Abstract
Purpose
To determine adherence to face-down positioning (FDP) among patients who underwent vitrectomy and gas tamponade for macular hole (MH) repair.
Method
A total of 69 patients (37 females and 32 males) who underwent primary vitrectomy for MH repair were studied. Nurses recorded whether the patient complied with FDP each time they examined the patient. FDP score was obtained from the nursing records; patients were given a score of 1 if they complied with the FDP and 0 if they did not. The score was recorded four times per day for the first 3 postoperative days. A perfect FDP score was 12.
Results
The mean ± standard deviation of the FDP scores was 10.6±1.8 (range: 4–12). Overall, 32 (46.4%) patients scored a perfect 12, and 7 (10.1%) patients scored <8. Failure of the MH closure was observed in only one patient (1.4%), who showed the poorest adherence to FDP (score =4). Consequently, the closure rate in patients with FDP score <7 (2/3, 66.7%) was significantly lower than in patients with an FDP score ≥7 (66/66, 100%) (P<0.05, Fisher’s exact probability test).
Conclusion
While adherence to FDP after MH surgery was better than that observed after vitrectomy for rhegmatogenous retinal detachments in our previous study, the percentage of patients with FDP scores <8 did not differ. Statistically, the poor adherence to FDP can negatively impact the effectiveness of the surgery for MH repair.
Introduction
Face-down positioning (FDP) is a standard posture recommended for patients following vitrectomy and gas tamponade procedures during macular hole (MH) surgery.Citation1–Citation28 Patients find the FDP inconvenient, and so it is not readily tolerated; therefore, the optimal method and duration of the FDP have been debated for many years.Citation2–Citation28 Shortening the duration of the FDPCitation2,Citation5,Citation8,Citation10,Citation11,Citation14,Citation16,Citation17,Citation22 and adopting alleviated positioning, such as avoidance of the supine or face-up positioning by the patients,Citation6–Citation13,Citation15,Citation19,Citation20,Citation22–Citation25,Citation27,Citation28 have been proposed and statistically compared with strict FDP.Citation5,Citation7–Citation12,Citation21–Citation25,Citation27,Citation28 However, these studies lacked adherence controls, and the intervention was the advice given to the patients to maintain the positioning rather than the positioning itself.Citation21 Even if the same advice was given to all the patients, some patients complied strictly, whereas others did not. Therefore, the disclosure of the actual adherence scores will help access the necessity of FDP in the prognosis of MH surgery.
Recently, we investigated 127 patients who underwent vitrectomy for rhegmatogenous retinal detachment.Citation29 We observed that the adherence to FDP varied considerably among the patients and that some patients failed to maintain the FDP for nearly or more than half the prescribed the time. The purpose of this study was to determine the differences in adherence to FDP in patients with causative diseases and the impact of adherence on the prognosis after MH surgery.
Method
Methodology and subjects
We retrospectively examined the nursing records of patients who had undergone primary vitrectomy and gas tamponade for idiopathic MH at the Fujita Health University Hospital (Toyoake, Japan) for a period of 1 year between April 2012 and March 2013. A total of 69 patients (37 females and 32 males) were included. The nursing records included detailed information related to the adherence of the patients to FDP.
Surgery
All the patients who had signed consent forms for the surgery and FDP received instructions on FDP. Pars plana vitrectomy was performed by experienced surgeons. Further, each patient also underwent triamcinolone-assisted internal limiting membrane peeling of approximately two disc diameters, prophylactic phacoemulsification, intraocular lens implantation, a complete fluid-gas exchange, and gas tamponade with 20% sulfur hexafluoride.
Postoperatively, the patients were advised to maintain FDP as much as possible every day for at least 1 wk. After the second week, when the MH closure was confirmed by optical coherence tomography, some patients were advised only to avoid the face-up position until the disappearance of the intraocular gas.
Nursing records
If the patients underwent gas tamponade, this was indicated in the hospital chart. Each time the patient was examined, including the four routine ward rounds per day, the nurse recorded whether the patient had complied with FDP. The nurse instructed the patient to resume FDP. If patients were found sleeping in a position other than FDP, the nurse woke them and asked them to assume FDP.
Each time the patient was checked, the nurse entered the data regarding the patient adherence to FDP into a handheld terminal. The data were exported and stored in a digital hospital chart.
