Abstract
Objective
To identify residents’ perceived barriers to learning phacoemulsification surgical procedures and to evaluate whether virtual reality simulation training changed these perceptions.
Design
The ophthalmology residents undertook a simulation phacoemulsification course and proficiency assessment on the Eyesi system using the previously validated training modules of intracapsular navigation, anti-tremor, capsulorrhexis, and cracking/chopping. A cross-sectional, multicenter survey on the perceived difficulties in performing phacoemulsification tasks on patients, based on the validated International Council of Ophthalmology’s Ophthalmology Surgical Competency Assessment Rubric (ICO-OSCAR), using a 5-point Likert scale (1 = least and 5 = most difficulty), was conducted among residents with or without prior simulation training. Mann–Whitney U tests were carried out to compare the mean scores, and multivariate regression analyses were performed to evaluate the association of lower scores with the following potential predictors: 1) higher level trainee, 2) can complete phacoemulsification most of the time (>90%) without supervisor’s intervention, and 3) prior simulation training.
Setting
The study was conducted in ophthalmology residency training programs in five regional hospitals in Hong Kong.
Results
Of the 22 residents, 19 responded (86.3%), of which 13 (68.4%) had completed simulation training. Nucleus cracking/chopping was ranked highest in difficulty by all respondents followed by capsulorrhexis completion and nucleus rotation/manipulation. Respondents with prior simulation training had significantly lower difficulty scores on these three tasks (nucleus cracking/chopping 3.85 vs 4.75, P = 0.03; capsulorrhexis completion 3.31 vs 4.40, P = 0.02; and nucleus rotation/manipulation 3.00 vs 4.75, P = 0.01). In multivariate analyses, simulation training was significantly associated with lower difficulty scores on these three tasks.
Conclusion
Residents who had completed Eyesi simulation training had higher confidence in performing the most difficult tasks perceived during phacoemulsification.
Introduction
The global number of blindness due to cataract has increased from 12.3 million in 1990 to 20 million in 2010.Citation1,Citation2 In East Asia, including Hong Kong, cataract is the leading cause of blindness and visual impairment in the pooled data of population-based studies.Citation3,Citation4 Various initiatives have been undertaken in response to fight the cataract epidemic in Hong Kong, including implementation of key performance indicator based on the waiting time for cataract surgery in public hospitals and subsidization for cataract surgery in public–private partnership programs. As a result, the average waiting time for cataract surgery in public hospitals has markedly reduced approximately threefold, from over 44 months before 2008 to 15 months after 2013.Citation5 As physicians have pledged to keep shortening the waiting time, the demand for cataract surgeries will continue to be relentless.
Alongside the rising demand for cataract surgeries, there is a constant influx of ophthalmic residents. Learning to competently perform phacoemulsification is one of their top training priorities. Traditionally, residents learned phacoemulsification based on the Halsted apprenticeship model,Citation6 in which they perform the techniques step by step on actual patients under the close supervision of an attending physician. A wide range of intraoperative complication rates from 2.0% to 14.7% in resident-performed phacoemulsification surgeries have been reported; while some phacoemulsification surgeries performed by residents have comparable outcomes,Citation7–Citation9 others have increased complication rates and worse patient outcomes.Citation10–Citation16 The highly variable complication rates could be due to the lack of systematic consideration of potential perioperative risk factors, such as history of traumatic cataracts, hypermature cataracts, and zonular loosening.Citation10 Nonetheless, the cost of training during live surgeries may be higher due to prolonged operation time.Citation17,Citation18 With rising patient expectations and demands of high-quality surgical outcomes, it is vital that ophthalmic residents learn to operate in a manner that is safe and time efficient.
A pilot virtual reality simulation cataract surgery training course was conducted in Hong Kong using the validated training modules on the Eyesi (VRmagic, Holding AG, Mannheim, Germany) computer-generated three-dimensional cataract operation environment for ophthalmic residents. A cross-sectional survey was conducted after the course for participants and nonparticipants of the course. The objectives of this study were to identify the residents’ perceived barriers to learning phacoemulsification procedures and whether simulation training on Eyesi changed these perceptions.
