Abstract
Background
The purpose of this study is to illustrate the fundus autofluorescence and high-definition optical coherence tomography (HD-OCT) features of acute and long-standing retinal artery occlusions.
Design
Retrospective case series.
Participants
Patients with acute and chronic retinal and cilioretinal artery occlusions are included in this series.
Methods
A detailed clinical examination, color fundus photographs, autofluorescence, and HD-OCT of the subjects were performed.
Results
HD-OCT demonstrates the localized and well-demarcated thickening of the inner retina in the acute phase of arterial occlusions that correlates with the areas of blocked autofluorescence caused by the cloudy swelling of the retina. The areas of blocked autofluorescence disappear with chronicity of the disease and this corresponds to the thinning of the inner retinal layers on HD-OCT.
Conclusion
Heidelberg OCT and autofluorescence are useful tools to assess retinal arterial occlusions especially in subjects with unexplained visual field loss.
Background
Retinal artery occlusions usually present with irreversible field loss corresponding to the area of retinal ischemia. The initial pallor of the retina is replaced by the normal sheen of the fundus and it is not always easy to diagnose the condition in long-standing cases.
The high-definition spectral domain optical coherence tomography scans (HD-OCT), an advancement over the previous time domain OCTs, show near perfect delineation of the retinal layers, akin to an in-vivo histological section of the retina. Together with fundus autofluorescence imaging that indicates the health of the outer retina and retinal pigment epithelium (RPE), we are now able to better understand retinal disease processes. This case series highlights how these non-invasive imaging techniques provide valuable information on the diagnosis of retinal arterial diseases.
Design
This is a case series of patients who attended the Laser and Retinal Research Unit of King’s College Hospital, London, with history of acute visual disturbance or unexplained visual field loss, who were subsequently diagnosed to have acute or long-standing occlusions of cilioretinal artery, central and branch retinal arteries.
Material and methods
All the subjects in this case series underwent detailed clinical examination including visual acuity assessment, slit-lamp examination, fundus biomicroscopy, and indirect ophthalmoscopy. The color fundus photographs were recorded with Topcon fundus camera. The red-free, infrared, autofluorescence imaging, and HD-OCT were performed using the Spectralis HRA+OCT (Heidelberg Engineering, Heidelberg, Germany) system.
Case 1
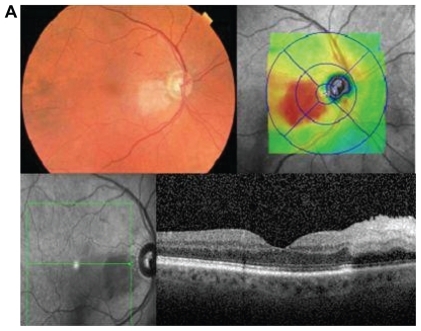
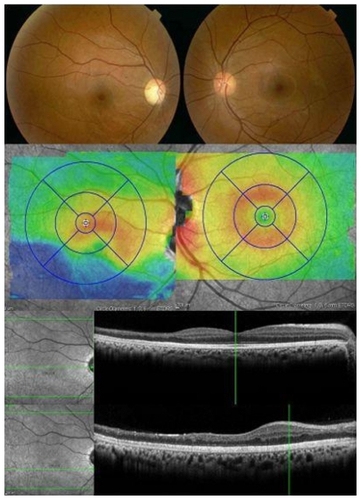
A 76-year-old male presented with a central visual blur in the right eye of 3 days duration. He had undergone retinal detachment surgery in the left eye. His visual acuity was 6/9 in the right eye and 6/12 in the left eye. Clinical examination showed an acute fovea sparing cilioretinal artery occlusion in the right eye. The HD-OCT revealed marked thickening of the inner retina supplied by the cilioretinal supply with an abrupt transition to the normal thickness where the retina is presumably supplied by the central retinal artery (). The autofluorescence of the corresponding area showed blocked fluorescence with normal fluorescence over the rest of the retina. Fundus fluorescein angiography revealed delayed filling of the cilioretinal artery while the branches of the central retinal artery showed normal perfusion ().
