE) technique has become the standard of care due to its faster rehabilitation and lower complication rates in cataract surgery. Despite advances in PE technique, pseudophakic cystoid macular edema (PCME) is still one of the most common causes of vision loss following surgery.Citation1 Although the exact pathogenesis of PCME is not clear, multifactorial pathogenesis including the release of inflammatory mediators such as prostaglandins, light toxicity, and mechanical irritation are thought to cause a breakdown of the blood–aqueous barrier and the blood–retinal barrier, thus producing increased vascular permeability and macular edema.Citation2,Citation3 In most cases, PE does not change the macroscopic fundus appearance of the retina. However, increase in central retinal thickness (CRT), even without PCME, after uneventful cataract surgery has become a safety concern for this frequently performed operation.Citation4–Citation6 Changes in subfoveal choroidal thickness (CT) after uneventful cataract surgery are sparsely studied with varying results.Citation6–Citation9
Femtosecond laser-assisted cataract surgery (FLACS) was approved by the Food and Drug Administration in 2009 and is promising in terms of increased predictability and consistent results by offering automated steps during critical phases of cataract surgery.Citation10 FLACS also offers a decrease in cumulative dissipated energy that might reduce the release of inflammatory mediators within the aqueous chamber, which may result in less macular edema.Citation11,Citation12 Initial studies on the effect of FLACS surgery on macular thickness revealed promising results compared to standard PE.Citation13,Citation14 Standard PE and FLACS techniques have not yet been compared with a view to observe changes in postoperative CT, which could be important in developing PCME. From this point of view, short-term CRT and CT changes need to be evaluated after standard PE and FLACS with posterior chamber intraocular lens (IOL) implantation.
Materials and methods
This retrospective case series included patients with different grades (I–IV) of cataract who had uneventful FLACS and standard PE surgery. Patients who had FLACS were compared to those who had standard PE surgery in terms of the postoperative CRT and CT. All surgeries were performed by the same experienced surgeon (BSA) at Kaskaloglu Eye Hospital between January 2015 and March 2015. In line with the tenets of the Declaration of Helsinki, informed consent for FLACS and standard PE surgery was obtained from all patients who declared that they were able to comply with the treatment procedure and the follow-up schedule. Patient consent for review of their charts and records for the current study was not required by the Instutional Review Board of Van Education and Training Hospital because of the retrospective design of the study.
The Lens Opacities Classification System (LOCS) III grading score was used.Citation15 Preoperative LOCS score was estimated by an independent physician using a slit-lamp (Inami L-0185; Inami & Co, Tokyo, Japan) at maximum illumination without light filtering. Exclusion criteria were history of any ocular diseases and surgery, particularly those, which can cause changes in the macula. Since diabetes, hypertension, and cigarette smoking may well affect CT, those were excluded as well.
All patients underwent a full ophthalmic examination including best-corrected visual acuity (BCVA), slit-lamp evaluation, intraocular pressure measurement (Goldmann tonometry), macular and optic disc examination to exclude other ocular pathologies, and CRT and CT measurements by using high-resolution spectral domain optical coherence tomography (SD-OCT; 3D OCT-2000® Topcon; Topcon Corp., Tokyo, Japan). Preoperative and postoperative (at day 1, day 7, and 4 weeks after surgery) CRT and CT measurements were components of standard examination for cataract patients in the present clinic. The differences of CT and CRT were corrected for the resolution limits of the OCT device used in the clinic. In order to calculate the power of IOL needed, biometry was conducted using optical (IOLMaster; Carl Zeiss Meditec Inc, Jena, Germany) and immersion (Ocuscan; Alcon Labs Inc, Fort Worth, TX, USA) techniques.
Procedure
All procedures were carried out under topical anesthesia with proparacaine hydrochloride 0.5% (Alcaine®; Alcon Labs Inc). Standard preoperative medications administered for pupillary dilation an hour before surgery were tropicamide 0.5% (Tropamide®; Bilim Ilac, Istanbul, Turkey), phenylephrine hydrochloride 0.25% (Mydfrin®; Alcon Labs Inc), and nepafenac 0.1% ophthalmic suspension (Nevanac®; Alcon Labs Inc).
