Abstract
Purpose
To evaluate the morphological changes in retinal microstructures following modified photodynamic therapy (PDT) for chronic central serous chorioretinopathy.
Subjects and methods
Retrospective study of 21 consecutive eyes (age, 59±8.0 years [mean ± SD]) of 21 patients with chronic central serous chorioretinopathy. Inner foveal thickness (the distance between the internal limiting membrane and external limiting membrane), photoreceptor outer segment (PROS) length at the point without serous retinal detachment and choroidal thickness were assessed with enhanced depth imaging optical coherence tomography before treatment and at 1, 3 and 6 months after modified PDT.
Results
Six eyes had half-dose and 15 eyes had half-fluence PDT. PROS length within the irradiated area was significantly decreased by 3.9% at 1 month compared with that before modified PDT (43.5±5.72 and 40.5±7.53, P=0.020 [paired t-test]) and returned to baseline length at 3 and 6 months (43.0±5.42 and 43.5±4.33 μm [mean ± SD]; P=0.53 and 1.00 [paired t-test]). PROS length of the nonirradiated area at 1, 3 and 6 months after modified PDT did not significantly differ from that before PDT (41.8±6.35, 41.4±5.33, 41.9±4.67 and 42.3±4.26 μm [mean ± SD]; P=0.66, 0.90 and 0.60, respectively [paired t-test]). There was no significant change in inner foveal thickness during the observation period. At all time points, choroidal thickness was significantly thinner than it was before PDT (P<0.001, paired t-test).
Conclusion
Modified PDT may cause mild temporary microstructural changes.
Introduction
Chronic central serous chorioretinopathy (CSC) is characterized by long-term serous retinal detachment (SRD) in the central macular regionCitation1,Citation2 due to primary disturbance of choroidal circulation.Citation1–Citation3 Persistent or recurrent SRD leads to progressive visual loss.Citation4,Citation5 The pathogenesis of CSC is not well understood, but some reports have described systemic involvement.Citation6,Citation7
Since the first report showing the efficacy of photodynamic therapy (PDT) with verteporfin (Visudyne; Novartis AG, Basel, Switzerland) for the treatment of chronic CSC,Citation8 several subsequent reports have confirmed its effectiveness, which is through promotion of subretinal fluid (SRF) absorption by reducing choroidal vascular hyper-permeability. Although rare, complications such as retinal pigment epithelium (RPE) changes, excessive choriocapillaris hypoperfusion and secondary choroidal neovascularization (CNV) have been reported.Citation8–Citation12 To reduce adverse effects, modified PDT protocols, such as half-fluence/half-dose PDT, have been proposed and are now frequently used in the treatment of chronic CSC.Citation13,Citation14 While several studies have reported its effectiveness and safety, the influence on photoreceptors has been also reported.Citation15,Citation16 However, no studies have demonstrated quantitative change of photoreceptors after modified PDT.
Spectral-domain optical coherence tomography (SD-OCT, Spectralis®; Heidelberg Engineering, Heidelberg, Germany) has enabled the investigation of morphological changes to the microstructures of photoreceptors in the retina. Some studies have shown a significant association between the best-corrected visual acuity (BCVA) and the integrity of the ellipsoid zone (EZ, also known as the photoreceptor inner and outer segment junction line) and interdigitation zone (also known as the cone outer segment tips) in CSC.Citation17–Citation19 Recently, it was also reported that central photoreceptor outer segment (PROS) length, which refers to the distance between the EZ and the RPE (defined as the most hyperreflective line by ImageJ [National Institutes of Health, Bethesda, MD; available at http://rsbweb.nih.gov]), is strongly correlated with BCVA after idiopathic epiretinal membrane (ERM) surgery and in patients with diabetic macular edema.Citation20,Citation21 Thus, PROS length is also considered an important parameter for deducing retinal function.
PDT causes choriocapillaris damage and choroidal vascular remodeling. A number of studies have investigated choroidal structure after PDT, demonstrating decreased choroidal thickness (CT) even after modified PDT.Citation22–Citation25 However, only a few qualitative studies, but no quantitative reports, have thoroughly investigated the microstructural changes in the outer retina after modified PDT. Thus, the current study examined PROS length and inner foveal thickness (IFT) to determine the influence on photoreceptors after modified PDT for chronic CSC.