FDP Score
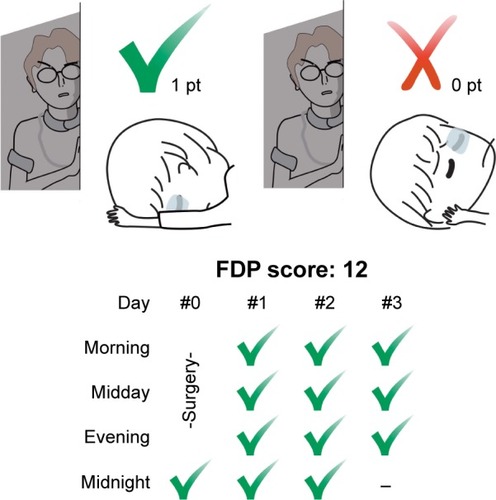
To quantify the patients’ adherence to FDP, the position of each patient was scored four times per day: at midnight, morning, midday, and evening, at approximately 24:00 h, 6:00 h, 12:00 h, and 18:00 h, respectively. Patient monitoring began at 24:00 h on the day of the surgery. Although the nurses continued these examinations until the gas disappeared or the patient was discharged, we only counted the score for the first 3 consecutive days in our initial attempt.Citation29 Consequently, a total of 12 observations were recorded, and the patients were given a score of 1 each time they followed FDP. Thus, a patient with perfect adherence would have a score of 12 ().
Figure 1 FDP score.
Abbreviation: FDP, face-down positioning.
Results
Outline and gender differences
shows the demographics of all the patients. The mean ± standard deviation of the FDP score was 10.6±1.8 (range, 4–12) for all the patients. The mean FDP score in female patients (10.9±1.5) was higher than that in males (10.3±2.1); however, this difference was not statistically significant (P>0.2, Mann–Whitney U test).
Table 1 Subjects and the FDP score
A total of 32 patients (46.4%) had a perfect score of 12, which included 19 (51.4%) females and 13 (40.6%) males. Seven patients (10.1%) were given low scores,Citation29 with an FDP score <8, including two females (5.4%) and five males (15.6%). There were more perfect scorers and fewer low scorers among female patients than that among male patients; however, there were no statistically significant differences between the males and females (P>0.37 and P>0.16, respectively, χ2 test).
Age analysis and individual observations
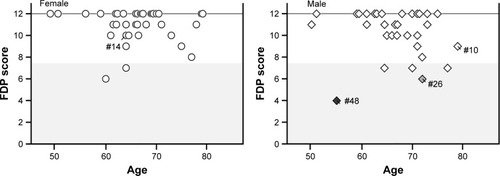
shows the distribution of the FDP score as a function of age. No significant correlation of the FDP score with age was observed, irrespective of sex.
Figure 2 Age distribution of the FDP score in females (left panel) and in male patients (right panel).
Abbreviations: FDP, face-down positioning; MH, macular hole.
Patients who failed to score a perfect 12 FDP score included a 79-year-old male (#10) with a score of 9 and a 64-year-old female (#14) with a score of 10. The lowest scorers included a 72-year-old male (#26) with a score of 6 and a 55-year-old male (#48) with a score of 4 (). As the patient did not follow FDP, the data regarding their actual body position are not available; however, there was some data available, for example, the patients often remained in the supine position or sitting upright position during the daytime hours.
Figure 3 FDP score of patients who failed to score a perfect 12: #10 represents a 79-year-old male with an FDP score of 9 (top left panel); #14 represents a 64-year-old female with an FDP score of 10 (top right panel); #26 represents a 72-year-old male with an FDP score of 6 (bottom left panel); and #48 represents a 55-year-old male with an FDP score of 4 (bottom right panel).
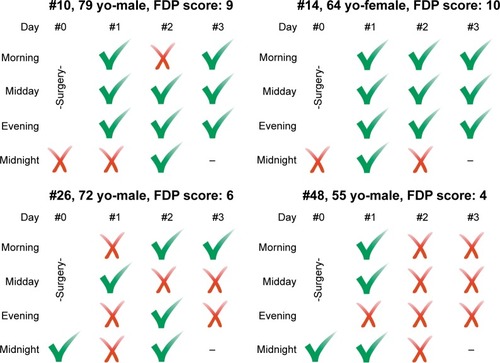
Patients #10 and #14 had intermediate scores, which are shown in the upper panels of . These patients usually maintained FDP during the day, but tended to lose a point at midnight. The patients who showed the poorest adherence (#26 and #48) did not maintain FDP even during the day (lower panels of ). Any disability or any problematic behavior was not mentioned in the nursing records. The patients understood the advice given by the nurse each time but were often found in the supine position during the next examination. Moreover, repeated instructions did not improve their adherence.
Prognosis after surgery
Primary anatomical MH closure was achieved in 68 eyes (98.6%). Only one patient (1.4%, #48) failed to achieve MH closure, and this patient had the lowest FDP score ( and ). Consequently, the closure rate in patients with an FDP score <8 (6/7, 85.7%) was lower than that in patients with an FDP score ≥8 (62/62, 100%); however, the difference was not statistically significant (P<0.11, Fisher’s exact probability test). A statistically significant difference was observed when a FDP score of 7 was used as the cutoff level; the closure rate in patients with FDP score <7 (2/3, 66.7%) was significantly lower than that in patients with an FDP score ≥7 (66/66, 100%) (<0.05, Fisher’s exact probability test).