In the FLACS group, femtosecond laser procedure was performed using the LenSx laser system with the SoftFit™ interface (version 2.20 software, Laser SoftFit™; Alcon Labs Inc). The LenSx laser is a 50 kHz infrared laser with a pulse width of 600–8,002 femtosecond, a central laser wavelength of 1,030 nm, and a maximum pulse energy of 15 mJ. The SoftFit™ patient interface has an additional soft contact lens between the corneal surface and the curved interface. The interface surface had a diameter of 10.8 mm and a curvature of 8.3 mm. This disposable patient interface was docked to the eye and the individual patient treatment was programmed into the laser system. The system automatically imaged the ocular structures with the integrated OCT imaging system and determined the treatment parameters. All patients in the FLACS group had capsulotomy, lens fragmentation, and corneal incisions by the laser. A 5 mm diameter capsulotomy with pupil centration was created by scanning a cylindrical pattern as ablation pattern. Hybrid pattern (the central 2.5 mm core liquefied and the peripheral parts fragmented into four parts with two cuts) was used as the fragmentation pattern. A 2.40 mm three-plane trapezoidal primary incision and two 1.20 mm 30°-angled secondary incisions were created. Parameters included laser pulse energy at 7 mJ for corneal incisions and 5 mJ for capsulotomy and lens fragmentation.
The PE group underwent conventional cataract surgery. A 2.40 mm main corneal incision with a metal keratome and continuous curvilinear capsulorrhexis using rhexis forceps were performed before PE.
After hydrodissection, PE was performed using the Infiniti system® (Alcon Labs Inc) in both groups. Lens segmentation was undertaken in both groups using a quick chop approach. In all cases, after removal of the lens cortex, a foldable IOL was implanted uneventfully in the capsular bag.
Intraoperative measurements included determining the effective PE time (EPT). The EPT is measured in seconds and represents the total PE time multiplied by the average percentage power used. It is a metric of the length of PE time at 100% power in continuous mode.
CRT and subfoveal CT were measured preoperatively, on the first day, first week, and the first month postoperatively, by using high-resolution SD-OCT (3D OCT-2000® Topcon) with 6 mm single line scanning (λ=840 nm, 27.000 A-scans/s, and 5 μm axial resolution). All CT and CRT measurements were performed by one grader (EK) and the grader was masked for the surgery method. The protocol of the enhanced choroidal mode cross scan was conducted centering on the fovea as described previously.Citation16 Scans with low quality and blinks were not included and were repeated. In order to avoid the circadian change in CT measurements, all measurements were performed at the same time of the day (between 08:00 and 09:00 am). For each eye, CT and CRT were measured three times repeatedly at regular intervals of 20 minutes and the mean values were recorded. Eyes with >5% difference between three measurements were excluded from the study.
The standard postoperative regimen included one drop each of 0.5% moxifloxacin (Vigamox; Alcon Labs Inc), nepafenac 0.1% ophthalmic suspension (Nevanac; Alcon Labs Inc), and 0.1% dexamethasone ophthalmic suspension (Maxidex; Alcon Labs Inc) four times a day for 2 weeks and was the same for both groups. Steroid drops then were reduced to twice daily for another week. The patients were followed up at day 1, day 7, and 4 weeks after surgery.
Data were extracted from patient charts and surgical videos, which included preoperative and postoperative corrected distance visual acuity, cataract grading, and preoperative and postoperative CRT and CT. Intraoperative measurements included EPT. Patient charts and findings were analyzed retrospectively.
Statistical analysis
Statistical analysis was performed with SPSS for Windows 16.0 (SPSS Inc., Chicago, IL, USA). For intergroup comparisons, chi-square test and independent t-test were used. Power calculation was carried out for CT and CRT by using SPSS general linear model repeated measures section. The magnitude of the change from baseline to the peak was analyzed with possible explanatory variables by multiple regression models. A P-value <0.05 was considered statistically significant.