Subjects and methods
Patient selection
Thirty-seven chronic CSC patients underwent their first PDT between May 2012 and July 2014 at Tokyo University Hospital. Among them, 21 were enrolled in the current analysis after excluding the following patients: 1) those who had received previous PDT (n=1); 2) those with evidence of CNV or polypoidal choroidal vasculopathy (PCV) (n=1); 3) those who received PDT irradiation covering the extrafoveal region only (n=3) and 4) those who had smaller area of PDT irradiation than the lesion of SRD (n=11), because we measured PROS length at the point where PDT was irradiated but without SRD, in order to avoid the influence of SRD on photoreceptors. All patients had symptomatic chronic CSC for ≥3 months, and were followed up for at least 6 months after initial PDT. Diagnosis was based on the findings of slit-lamp biomicroscopy, fluorescein angiography (FA), indocyanine green angiography (ICGA) and SD-OCT. BCVA data and SD-OCT images were available from all patients before PDT and at 1, 3 and 6 months after PDT.
Study protocol
This retrospective study was approved by the Institutional Review Board of the University of Tokyo. All patients provided written consent to review their medical records. BCVA and SD-OCT findings were investigated before and at 1, 3 and 6 months after PDT. BCVA findings were converted to a logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Macular scanning with SD-OCT was performed using both standard and enhanced depth imaging modes, with a width of 6 mm. In SD-OCT images, we assessed the IFT (the distance between the internal limiting membrane [ILM] and the external limiting membrane [ELM]), PROS length (the distance between the EZ and the RPE) and CT. RPE layer was defined using ImageJ software in the following text.
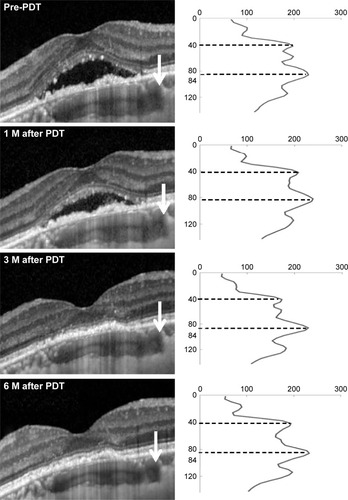
IFT and PROS length measurements were performed using ImageJ software V1.48, according to the method of Shiono et al.Citation21 Reflectivity of cross-sectional parallel lines was calculated longitudinally within the selected area in gray-scale SD-OCT images. SD-OCT scans through the fovea showed 4 clearly distinguishable, highly reflective bands as previously described, representing the RPE, EZ, ELM and ILM. PROS length was measured as the distance between the RPE and the EZ, and IFT as that between the RPE and the ILM. IFT was measured at the fovea, and the PROS length was measured at 2 sections: one within the irradiated area and the other outside. To exclude the influence of SRD, measurements were performed in the area without SRD. In patients that had “follow-up” mode SD-OCT scans, we could choose the same points. In other cases, we selected the same points from the fundus images accompanied with SD-OCT scans at each time point (). Examples of the serial changes of PROS length calculated from SD-OCT findings are displayed in .
Figure 1 Thick arrow in the fundus image refers to the same place where thin arrow points to the spectral domain optical coherence tomography scan.
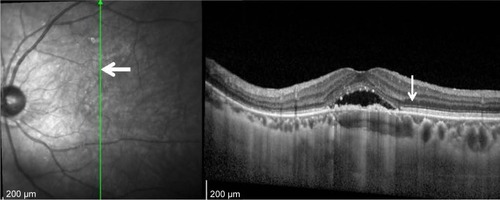
Figure 2 A representative case with chronic CSC.
Abbreviations: CSC, central serous chorioretinopathy; EZ, ellipsoid zone; M, months; PDT, photodynamic therapy; RPE, retinal pigment epithelium.
CT was assessed at 3 sections: fovea and 2 points where the PROS length was measured. CT was measured manually with a caliper embedded in the SD-OCT system.