Methods
Simulation training curriculum
A structured, certified phacoemulsification simulation training course was held for ophthalmic residents who participated on a voluntary basis at The Chinese University of Hong Kong Ophthalmic Microsurgical Training Centre, the only virtual reality eye surgery simulation training facility in Hong Kong. The course included didactic lectures and hands-on practicum on the Eyesi simulator. Before simulation training began, all participants were given a 2-hour formal introduction and standardized instructions on how to use the Eyesi phacoemulsification interface software version 2.8 by the training coordinator. Four training modules with specific difficulty levels were chosen because their construct validities had been demonstrated previously.Citation19–Citation24 The modules consisted of a mix of generic three-dimensional and cataract-specific, static and dynamic tasks in order to capture a full range of dexterity and skill as measured and trained by the simulator. Three of them were single-handed tasks (cataract navigation training [intracapsular], level 3; cataract anti-tremor training [intracapsular], level 2; capsulorrhexis training, level 1), and one was a bimanual task (cataract cracking and chopping training, level 2). The participants were given as much practice time as possible before sitting in for a test at the end of the 4-week course. For each of the four tasks, participants could achieve a maximum score of 100, resulting in a total maximum course score of 400. A proficiency test was performed under supervision, which required 80% passing mark. A certificate was awarded upon successful completion of the course.
Survey
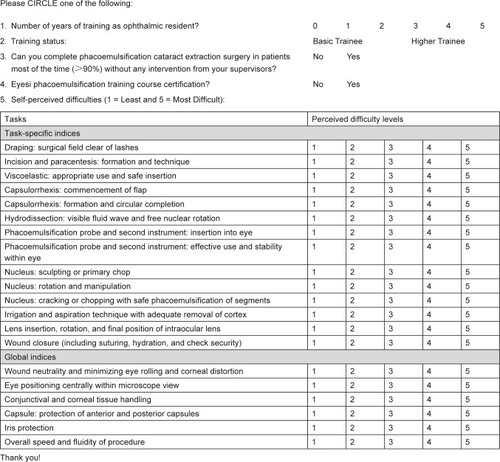
A cross-sectional, anonymous, self-administered territory-wide survey of ophthalmic residents’ self-perceived learning barriers to phacoemulsification techniques, based on modifications of the validated International Council of Ophthalmology’s Ophthalmology Surgical Competency Assessment Rubric (ICO-OSCAR) – Phacoemulsification tool,Citation25 was conducted among ophthalmic residents in Hong Kong regardless of their participation in the simulation training course or not (). The study adhered to the tenets of the Declaration of Helsinki. Informed consent was signed by all subjects. The study was approved by the Hong Kong hospital authority cluster institutional review board. The residents were affiliated with five regional hospitals throughout the three major districts in Hong Kong: Tung Wah Eastern Hospital and Pamela Youde Nethersole Eastern Hospital in Hong Kong Island, Hong Kong Eye Hospital in Kowloon, Alice Ho Miu Ling Nethersole Hospital, and Prince of Wales Hospital in the New Territories. The coverage was about 50% of all ophthalmic resident doctors throughout the Hong Kong Special Administrative Region. After reading the specific guidelines for grading of each surgical step listed on the ICO-OSCAR, the respondents ranked the levels of perceived difficulty on a 5-point scale (1 = least and 5 = most difficult) for each of the 14 phacoemulsification procedures and six global indices on the survey. In addition, they provided demographic information, and answered questions on their training status (basic or higher ophthalmic trainees, as determined by whether they had passed the intermediate examination to obtain the Membership of the Royal College of Surgeons of Edinburgh [MRCSEd]), whether they were able to complete phacoemulsification cataract extraction surgery in patients most of the time (>90%) without any intervention from their supervisor (Yes or No), and whether they received the certification for the Eyesi phacoemulsification training course (Yes or No).