Case 2
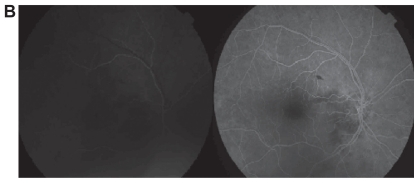
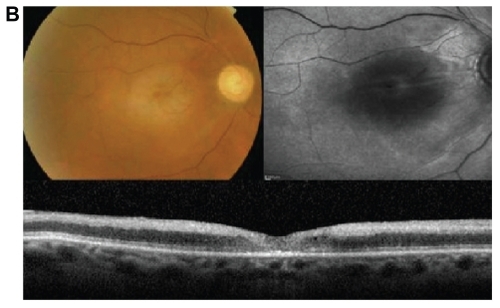
A 69-year-old lady presented with history of sudden loss of vision in the right eye of 18 hours duration. She is a known hypertensive and is on dialysis for chronic renal failure. She could perceive hand movements in the right eye and 6/18 in the left eye. She had features of acute central retinal artery occlusion (CRAO) with sparing of the cilioretinal artery that supplied a small area of the retina in the upper temporal area adjacent to the disc, not involving the fovea. Fundus autofluorescence of the right eye showed blocked fluorescence in the posterior pole except in the area of the cilioretinal artery, which showed normal fluorescence. This blocked effect corresponded to the marked thickening of the inner retina in the area supplied by the occluded central retinal artery (CRA). The thickening terminated abruptly at the junction of the CRA with the cilioretinal artery, revealing normal retinal layers in the area uninvolved by the occlusion ().
Figure 2a Color fundus photographs of the right eye (Case 2) showing central retinal artery occlusion with cilioretinal sparing and normal left eye. The decreased autofluorescence of the right eye correspond to marked inner retinal thickening on HD-OCT, with normal autofluorescence in the cilioretinal area. The thickening of the retina is obvious in the retinal thickness color map as well.
The patient was followed up monthly for two subsequent visits, when the affected eye showed resolution of the cloudy thickening of the retina as shown in . The autofluorescence of the affected eye also improved, as the retinal thickening settled.
Case 3
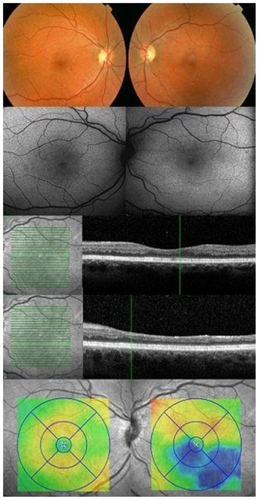
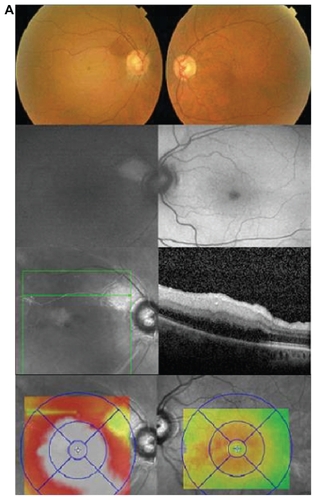
A 33-year-old lady presented a superior field defect in the left eye, noticed three months ago. On examination vision was 6/6 in both eyes. Fundus was unremarkable with mild temporal pallor of the optic disc in the left eye. Fundus autofluorescence was normal in both eyes. However, HD-OCT showed marked retinal thinning in the inferior temporal retina, with normal retinal thickness at the fovea, confirming the diagnosis of an inferior temporal branch artery occlusion. The outer retinal layers appeared well preserved with normal thickness. The retinal thickness color map clearly revealed the area corresponding to the occluded inferior temporal artery (). On retrospect, she gave a history of recurrent abortions and she was subsequently investigated for antiphospholipid antibody syndrome.
Case 4
A 22-year-old woman with antiphospholipid syndrome developed a visual field defect following a pre-term delivery a year ago. On examination, visual acuity was 6/6 in both eyes. Fundus autofluorescence was normal in both eyes but retinal thickness color map showed marked retinal thinning in the inferior part in the right eye () providing the clue to the diagnosis of a long-standing inferotemporal branch retinal artery occlusion. The HD-OCT showed normal retinal architecture at the foveal area with thinning of the inner retina temporal and inferior to the fovea with preservation of the outer retinal layers.
Discussion
This case series demonstrates the autofluorescence and OCT findings in cases of acute and long-standing retinal artery occlusions. Previous studies have reported sectorial thinning of the retina in branch artery occlusions using time-domain OCT.Citation1–Citation4 Puliafito et al described increased reflectivity of the inner retinal layers, that he attributed to the morphological changes secondary to ischemia.Citation4 The reduced reflectivity of the external retinal layers was postulated to be due to the accumulation of fluid in the area. But Hayreh et al has demonstrated by histological studies that two hours after a CRAO, irreversible damages occur to the inner retinal layers including the nerve fibre layer, ganglion cell layer, and inner two third of the inner nuclear layer. However, the outer nuclear and plexiform layers and photoreceptors remained intact.Citation5,Citation6 Our study helps understand this difference in observations regarding changes in the outer retinal layers made by the two investigators.