Photodynamic therapy
Patients received either half-fluence or half-dose PDT with verteporfin. Half-fluence PDT was performed with a 6 mg/m2 dose of verteporfin but with half-fluence of 300 mW/cm2 for 83 seconds. Half-dose PDT was employed using a 50% dose of verteporfin (3 mg/m2) with the duration and laser power unchanged, and a fluence of 600 mW/cm2 for 83 seconds. Greatest linear dimension (GLD) was determined with reference to the area of abnormal choroidal circulation, such as hyperpermeability and dilated choroidal vessels, and the area showing RPE breakdown according to the findings of FA and ICGA. We adopted ICGA study in 14 eyes and FA study in 7 eyes, and determined GLD strictly to avoid possible collateral damage. Laser spot size was set aŝ500 μm plus the GLD, with a maximum size of 50 μm. Verteporfin was infused over 10 minutes, followed by delivery of diode laser at 689 nm (Visulas 690S; Carl Zeiss Meditec Inc., Dub-lin, CA, USA) 15 minutes after the start of infusion. After treatment, all patients were given protective spectacles and instructed to avoid strong light for at least 48 hours.
Statistical analysis
Serial comparisons of mean BCVA, IFT, PROS length and CT were conducted using the paired t-test. JMP software (version 11; SAS institute Inc., Cary, NC, USA) was used for data analysis, and a P-value of <0.05 was considered statistically significant. Bonferroni correction was not performed because this was a hypothesis-generating study, the purpose of which was to identify a possible association between variables. Intraclass correlation coefficients were calculated by ICC function in psych R package.
Results
A total of 21 eyes of 21 patients with chronic CSC were studied (male eyes 14, mean age 59±8.0 years). Two patients were with drusen and 1 patient with ERM. There was no patient with high myopia or other retinal diseases. Fifteen patients received half-fluence PDT and 6 received half-dose PDT. The mean spot size was 2,977 μm with a range from 1,400 to 4,500 μm.
SRD was resolved completely after 1 month in 12 eyes and after 3 months in 5 eyes, with 17 (81%) of the eyes showing complete reabsorption. The remaining 4 eyes had persistent SRD throughout the follow-up period: 2 showed a decrease, but the other 2 were unchanged. No patients developed systemic side effects related to PDT, and neither RPE atrophy nor development of CNV was observed. The mean logMAR BCVA was 0.18 (0.66), 0.19 (0.64), 0.13 (0.74) and 0.12 (0.76) before PDT and at 1, 3 and 6 months after PDT, respectively. Compared with baseline, a significant BCVA improvement was seen at 3 and 6 months after treatment (P=0.0045, 0.0020, respectively, paired t-test).
Retinal sublayer thickness was measured by 2 independent ophthalmologists, and the repeatability of the measurement was high, as evaluated by intraclass and interclass repeatability (). At 1, 3 and 6 months after PDT, the mean IFT was not significantly different from that before PDT (, P=0.30, 0.22 and 0.22, respectively, paired t-test; ). However, the mean PROS length of the irradiated area at 1 month after PDT was thinner than that before (, P=0.020, paired t-test); although at 3 and 6 months, there was no significant difference compared with that before PDT (, P=0.53, 1.00, paired t-test; ). The same result was derived in half-fluence PDT group, and there was a similar trend in half-dose PDT group (). The mean PROS length of the nonirradiated area at 1, 3 and 6 months after PDT was not significantly different from that before PDT (, P=0.66, 0.90, and 0.60, respectively, paired t-test; ). The mean CT measured at 3 sections at 1, 3 and 6 months after PDT is listed in . At all time points, the mean CT of all 3 sections was significantly thinner than that before PDT (P<0.001, paired t-test).
Figure 3 Serial changes in mean central IFT after half-fluence PDT in chronic central serous chorioretinopathy.
Abbreviations: IFT, inner foveal thickness; M, months; PDT, photodynamic therapy.