Results
The FLACS group comprised 25 eyes of 25 patients who had undergone FLACS. The mean age of the 16 female and 9 male patients was 70.5±6.7 years (range 59–84 years). The PE group comprised 27 eyes of 27 patients who had undergone standard PE surgery. The mean age of the 17 female and 10 male patients was 70.2±9.6 years (range 51–90 years) ().
Table 1 Preoperative characteristics of the patients
Mean cataract grade was 2.81±0.65 in the FLACS group and 2.78±0.71 in the PE group, with no statistically significant differences between the groups. The EPT was 1.98±1.01 seconds in the FLACS group and 4.23±1.96 seconds in the PE group. The EPT was statistically significantly lower in the FLACS group (P<0.0001). There was no correlation between EPT and the difference of CT compared with basal CTs at day 1 (r=0.13, P=0.36), week 1 (r=0.18, P=0.20), and month 1 (r=0.06, P=0.70).
One month following surgery, the inflammation indicated by the presence of cells or flares in the anterior chamber disappeared in all patients. There was no complication in the postoperative course of any patient. There was no significant difference between the two groups in terms of age, preoperative BCVA (P=0.35), refractive errors (P=0.36), axial length (P=0.66), anterior chamber depth (P=0.76), intraocular pressure (P=0.72), preoperative CRT (P=0.31), or preoperative subfoveal CT (P=0.48) (). No PCME or subretinal fluid developed in any patient.
Mean preoperative and postoperative CRT and CT values are shown in . CRT was not different in any visit compared with baseline retinal thickness in both groups. In the FLACS group, there was no significant difference between baseline CT and postoperative CT values (P=0.37, 0.10, and 0.59). In the PE group, the mean subfoveal CT 1 day, 1 week, and 1 month after surgery were significantly higher compared with the baseline CT (P=0.003, 0.02, and 0.02, respectively) ( and , ). Observed power was 0.849 for CT, 0.323 for CRT.
Figure 1 Choroidal thickness increased significantly in the phacoemulsification (PE) group but did not change in the femtosecond laser-assisted cataract surgery (FLACS) group.
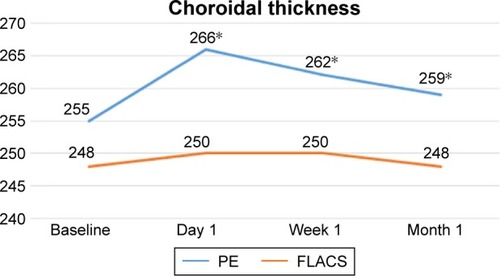
Table 2 Preoperative and postoperative values of CRT and CT
Table 3 Results of paired t-test in femtosecond laser-assisted cataract surgery group
Table 4 Results of paired t-test in phacoemulsification group
Multiple regression analysis revealed that age, gender, spherical equivalent, axial length, anterior chamber depth, intraocular pressure, baseline CRT, and baseline CT were not predictors of significant choroidal thickening at day 1, week 1, or month 1 in the PE group ().
Table 5 Multiple regression analysis of CT difference at day 1, week 1, and month 1 in phacoemulsification group
Discussion
Proposed etiologic factors of PCME include inflammation, vitreous traction, and hypotony.Citation17 Of these, the core mechanism is likely surgically induced anterior segment inflammation that results in the release of endogenous inflammatory mediators. A critical threshold of inflammatory mediators in the aqueous is likely required for detectable edema.