Table 2 Closure rate
On preoperative assessment of patient #48, the MH was 390 µm in diameter and consistent with Gass stage 3. He underwent a second surgery 10 days after the first surgery. Complete fluid-gas exchange and gas tamponade with 20% sulfur hexafluoride were performed again without repeating the removal of internal limiting membrane. This patient’s FDP score after the second surgery was a perfect 12, and his MH closed completely.
Another patient, #26, who underwent a repeat surgery, was also one of the low scorers ( and ). His MH closed successfully; however, he developed a rhegmatog-enous retinal detachment in the same eye 6 months later. During the second vitrectomy procedure, the causative retinal break was closed and the retina was reattached. The FDP score after the second surgery was 9, whereas it was 6 after the first surgery. The relationship between poor adherence after the first surgery and the onset of retinal detachment was not determined.
Discussion
Mechanical sensory devices have been produced and tested in two pilot studies involving 10Citation4 and 13Citation21 patients, respectively, to assess the posture of the head after MH surgery. Although the device recorded the patient’s head position continuously for 24 h, it had to be mounted on the patient’s head, which could increase the strain on the patients. Although the FDP score measured by us is a rough index obtained only from the nursing records, it can still be retrospectively used for the evaluation of many patients and their surgical outcomes.Citation29 In this study, approximately 50% of the females and 40% of the males had a perfect FDP score of 12. However, the sampling frequency of four times per day was not sufficient to actually determine whether their adherence was perfect; nonetheless, we can assume that they showed good adherence.
Patients who did not have a perfect score were often not found in FDP at midnight, which may possibly be attributable to deep sleep. Further, this was also found to be the case in a study which used a head-mounted monitoring device.Citation4 The effort required to sleep in FDP may be different from that required to remain in FDP during the awake hours, and this may be a key determination of the degree of adherence for many patients.
Low scorers, who failed nearly or more than half the time, did not maintain FDP even during the day. It should be noted that the patients surveyed in this research were kept in the hospital under observation. If they had recovered at home after the surgery, their adherence would likely have been worse.
In an analysis of the FDP scores in 127 patients after vitrectomy for rhegmatogenous retinal detachments at the same facility over the same time period, 31.1% of females and 29.3% of males were perfect scorers,Citation29 which is lower than that observed in the present study. This may be because of the urgency of surgery for retinal detachments. In cases of retinal detachments, many patients underwent surgery on the first day of their hospital visit. However, patients with MH had a substantial amount of time to prepare for their surgery because their surgery was scheduled at least 1 month in advance. Consideration time for surgery and FDP could improve patient adherence. However, the percentage of patients with FDP scores <8 did not differ; the overall rate among patients with retinal detachment was 9.4% and that among males was 14.6%.Citation29 This indicates that even the long preparation period had little effect on the patients who showed the poorest adherence.
In this study, the lowest scorer was the only patient who failed to achieve the initial MH closure. Statistically, it suggests that poor adherence to FDP was responsible for the failed MH surgery. After a second surgery, this patient’s adherence drastically improved and the MH closure was successfully achieved.
In the treatment of MH, the optimal manner and the duration of the FDP to optimize patient recovery have been argued.Citation2–Citation28 Although each protocol assumes that the patients will follow the given advice, some patients (approximately 10%) do not comply. Although they may appear compliant, their poor prognosis can negatively impact the effectiveness of the surgery.
Conclusion
Adherence may be improved by various measures, for example, by supplying an inflatable assistant deviceCitation18 or fastening a tennis ball to the back of the patient’s nightshirt to keep the patient in a nonsupine position.Citation19 Poor adherence could be attributed to the inconvenience of FDP; therefore, alleviated positioning,Citation6–Citation13,Citation15,Citation19,Citation20,Citation22–Citation25,Citation27,Citation28 which may be easier to comply with, may improve patient adherence and postoperative outcomes.
Ethics approval and consent to participate
This study adhered to the tenets of the Helsinki Declaration and was approved by the Institutional Review Board of Fujita Health University (IRB no 16-036). For this type of study, hospital-based and retrospective, formal consent is not required. IRB of Fujita Health University waived the patient written informed consent for this study as patient data confidentiality was maintained at all times.
Author contributions
Shimada drafted the manuscript; Seno and Mizuguchi were responsible for data acquisition; Tanikawa and Horiguchi performed the surgery. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The dataset supporting the findings of this study is available upon request from Yoshiaki Shimada, MD (e-mail: [email protected]). A part of this study was presented at the 8th Asia Pacific Vitreo-retina Society Congress 2013.12.7, Nagoya, Japan, as a poster presentation.
Disclosure
The authors report no other conflicts of interests in this work.