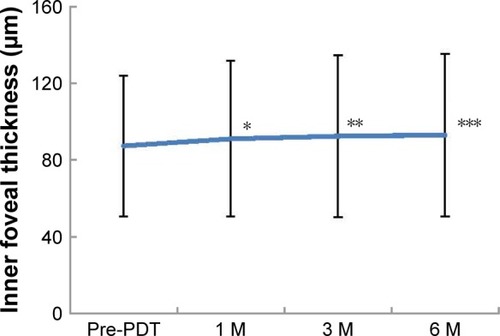
Figure 4 Serial changes in mean PROS length of the irradiated area after half-fluence PDT in chronic central serous chorioretinopathy.
Abbreviations: M, months; PDT, photodynamic therapy; PROS, photoreceptor outer segment.
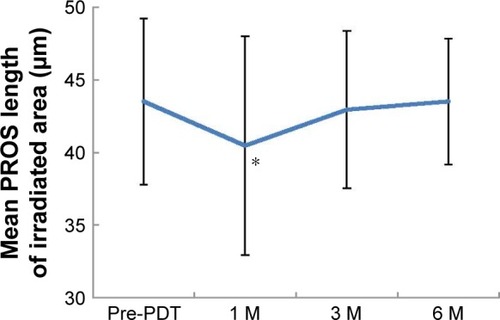
Figure 5 Serial changes in mean PROS length of nonirradiated area after half-fluence PDT in chronic central serous chorioretinopathy.
Abbreviations: M, months; PDT, photodynamic therapy; PROS, photoreceptor outer segment.
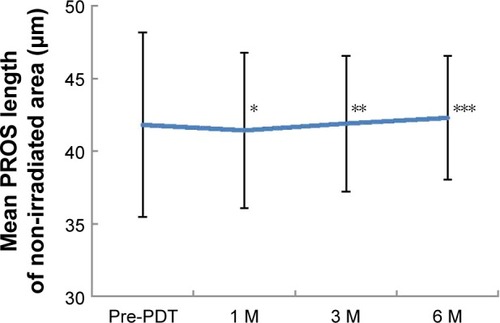
Table 1 Repeatability for inner foveal thickness, PROS length and choroidal thickness in CSC obtained using SD-OCT (n=21)
Table 2 Changes in inner foveal thickness after PDT (n=21)
Table 3 Changes in PROS length after PDT (n=21)
Table 4 Changes in PROS length after PDT in irradiated area in half-fluence and half-dose groups
Table 5 Changes in choroidal thickness after PDT (n=21)
Discussion
This retrospective study suggests that PDT induces temporary micro-morphological changes in photoreceptors. The PROS length of the irradiated area was significantly thinner at 1 month after PDT than that before PDT, but it recovered to the baseline level at 3 and 6 months after PDT. In half-dose PDT, PROS length tended to become shorter at 1 month, although not significant due to small sample size (6 eyes). In contrast, the PROS length of the nonirradiated area did not differ from that before PDT at each time point examined. This temporal change in photoreceptors could have been a direct or secondary effect of modified PDT.
In this study, we were able to detect significant shortening of PROS length at 1 month after PDT. There is conflicting evidence about the influence of PDT on photoreceptors. Schlötzer-Schrehardt et al reported that the overlying RPE and sensory retina were preserved in histopathological analysis 1 week after PDT, suggesting no subacute retinal or RPE damage after PDT.Citation22 However, no histological study has yet investigated changes to photoreceptors 1 month after PDT. We hypothesize that this change occurs later than 1 week after PDT or that the histological changes are minute since the change in length, although significant, was only 3.1 μm. Indeed, the current method may be able to detect minute changes compared with histological analysis. For example, Yuksel et al also reported the significant changes in PROS length after ERM surgery, although the changes were just 2.9 μm at a minimum.Citation26
There are 3 possible explanations for the temporal shortening of PROS after PDT: hypoperfusion of choriocapillaris, a temporal increase of exudation after PDT and a direct effect by PDT. First, it may have been a secondary effect of collateral choroidal damage. The effect of PDT on choriocapillaris has been reported in both pathological and ICGA examinations. Schlötzer-Schrehardt et al detected choriocapillaris occlusion in the region of PDT application 1 week after standard PDT in human eyes by histopathological analysis.Citation22 They also demonstrated the existence of repair mechanisms through observations of surviving endothelial cells, which indicated choriocapillaris recanalization as soon as 1 week after treatment. In the untreated area, choriocapillary structure was normal with open lumina. Schmidt-Erfurth et al later reported choroidal hypofluorescence in the treated area, the severity of which was most intense 1 week after PDT, with subsequent recovery of choroidal perfusion in ICGA findings.Citation23 By means of ICGA, Reibaldi et al revealed that choriocapillaris at the site of PDT application was affected even by low-fluence PDT, although the intensity was less than that with standard PDT.Citation14 Taken together, these findings suggest that in general, there is temporal choriocapillaris occlusion after PDT. Since the nutrients from choroidal circulation are essential for photoreceptor maintenance, it is rational to consider such choriocapillaris hypoperfusion that might have affected photoreceptors. The second explanation is that these changes were related to a temporal increase in exudation after PDT. Previous studies uniformly agree that there is a temporal exacerbation of exudative change after PDT, which resolved as early as 1 week after PDT.Citation27–Citation29 It is also possible that this temporal exudation might have caused damage to the photoreceptors and contributed to the temporal reduction of PROS length. The final explanation is that PDT had a direct effect on photoreceptor cells through unknown mechanism(s).