PCME is estimated to occur in 20%–30% of patients undergoing PE, based on fluorescein fundus angiography findings.Citation3,Citation18,Citation19 OCT-based studies suggest that this rate ranges from 4% to 11%,Citation20,Citation21 but may be up to 41% in 6 weeks following surgery.Citation4 Since the majority of these patients do not experience any visual disturbances,Citation18 the term “clinical PCME” was coined, and is defined as symptomatic vision loss of 20/40 or worse, and is seen much less frequently with today’s surgical techniques, at a rate of ~0.1%–2.35%.Citation22,Citation23 However, macular thickness changes without the development of PCME have been reported in many studies.Citation4,Citation6–Citation8
In the current study, CRT did not change in the PE group after surgery. Though most studies in the literature described a significant increase in CRT after standard PE surgery,Citation4–Citation6,Citation8,Citation13,Citation14,Citation21,Citation24–Citation26 the majority of these studies found no correlation between BCVA and the amount of thickness change. Yet, a few reports found an insignificant change in CRT after standard PE surgery.Citation27 Some studies reported that the changes started early after PE surgery (within the first week)Citation13,Citation21,Citation26 and progressively increased until the first month after PE surgery.Citation6,Citation8,Citation21,Citation26 Other studies reported a progressive increase in the macular thickness until 6–12 weeks after PE surgery.Citation4,Citation5,Citation25
CRT did not differ postoperatively in the FLACS group in the current study. Ecsedy et al compared the effect of standard PE and FLACS on the macular thickness within the first month after surgery.Citation13 They found a significantly higher macular thickness in the PE group 1 week after cataract surgery compared to the FLACS group, but this difference decreased and became only marginally significant 1 month after surgery.Citation13 Similarly, Nagy et al described macular edema mainly in the outer nuclear layer in both the PE and FLACS groups, but the macular thickness was significantly less after FLACS.Citation14
A recent study described an acute expression of pro-inflammatory genes and proteins in the neurosensory retina as well as in the choroid of mice undergoing lens extraction (with increased expression of IL-1β within the retina pigment epithelium/choroid of both operated eyes and fellow eyes compared with unoperated control eyes).Citation28 This led investigators to search for a possible role of choroid in the inflammatory reaction after cataract surgery. The CT increased significantly 1 day, 1 week, and 1 month after PE surgery in the current study. This is in accordance to most relevant studies, which found an increase in CT after standard PE surgery.Citation7–Citation9 For instance, Ohsugi et al found an increase in CT, which continued 6 months after surgery and was negatively correlated with increased intraocular pressure and axial length.Citation7 Pierru et al described an increase in CT starting 1 day after surgery and continuing until 3 months after surgery.Citation8 They also found a negative correlation between CRT and increased age and increased axial length. Noda et al also found an increase in CRT after standard PE, which continued until 6 months after surgery with a larger increase in male patients and patients with a thicker baseline subfoveal CT.Citation9 In contrast, Falçao et al described an insignificant change in CT after PE surgery in a smaller series.Citation6 Regression analysis was also performed in the current study, but no correlation was found between age, gender, spherical equivalent, axial length, anterior chamber depth, intraocular pressure, baseline CRT, baseline CT, and changes in CT.
FLACS demonstrated somewhat better results over standard PE surgery regarding CRT, as described in this study and elsewhere.Citation13,Citation14 Yet, little is known about the effects of FLACS on CT; so it is believed that this rare study of its kind, which compares the results with standard PE surgery, sheds new light on the effects of FLACS. The fact that there was no change in CT 1 day, 1 week, and 1 month after FLACS may suggest that FLACS is also safe for subretinal tissues in the subfoveal area. Reducing surgically induced inflammation and trauma may decrease the incidence of PCME. Several studies have reported significant reductions in EPT using the femtosecond laser technique compared with the conventional technique.Citation29,Citation30 In the present study, the EPT was also statistically significantly lower in the FLACS group. However, results showed no correlation between EPT and the difference of CT in this study. The difference between postoperative CTs in FLACS and standard PE groups cannot be explained by EPT, although EPT was significantly different between FLACS and standard PE groups.
With lower EPT values, FLACS may offer more advantages than standard PE surgery in terms of postoperative retinal thickness and CT. Other surgical measures such as cumulative dissipated energy, ultrasound total time, and total time under microscope light and laser are needed for comparison with further studies.