Although the time domain OCT (TD-OCT) is an invaluable tool in the diagnosis, management and follow up of various ocular conditions, its axial resolution of 10 μm is inferior to the HD OCT which has a scan rate at least 20,000 axial scans per second and an improved axial resolution of 2–5 μm. Thus, the latter enables precise delineation of almost all of the retinal layers, which was not always possible with TD-OCT. The preferential thickening of the inner retinal layers in acute arterial occlusions and the thinning of these layers in long standing occlusions with preservation of the outer retinal layers is better identified with HD-OCT. Additionally, the TD-OCT uses six radial B-scans centered around the fovea and mathematical interpolations are used to derive thickness estimates for the area in between. On the other hand, HD-OCT evaluation is evenly distributed over the sampled area allowing precise localization of the area of supply of the occluded vessel.
The classic description of acute occlusions of the retinal artery is a cloudy swelling of the inner retinal layers, and this explains the thickening of the inner retinal layers up to the inner plexiform layer, with abrupt transition at the junction with the perfused retina in the first two cases.
The outer retinal layers from the outer plexiform layer below the thickened inner retina are not clearly discernable in the HD-OCT and is seen as a hypo-reflective or widened area, in contrast to the adjacent layers below the normally perfused retina. This is due to the ‘back shadowing’ or masking of the outer layers by the cloudy swelling of the inner retina.
Autofluorescence of the area supplied by the occluded retinal artery in the acute stages also show decreased autofluorescence due to the blockage of the normal autofluorescence of the RPE by the thickened inner retina. The resolution of the cloudy swelling over time leads to recovery of the normal autofluorescence of the retina. In very thin inner retina, an increased autofluorescence may also be visualized due to a ‘window defect’.
A recently published report on sequential retinal changes after embolic occlusion of the inferior branch artery using spectral domain OCT,Citation7 describes the inner retinal thickening that developed in the acute phase of disease and resolution of the same after distal propagation of the embolus, indicating that the cloudy swelling is reversible.
Fundus fluorescein angiography (FFA) in arterial occlusions show delayed filling of the involved artery in the acute stage (as shown in ) with delay in the retinal arteriovenous transit time. Complete lack of filling of the retinal arteries in the acute stage is very rare (less than 2%).Citation8 The retinal circulation then re-establishes at varying intervals of time following the occlusion and may even be normal in long-standing occlusions, but the visual field defect is usually permanent. Thus FFA is only useful in the diagnosis of the acute stage of artery occlusions if it is clinically challenging to diagnose.
In most cases, although the pale retina is replaced by the normal sheen of the fundus, damage of the inner retina results in irreversible field defects. The diagnosis of subtle, long-standing branch arterial occlusions with preserved normal central vision may sometimes be challenging. However, the characteristic thinning of the inner retinal layers with well demarcated junction between the nonperfused and perfused retina (Cases 3 and 4) on OCT is a useful sign to aid diagnosis. In fact, the OCT thickness color map easily identifies the thinning of the retina that is supplied by the occluded retinal artery.
Current treatment options for acute artery occlusions are not effective in reversing the damage caused by the occlusion. A number of options have been tried within the first 24 hours of the occlusion such as ocular massage, anterior chamber paracentesis, breathing a mixture of oxygen and carbon dioxide, and the use of fibrinolytic agents. However, the latest findings on OCT and autofluorescence explains why the outcomes are equivocal.
It is important that the patients are investigated thoroughly for an underlying cause of the occlusion. Echocardiography, carotid doppler studies, coagulation profile, erythrocyte sedimentation rate, and C-reactive protein are imperative to pre-empt further systemic and ocular vascular events.
Conclusion
We conclude that HD-OCT serves as a valuable, noninvasive tool in the diagnosis of acute and long-standing retinal artery occlusions.
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- AsefzadehBNinyoKLongitudinal analysis of retinal changes after branch retinal artery occlusion using optical coherence tomographyOptometry2008792859018215797
- TakahashiHHiroyukiISectoral thinning of the retina after branch retinal artery occlusion (Japan)Jpn J Ophthalmol20095349450019847605
- Salinas-AlamánAGarcía-LayanaAHeras-MuleroHGarcía-GómezPJOptical coherence tomography in central retinal artery occlusionArch Soc Esp Oftalmol20068155355617016789
- PuliafitoCAHeeMRSchumanJSFujimotoJGOptical coherence tomography of ocular diseases1ª editionThorofareSlack Inc1996
- HayrehSSKolderHEWeingeistTACentral retinal artery occlusion and retinal tolerance timeOphthalmology19808775786769079
- HayrehSSZimmermanBMKimuraACentral retinal artery occlusionRetinal Survival Time Exp Eye Res2004783723736
- MurthyRKGroverSChalamKVSequential spectral domain OCT documentation of retinal changes after branch retinal artery occlusionClin Ophthalmol2010432732920463801
- BrownGCMagargalLECentral retinal artery obstruction and visual acuityOphthalmology19828914197070767