We detected a temporal change in photoreceptors, but the influence on visual function has not been determined. Some reports suggest a high correlation between PROS length and BCVA. Shiono et al demonstrated a significant correlation between postoperative PROS length and BCVA in patients with a removed ERM, particularly at the central region.Citation21 Forooghian et al also reported a strong correlation between foveal PROS length and BCVA in patients with diabetic macular edema.Citation20 These findings support the fact that the central PROS length is a quantitative and important parameter of visual function. However, we did not assess the correlation between PROS length and BCVA. One reason for this was the relatively small number of investigated eyes, but more importantly, the measurements were taken outside the fovea to avoid the area of SRD. Therefore, it deemed unsuitable to assess the relationship between retinal function and the temporal changes in PROS length after PDT.
Several studies have assessed retinal function after PDT by evaluating retinal sensitivity using microperimetry. Fujita et al evaluated retinal sensitivity in central 4°, 8° and 12° circles in chronic CSC, revealing significant improvements at 1, 3 and 6 months after half-dose PDT at all sites.Citation30 Senturk et al also examined retinal sensitivity in central 10°, 20°, and paracentral 10° to 20° sites, revealing significant improvements at 1, 3 and 6 months after half-dose PDT in eyes with chronic CSC.Citation31 Multifocal electroretinogram (mfERG) has also been utilized to evaluate retinal function after PDT. In contrast to the microperimetric studies, Lai et al detected a transient reduction in response amplitudes and a delay in peak latencies of mfERG for as long as 2 weeks, and recovery 1 month after PDT in patients with CNV.Citation11 Overall, electrophysiological and current SD-OCT studies indicate temporal retinal damage after PDT, while microperimetric results show improved retinal function. It is not surprising that the retinal function improves after the absorption of SRF as has been reported by previous studies. These apparently discordant functional findings from previous studies may be due to the difference in the baseline visual function, the irradiation area, the size of SRF and chronicity of the disease. The current cases were with relatively good visual acuity and no signs of chronicity such as atrophic tract (or gravitational tract).
With regard to CT, our results concur with those of previous investigations. We also evaluated choroidal changes after PDT for chronic CSC using SD-OCT at 3 sections: 2 within the irradiated area and 1 in the nonirradiated area. A reduction in CT was observed in all areas. Sugano et al also reported a reduction in CT after PDT for PCV outside the irradiated area.Citation32 Our results are compatible with previous reports of the effect of PDT on the choroid even in the area not exposed to PDT laser treatment.
Finally, our findings also showed that the mean IFT at 1, 3 and 6 months after PDT did not differ significantly from that before PDT; however, there was a tendency toward increased IFT at 1 month after PDT. The most probable cause of this can be due to improved metabolism of photoreceptors in the fovea after reattachment to RPE, or a decrease in physical pressure on the photoreceptors as a result of resolution of SRF.
