Abstract
We present a case of retinitis pigmentosa with vitreoretinal traction-associated retinal detachment. The retinal detachment was detected in the nasal periphery. No retinal breaks and no active vascular leakage were observed by fundus scopy and fluorescein angiography, respectively. However, 8 months later, the tractional retinal detachment was spontaneously resolved with posterior vitreous detachment.
Introduction
Retinitis pigmentosa (RP) was defined as a group of hereditary disorders that diffusely involve photoreceptor and pigment epithelial function characterized by progressive visual field loss and abnormal electroretinogram. RP also has changes at vitreoretinal interface, such as vitreoretinal traction and preretinal membrane, which causes macular disorders such as cystoids macular edema and macular hole. We report a case of vitreoretinal traction syndrome associated with RP, which spontaneously resolved after posterior vitreous detachment (PVD).
Case report
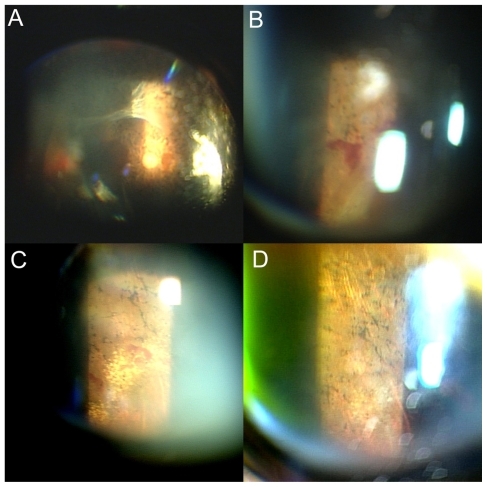
A 81-year-old woman presented with bilateral loss of peripheral vision and defective dark adaptation 15 years before. The best-corrected visual acuity was 20/28 and 20/28 in the right and left eyes, respectively. Slit-lamp examination showed bilateral retinal arteriolar narrowing and intraretinal pigment deposition (bone spicule pigmentation) in both eyes (). The visual fields of the patient were markedly constricted to the central 10° in both eyes (). On June 2, 2006, retinal detachment was detected in the nasal periphery in the right eye (). At that time, PVD was confirmed with Weiss ring (). Fluorescein angiography showed a hyperfluorescence due to atrophy of retinal pigment epithelium but no active leakage in the detached area (). Fundus examination revealed no retinal breaks. Therefore, we diagnosed tractional retinal detachment associated with vitreoretinal traction. The detached area was within the area where the visual field was lost, and we observed a clinical course of this eye without any treatment. Retinal detachment was kept localized and not extended. Five months later, PVD further progressed beyond the arcade area, accompanying retinal hemorrhage around the detached retina. Thereafter, the tractional retinal detachment and retinal hemorrhage were gradually resolved. Eight months later, the retina was completely reattached.
Figure 1 Photographs of a 81-year-old woman with retinitis pigmentosa. A) Fundus photographs show bilateral retinal arteriolar narrowing and intraretinal pigment deposition (bone spicule pigmentation) in both eyes, left: left eye, right: right eye. B) A fundus photograph of the right eye using a slit-lamp examination shows a detached retina in the nasal periphery. C) Fluorescein angiography images of the right eye show a hyperfluorescence due to atrophy of retinal pigment epithelium and hypofluorescence in the detached area.
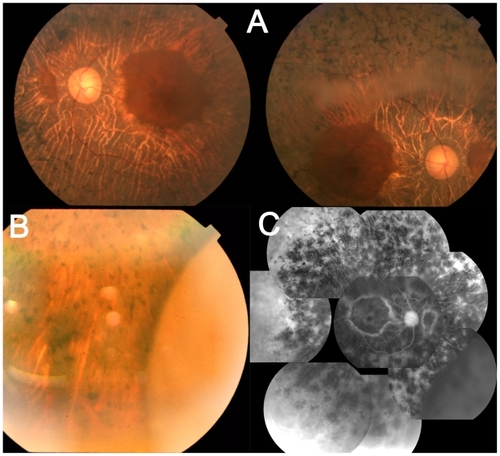
Figure 2 Visual fields of left eye (left) and right eye (right) of a patient with retinitis pigmentosa using a Goldmann perimeter were markedly constricted to the central 10° diameter.