Statistical analysis
Mann–Whitney U tests were carried out to compare the means of continuous variables between the subgroups with or without training on Eyesi. Univariate and multivariate regression analyses were performed for potential predictors (higher trainee, can complete phacoemulsification most of the time [90%] without supervisor’s intervention, and certification in the Eyesi training course) and their associations with the tasks in which Eyesi simulation-trained residents had significantly lower difficulty scores. A P-value of <0.05 was considered to be statistically significant. All of the statistical analyses were performed with SPSS software version 18.0 (SPSS Inc, Chicago, IL, USA).
Results
There were 22 residents in all five of the regional hospitals, and all were invited to participate in the survey. Nineteen completed the survey, and the response rate was 86.3%. The mean ± SD age of ophthalmic residents who participated in the survey was 28.7 ± 1.8 years (range 25–35 years), of which 11 (57.9%) were female. Thirteen (68.4%) had participated and were certified in the Eyesi simulation training course. The mean number of years of training was 3.5 ± 1.8 (range 1–5 years), and 12 (63.2%) were basic trainees (first year: six trainees; second year: six trainees) and seven (36.8%) were higher trainees (third year: four trainees; fourth year: two trainees; fifth year: one trainee). Five out of the 19 trainees could complete phacoemulsification in >90% of cases without intervention from attending physicians. All five of them were higher trainees.
The mean self-perceived difficulty scores on phacoemulsification procedures of the overall group, the group that did not have Eyesi training, and the group that had Eyesi training are shown in . Nucleus cracking or chopping was ranked the highest in difficulty by the overall group (mean score 4.06 ± 0.83). This was followed by capsulorrhexis formation and completion (mean score 3.61 ± 0.92), nucleus rotation and manipulation (mean score 3.41 ± 1.28), hydrodissection (mean score 3.22 ± 1.26), nucleus sculpting or primary chop (mean score 3.12 ± 1.36), and effective use and stability of phacoemulsification probe and secondary instruments within the eye (mean score 3.12 ± 1.36). For the global indices, overall speed and fluidity of the procedure ranked the highest in difficulty (mean score 3.26 ± 1.24). Except for hydrodissection and effective use and stability of phacoemulsification probe and secondary instruments within the eye, trainees without prior Eyesi simulation training had significantly higher mean difficulty scores in all the top ranking procedures and global indices. A histogram () illustrates the eight tasks (specific and global) that residents without Eyesi training had significantly higher mean difficulty scores than those who had Eyesi training. These tasks were ordered from left to right on the histogram according to the highest difficulty ranking perceived by the overall group to the least difficult.
Figure 2 Histogram of mean difficulty scores of the eight tasks that trainees without Eyesi training had significantly higher scores than trainees who had the Eyesi training. These tasks were ordered from left to right on the histogram according to the highest difficulty ranking perceived by the overall group to the least difficult.
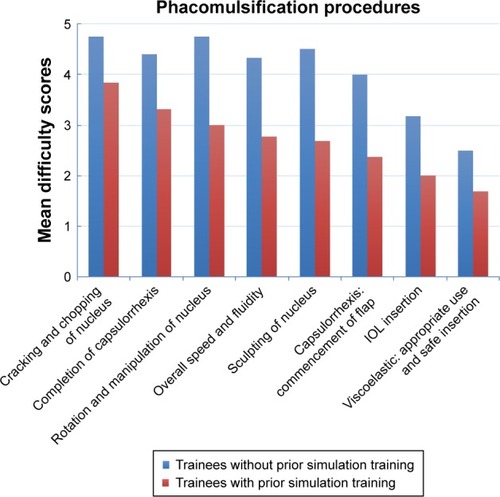
Table 1 Mean difficulty scores on 14 specific tasks and six global indices for phacoemulsification based on the International Council of Ophthalmology’s Ophthalmology Surgical Competency Assessment Rubric perceived by all respondents (N = 19), the subgroup which had no Eyesi simulation training (N = 6), and the subgroup which had Eyesi simulation training (N = 13)
Regression analyses were performed to evaluate the associations of the eight tasks that the residents with Eyesi simulation training had significantly lower mean difficulty scores ( and ) with potential predictors. In univariate analyses, higher trainees were significantly associated with lower difficulty scores in overall speed and fluidity of procedure, commencement of capsulorrhexis flap, intraocular lens (IOL) insertion, and appropriate use and safe insertion of viscoelastic. Residents who could complete phacoemulsification most of the time (>90%) without supervisor’s intervention were significantly associated with lower difficulty score in commencement of capsulorrhexis flap. In multivariate analyses, residents who were certified in the Eyesi simulation course were significantly associated with lower difficulty scores in cracking and chopping of lens nucleus, completion of capsulorrhexis, rotation and manipulation of lens nucleus, and sculpting or primary chopping of nucleus.