Analytic software of SD-OCT has been improving and Spectralis is equipped with new software that can finely segment each retinal layer and measure each layer’s thickness automatically. In normal eyes, this measuring method may be quite accurate, but if there are lesions such as SRF, and/or pigment epithelial detachment, automated segmentation sometimes fails to recognize ELM, EZ, RPE and Bruch membrane correctly, thus requiring manual correction. Although ImageJ uses manual measurement, it is most useful in the analysis of the outer retinal thickness.Citation33,Citation34 We still assume this to be one of the most accurate measurements at the moment.
Despite the significant findings, our study is limited by its retrospective design. The number of investigated eyes was relatively small, and the follow-up period was relatively short. Further prospective studies with large numbers are therefore needed to confirm our results. Other limitations were the lack of evaluation at the early phase within 1–2 weeks after PDT and insufficient evaluation of retinal function. Analysis of sequence changes in the retina after PDT are therefore required both morphologically and functionally, allowing us to determine the mechanism of temporal impairment of the retina induced by PDT. Our study showed that a total of 17 of 21 eyes (81%) had complete reabsorption at 6 months. In contrast, Fujita et al studied totally 204 eyes with chronic CSC and reported 182 eyes (89%) with resolution of SRD at 12 months after the half-dose PDT.Citation35 Our treatment outcome seems slightly poor, but direct comparison is meaningless because of the differences of the follow-up period and studied subjects.
In conclusion, our findings showed mild outer retinal microstructural changes 1 month after modified PDT, with recovery at 3 and 6 months. The changes were short-lived and of uncertain clinical significance; however, it should be noted that we assessed patients with a single PDT application. There is a possibility that irreversible impairment to the retina may occur as a result of multiple PDT applications, especially when full-dose PDT is employed. Further observations and clinical trials are therefore needed to assess the effect of PDT on photoreceptor and retinal function.
Disclosure
The authors report no conflicts of interest in this work.
References
- PrunteCFlammerJChoroidal capillary and venous congestion in central serous chorioretinopathyAm J Ophthalmol1996121126348554078
- PiccolinoFCBorgiaLCentral serous chorioretinopathy and indocyanine green angiographyRetina19941432312427973118
- GuyerDRYannuzziLASlakterJSSorensonJAHoAOrlockDDigital indocyanine green videoangiography of central serous chorioretinopathyArchs Ophthalmol1994112810571062
- LevineRBruckerAJRobinsonFLong-term follow-up of idiopathic central serous chorioretinopathy by fluorescein angiographyOphthalmology198491154415486521993
- LooRHScottIUFlynnHWJrFactors associated with reduced visual acuity during long-term follow-up of patients with idiopathic central serous chorioretinopathyRetina2002221192411884873
- ErolMKBalkarliAToslakDEvaluation of nailfold videocapillaroscopy in central serous chorioretinopathyGraefe’s Arch Clin Exp Ophthalmol2016254101889189626995556
- KloosPLaubeIThoelenAObstructive sleep apnea in patients with central serous chorioretinopathyGraefe’s Arch Clin Exp Ophthalmol200824691225122818546012
- ChanWMLamDSLaiTYTamBSLiuDTChanCKChoroidal vascular remodeling in central serous chorioretinopathy after indo-cyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease levelBr J Ophthalmol200387121453145814660450
- FickerLVafidisGWhileALeaverPLong-term follow-up of a prospective trial of argon laser photocoagulation in the treatment of central serous retinopathyBr J Ophthalmol198872118298343061449
- Cardillo PiccolinoFEandiCMVentreLRigault de la LongraisRCGrignoloFMPhotodynamic therapy for chronic central serous chorioretinopathyRetina200323675276314707823
- LaiTYChanWMLamDSTransient reduction in retinal function revealed by multifocal electroretinogram after photodynamic therapyAm J Ophthalmol2004137582683315126146
- TzekovRLinTZhangKMOcular changes after photodynamic therapyInvest Ophthalmol Vis Sci200647137738516384988