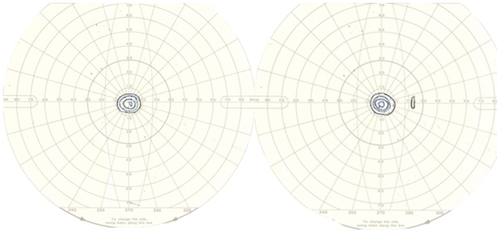
Figure 3 The right eye of the same patient. A) and B) A fundus photograph using a slit-lamp examination of 5 months later shows that the posterior vitreous detachment further progressed beyond the arcade area A), accompanying retinal hemorrhage around the detached retina B). C) A fundus photograph using a slit-lamp examination of 8 months later shows that the retina is reattached, and hard exudates are observed in the nasal periphery. D) A fundus photograph using a slit-lamp examination of 12 months later shows that those hard exudates are resolved.
Discussion
In this case, an eye with RP was complicated with tractional retinal detachment, possibly associated with increased vitreoretinal traction secondary to the incidence of PVD. The retinal detachment was limited within the area where the visual field was lost and was not progressive. Therefore, we observed a clinical course of the patient without any surgical treatment. Eight months later, spontaneous resolution of tractional retinal detachment resulted from progression of PVD, which was suggested by transiently increased traction-related retinal hemorrhage. Eyes with RP may have abnormal liquefaction of vitreous and altered distribution of vitreoretinal adhesion. The incidence of PVD in the posterior pole might result in the focal remarkable traction in the peripheral retina and tractional retinal detachment. Eight months later, the retinal detachment was resolved because local vitreoretinal traction was weakened with extention of PVD beyond the arcade vessels.
RP has vitreomacular traction-related pathologic events involving vitreomacular traction syndrome, cystoids macular edema, and macular hole.Citation1–Citation3 Such changes in this patient with RP might result in a tractional retinal detachment. Rani et alCitation4 reported that a 50-year-old man underwent a tractional retinal detachment involving the posterior pole with a taut posterior hyaloids surface. In this study, vitrectomy was not performed because the patient opted for no surgical intervention in view of poor prognosis. On the other hand, it was reported that vitrectomy was effective for vitreous opacity,Citation5 cystoid macular edema,Citation6 exudative retinal detachment,Citation7 and macular holesCitation8 in RP. However, regarding the indication to perform a vitrectomy, the balance of the expected gain in visual function and usual risks of vitrectomy and RP-related risks, such as phototoxicity worsening of visual field loss, and cystoid macular edema. It might be a choice that a patient with tractional retinal detachment in RP is observed without surgical treatment, if the detached area is not progressive.
Disclosure
The authors report no conflicts of interest in this work.
References
- FishmanGAFishmanMMaggianoJMacular lesions associated with retinitis pigmentosaArch Ophthalmol197795798803860943
- WiseGNClinical features of idiopathic preretinal macular fibrosis. Schoenberg LectureAm J Ophthalmol1975793493571121990
- DemirMNUnlNYalnizZAcarMAOrnekFA case of retinal detachment in retinitis pigmentosaEur J Ophthalmol20071767767917671951
- RaniAPalNAzadRVSharmaYRChandraPVikram SinghDTractional retinal detachment in usher syndrome type IIClin Experiment Ophthalmol20053343643716033369
- HongPHHanDPBurkeJMWirostkoWJVitrectomy for large vitreous opacity in retinitis pigmentosaAm J Ophthalmol200113113313411162992
- Garcia-ArumiJMartinezVSararolsLCorcosteguiBVitreoretinal surgery for cystoids macular edema associated with retinitis pigmentosaOphthalmology20031101164116912799242
- LeeSYYoonYHPars plana vitrectomy for exudative retinal detachment in coats-type retinitis pigmentosaRetina20042445045215187669
- JinZBGanDKXuGZNaoINMacular hole formation in patients with retinitis pigmentosa and prognosis of pars plana vitrectomyRetina20082861061418398364