References
- KellyNEWendelRTVitreous surgery for idiopathic macular holes results of a pilot StudyArch Ophthalmol19911096546592025167
- ThompsonJTSmiddyWEGlaserBMSjaardaRNFlynnHWJrIntraocular tamponade duration and success of macular hole surgeryRetina1996163733828912962
- TornambePEPolinerLSGroteKMacular hole surgery without face-down positioning. A pilot studyRetina1997171791859196926
- VermaDJalabiMWWattsWGNaylorGEvaluation of posturing in macular hole surgeryEye (Lond)20021670170412439662
- KrohnJDuration of face-down positioning after macular hole surgery: a comparison between 1 week and 3 daysActa Ophthalmol Scand20058328929215948778
- Dhawahir-ScalaFEMainoASahaKMokashiAAMcLauchlanRCharlesSTo posture or not to posture after macular hole surgeryRetina200828606518185139
- GuillaubeyAMalvitteLLafontainePOComparison of face-down and seated position after idiopathic macular hole surgery: a randomized clinical trialAm J Ophthalmol200814612813418440484
- TathamABanerjeeSFace-down posturing after macular hole surgery: a meta-analysisBr J Ophthalmol20109462663119767335
- TadayoniRVicautEDevinFA randomized controlled trial of alleviated positioning after small macular hole surgeryOphthalmology201111815015521035869
- ChandraACharterisDGYorstonDPosturing after macular hole surgery: a reviewOphthalmologica2011226Suppl 139
- SoleboALLangeCABunceCBainbridgeJWFace-down positioning or posturing after macular hole surgeryCochrane Database Syst Rev201112CD008228
- LangeCAMembreyLAhmadNPilot randomised controlled trial of face-down positioning following macular hole surgeryEye (Lond)20122627227721941361
- YagiFTakagiSTomitaGCombined idiopathic macular hole vitrectomy with phacoemulsification without face-down positioningJ Ophthalmol2012201257174822523650
- AlmeidaDRWongJBelliveauMRayatJGaleJAnatomical and visual outcomes of macular hole surgery with short-duration 3-day face-down positioningRetina20123250651022392092
- NadalJDelasBPiñeroAVitrectomy without face-down posturing for idiopathic macular holesRetina20123291892122080914
- MalikADooleyIMahmoodUSingle night postoperative prone posturing in idiopathic macular hole surgeryEur J Ophthalmol20122245646021928260
- XirouTTheodossiadisPGApostolopoulosMMacular hole surgery with short-acting gas and short-duration face-down positioningClin Ophthalmol201261107111222973086
- SchaeferHKossMJSinghPKochFSignificant improvement in compliance with the face-down position after vitrectomy and gas tamponadeKlin Monatsbl Augenheilkd201222992893622837068
- ForsaaVARaederSHashemiLTKrohnJShort-term postoperative non-supine positioning versus strict face-down positioning in macular hole surgeryActa Ophthalmol20139154755122830524
- IezziRKapoorKGNo face-down positioning and broad internal limiting membrane peeling in the surgical repair of idiopathic macular holesOphthalmology20131201998200323890419
- LeitritzMAZiemssenFVoykovBBartz-SchmidtKUUsability of a gravity- and tilt-compensated sensor with data logging function to measure posturing compliance in patients after macular hole surgery: a pilot studyGraefes Arch Clin Exp Ophthalmol201425273974424292701
- HeffezJLMacular hole repair without face-down positioningInt Ophthalmol Clin201454115
- FeistRMJrPomerleauDLFeistRNonsupine positioning is preferred by patients over face-down positioning and provides an equivalent closure rate in 25- and 23-gauge macular hole surgeryRetin Cases Brief Rep2014820520825372439
- AlbertiMla CourMFace-down positioning versus non-supine positioning in macular hole surgeryBr J Ophthalmol20159923623925147367
- PasuSBunceCHooperRThomsonABainbridgeJPIMS (Positioning In Macular hole Surgery) trial – a multicentre interventional comparative randomised controlled clinical trial comparing face-down positioning, with an inactive face-forward position on the outcome of surgery for large macular holes: study protocol for a randomised controlled trialTrials20151652726576755
- EssexRWKingstonZSMoreno-BetancurMThe effect of postoperative face-down positioning and of long- versus short-acting gas in macular hole surgery: results of a registry-based studyOphthalmology20161231129113626920098
- HuZXiePDingYZhengXYuanDLiuQFace-down or no face-down posturing following macular hole surgery: a meta-analysisActa Ophthalmol20169432633326385613
- AlbertiMla CourMNonsupine positioning in macular hole surgery: A Noninferiority Randomized Clinical TrialRetina2016362072207927046458
- SenoYShimadaYMizuguchiTTanikawaAHoriguchiMCompliance with the face-down positioning after vitrectomy and gas tamponade for rhegmatogenous retinal detachmentsRetina2015351436144025748281