- ChanWMLaiTYLaiRYTangEWLiuDTLamDSSafety enhanced photodynamic therapy for chronic central serous chorioretinopathy: one-year results of a prospective studyRetina2008281859318185143
- ReibaldiMCardasciaNLongoAStandard-fluence versus low-fluence photodynamic therapy in chronic central serous chorioretinopathy: a nonrandomized clinical trialAm J Ophthalmol2010149230731519896635
- HernandezGCarlosJCamarilloMSaddaSRLong-term follow-up of photoreceptor loss and recovery after half-fluence photodynamic therapy for chronic central serous chorioretinopathyRetin Cases Brief Rep20159210911325383847
- RatanasukonMThongthongKBhurayanontachaiPJirarattanasopaPPhotoreceptor disruption in central serous chorioretinopathy treated by half-dose photodynamic therapyClinl Ophthalmol201378792
- MatsumotoHKishiSOtaniTSatoTElongation of photoreceptor outer segment in central serous chorioretinopathyAm J Ophthalmol2008145116216818028861
- ParkSJWooSJParkKHHwangJMChungHMorphologic photoreceptor abnormality in occult macular dystrophy on spectral-domain optical coherence tomographyInvest Ophthalmol Vis Sci20105173673367920164460
- ItohYInoueMRiiTHiraokaTHirakataASignificant correlation between visual acuity and recovery of foveal cone microstructures after macular hole surgeryAm J Ophthalmol20121531111.e1119.e121880295
- ForooghianFStetsonPFMeyerSARelationship between photoreceptor outer segment length and visual acuity in diabetic macular edemaRetina2010301637019952996
- ShionoAKogoJKloseGPhotoreceptor outer segment length: a prognostic factor for idiopathic epiretinal membrane surgeryOphthalmology2013120478879423290984
- Schlotzer-SchrehardtUViestenzANaumannGOLaquaHMichelsSSchmidt-ErfurthUDose-related structural effects of photodynamic therapy on choroidal and retinal structures of human eyesGraefe’s Arch Clin Exp Ophthalmol2002240974875712271373
- Schmidt-ErfurthUMichelsSBarbazettoILaquaHPhotodynamic effects on choroidal neovascularization and physiological choroidInvest Ophthalmol Vis Sci200243383084111867605
- MarukoIIidaTSuganoYOjimaAOgasawaraMSpaideRFSubfoveal choroidal thickness after treatment of central serous chori-oretinopathyOphthalmology201011791792179920472289
- KangNHKimYTChange in subfoveal choroidal thickness in central serous chorioretinopathy following spontaneous resolution and low-fluence photodynamic therapyEye201327338739123288136
- YukselKKarakucukYOzkayaAComparison of photoreceptor outer segment length in diabetic and idiopathic epiretinal membranesEye201529111446145226183287
- RogersAHMartidisAGreenbergPBPuliafitoCAOptical coherence tomography findings following photodynamic therapy of choroidal neovascularizationAm J Ophthalmol2002134456657612383814
- CostaRAFarahMECardilloJACalucciDWilliamsGAImmediate indocyanine green angiography and optical coherence tomography evaluation after photodynamic therapy for subfoveal choroidal neovascularizationRetina2003232159165
- MichelsSSchmidt-ErfurthUSequence of early vascular events after photodynamic therapyInvest Ophthalmol Vis Sci20034452147215412714655
- FujitaKShinodaKMatsumotoCSMicroperimetric evaluation of chronic central serous chorioretinopathy after half-dose photodynamic therapyClin Ophthalmol201261681168723097612
- SenturkFKaracorluMOzdemirHKaracorluSAUysalOMicroperimetric changes after photodynamic therapy for central serous chorioretinopathyAm J Ophthalmol20111512303.e1309.e121168824
- SuganoYIidaTMarukoIOjimaASekiryuTChoroidal thickness outside the laser irradiation area after photodynamic therapy in polypoidal choroidal vasculopathyJpn J Ophthalmol201357329430023408087
- ChenHXiaHQiuZChenWChenXCorrelation of optical intensity on optical coherence tomography and visual outcome in central retinal artery occlusionRetina201636101964197026966866
- IchiyamaYKawamuraHFujikawaMSawadaOSaishinYOhjiMPhotoreceptor outer segment length and outer foveal thickness as factors associated with visual outcome after vitrectomy for vitreomacular traction syndromeRetina20163691707171226866525
- FujitaKImamuraYShinodaKOne-year outcomes with half-dose verteporfin photodynamic therapy for chronic central serous chorioretinopathyOphthalmology2015122355556125444637