This study has limitations that should be addressed. The sample size was small, representing results at a single center. Another weakness was the short follow-up period. Although most changes in CRT occur within the first month after surgery according to relevant studies in the literature, further follow-up might still be required to determine the effect of FLACS and standard ultrasound technique on retinal and choroidal tissues.
In conclusion, CT was more affected when using the standard PE technique rather than FLACS. The comparatively lower effect of FLACS on CT may be important to reduce the incidence of PCME. The small sample size is a serious limitation of this study. Especially, the observed power for CRT weakens the statistical power of the study. Prospective design with a bigger sample size is needed to find meaningful differences with respect to PCME. Although this may have no importance in standard patients, similar prospective trials are needed to assess the effects of the two methods on posterior segment structures, especially for those with comorbidities such as age-related macular degeneration (AMD) or uveitis in view of the recent publicity regarding a potential association between cataract surgery and late AMD.Citation31–Citation36
Acknowledgments
The Institutional Review Board of Van Education and Training Hospital approved this study (affirmation number: 2017/2).
Disclosure
The authors report no conflicts of interest in this work.
References
- YonekawaYKimIKPseudophakic cystoid macular edemaCurr Opin Ophthalmol2012231263222134362
- HudesGRLiWYRockeyJHWhitePProstacyclin is the major prostaglandin synthesized by bovine retinal capillary pericytes in cultureInvest Ophthalmol Vis Sci19882910151115163049428
- GuoSPatelSBaumrindBManagement of pseudophakic cystoid macular edemaSurv Ophthalmol201560212313725438734
- LoboCLFariaPMSoaresMABernardesRCCunha-VazJGMacular alterations after small-incision cataract surgeryJ Cataract Refract Surg200430475276015093635
- CaginiCFioreTIaccheriBPiccinelliFRicciMAFruttiniDMacu-lar thickness measured by optical coherence tomography in a healthy population before and after uncomplicated cataract phacoemulsification surgeryCurr Eye Res200934121036104119958122
- FalcãoMSGonçalvesNMFreitas-CostaPChoroidal and macular thickness changes induced by cataract surgeryClin Ophthalmol20148556024368877
- OhsugiHIkunoYOharaZChanges in choroidal thickness after cataract surgeryJ Cataract Refract Surg201440218419124360848
- PierruACarlesMGastaudPBaillifSMeasurement of subfoveal choroidal thickness after cataract surgery in enhanced depth imaging optical coherence tomographyInvest Ophthalmol Vis Sci20145584967497425052991
- NodaYOgawaAToyamaTUetaTLong-term increase in subfoveal choroidal thickness after surgery for senile cataractsAm J Ophthalmol2014158345545924875000
- NagyZZNew technology update: femtosecond laser in cataract surgeryClin Ophthalmol201418811571167
- PalankerDVBlumenkranzMSAndersenDFemtosecond laser-assisted cataract surgery with integrated optical coherence tomographySci Transl Med20102585885
- Conrad-HengererIHengererFHSchultzTDickHBEffect of femtosecond laser fragmentation on effective phacoemulsification time in cataract surgeryJ Refract Surg2012281287988323231739
- EcsedyMMihaltzKKovacsITakacsAFilkornTNagyZZEffect of femtosecond laser cataract surgery on the maculaJ Refract Surg2011271071772221877677
- NagyZZEcsedyMKovácsIMacular morphology assessed by optical coherence tomography image segmentation after femtosecond laser-assisted and standard cataract surgeryJ Cataract Refract Surg201238694194622624892
- ChylackLTJrWolfeJKSingerDMThe Lens Opacities Classification System III. The Longitudinal Study of Cataract Study GroupArch Ophthalmol199311168318368512486
- YamashitaTYamashitaTShirasawaMArimuraNTerasakiHSakamotoTRepeatability and reproducibility of subfoveal choroidal thickness in normal eyes of Japanese using different SD-OCT devicesInvest Ophthalmol Vis Sci20125331102110722247474
- WolterJRThe histopathology of cystoid macular edemaAlbrecht Von Graefe’s Arch Klin Exp Ophthalmol1981216851016910356
- UrsellPGSpaltonDJWhitcupSMNussenblattRBCystoid macular edema after phacoemulsification: relationship to blood–aqueous barrier damage and visual acuityJ Cataract Refract Surg199925111492149710569164
- GulkilikGKocaboraSTaskapiliMEnginGCystoid macular edema after phacoemulsification: risk factors and effect on visual acuityCan J Ophthalmol200641669970317224950
- BelairMLKimSJThorneJEIncidence of cystoid macular edema after cataract surgery in patients with and without uveitis using optical coherence tomographyAm J Ophthalmol2009148112813519403110
- PerenteIUtineCAOzturkerCEvaluation of macular changes after uncomplicated phacoemulsification surgery by optical coherence tomographyCurr Eye Res200732324124717453944
- HendersonBAKimJYAmentCSFerrufino-PonceZKGrabowskaACremersSLClinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatmentJ Cataract Refract Surg20073391550155817720069
- LoewensteinAZurDPostsurgical cystoid macular edemaDev Ophthalmol20104714815920703048
- CapellaMJBarraquerEEstudio comparativo entre cirugía de catarata por microincisión coaxial y facoemulsificación estándar [Comparative study of coaxial microincision cataract surgery and standard phacoemulsification]Arch Soc Esp Oftalmol2010858268273 Spanish21130942
- KusbeciTEryigitLYavasGInanUUEvaluation of cystoid macular edema using optical coherence tomography and fundus fluorescein angiography after uncomplicated phacoemulsification surgeryCurr Eye Res201237432733322440164
- SariESErmisSSYaziciAKoytakASahinGKilicAThe effect of intracameral anesthesia on macular thickness and ganglion cell-inner plexiform layer thickness after uneventful phacoemulsification surgery: prospective and randomized controlled trialGraefes Arch Clin Exp Ophthalmol2014252343343924390400
- GhoshSRoyIBiswasPNProspective randomized comparative study of macular thickness following phacoemulsification and manual small incision cataract surgeryActa Ophthalmol2010884102106
- XuHChenMForresterJVLoisNCataract surgery induces retinal pro-inflammatory gene expression and protein secretionInvest Ophthalmol Vis Sci201152124925520720227
- NagyZTakacsAFilkornTSaraybaMInitial clinical evaluation of an intraocular femtosecond laser in cataract surgeryJ Refract Surg200925121053106020000286
- AbellRGKerrNMVoteBJToward zero effective phacoemulsification time using femtosecond laser pretreatmentOphthalmology201312094294823465860
- WangJJFongCSRochtchinaERisk of age-related macular degeneration 3 years after cataract surgery: paired eye comparisonsOphthalmology2012119112298230322959104
- CasparisHLindsleyKKuoICSikderSBresslerNBSurgery for cataracts in people with age-related macular degenerationCochrane Database Syst Rev2012136CD006757
- KleinBEHowardKPLeeKEIyengarSKSivakumaranTAKleinRThe relationship of cataract and cataract extraction to age-related macular degeneration: the Beaver Dam Eye StudyOphthalmology201211981628163322578823
- CugatiSMitchellPRochtchinaETanAGSmithWWangJJCataract surgery and the 10-year incidence of age-related maculopathy: the Blue Mountains Eye StudyOphthalmology2006113112020202516935334
- WangJJKleinRSmithWKleinBETomanySMitchellPCataract surgery and the 5-year incidence of late-stage age-related maculopathy: pooled findings from the Beaver Dam and Blue Mountains eye studiesOphthalmology2003110101960196714522772
- ChewEYSperdutoRDMiltonRCRisk of advanced age-related macular degeneration after cataract surgery in the Age-Related Eye Disease Study: AREDS report 25Ophthalmology2009116229730319091420