Table 2 Regression analyses of four tasks (cracking and chopping of lens nucleus, completion of capsulorrhexis, rotation and manipulation of lens nucleus, and overall speed and fluidity) that trainees who had Eyesi simulation training had significantly lower difficulty scores than trainees who did not have Eyesi simulation training
Table 3 Regression analyses of four tasks (sculpting or primary chopping of nucleus, commencement of capsulorrhexis flap, IOL insertion, and appropriate use and safe insertion of viscoelastic) that trainees who had Eyesi simulation training had significantly lower difficulty scores than trainees who did not have Eyesi simulation training
Discussion
In this study, we have identified the top learning barriers to phacoemulsification cataract extraction surgery perceived by ophthalmic residents in Hong Kong. We expected that higher trainees, and trainees who were able to complete phacoemulsification most of the time without needing attending physician intervention, would also have the lowest difficulty scores in the surgical tasks.Citation26 However, after adjusting for these two potential confounding factors, Eyesi simulation training was significantly associated with increased confidence in higher difficulty surgical tasks. Virtual reality simulation training on the validated Eyesi modules followed by proficiency assessment appeared to be effective in lowering the perceived difficulties in performing the most skills-demanding phacoemulsification procedures on actual patients as rated by the residents.
Our survey was designed according to the ICO-OSCAR tool.Citation25 The rubric draft was developed by content experts from around the world based on the Dreyfus model of skill acquisition and revised by expert panels in teaching cataract surgery.Citation27 Hence, the respondents were able to gain thorough understandings on how their surgical proficiencies on actual patients would be assessed objectively based on the ICO-OSCAR before ranking the difficulty levels on the survey. Previous surveys on self-perceived training difficulties in phacoemulsification cataract extraction surgery did not use a standardized format to describe the specific surgical tasks.Citation28,Citation29 In 2006, Dooley and O’Brien reported the surgical procedures that were perceived to be most difficult by eight trainees during phacoemulsification cataract extraction surgery were 1) phacoemulsification, 2) capsulorrhexis, 3) irrigation/aspiration (I/A), 4) IOL insertion, and 5) hydrodissection.Citation28 Prakash et al reported in 2009 that 36 trainees ranked 1) foldable IOL insertion as the most difficult task, followed by 2) nucleus emulsification, 3) I/A, 4) capsulorrhexis, and 5) hydrodelineation.Citation29 Our questionnaire, based on the ICO-OSCAR guideline, had dissected the specific steps required to accomplish phacoemulsification of the nucleus, and we have identified that cracking and chopping, rotation and manipulation, and sculpting of the nucleus were among the most difficult tasks perceived by residents. Our survey provided important and updated information on the perceived learning barriers by ophthalmic residents in phacoemulsification, which could have changed from the previous decade because of the availability of improved fluidics and followability of advanced phacoemulsification systems, and newer inserters for rolled IOL through small corneal incisions.Citation30
Nevertheless, the development of user-friendly phacoemulsification systems has not changed the skills demanded from the surgeon when performing capsulorrhexis, other than the availability of femtosecond laser assistance which has not yet been implemented in public hospitals in Hong Kong. Capsulorrhexis had been regarded as one of the most challenging procedures during phacoemulsification cataract extraction surgery in this study as well as in a number of previous studies.Citation26,Citation28,Citation29,Citation31 When capsulorrhexis is attempted, there is a natural tendency for the flap to extend radially which increases the subsequent risk of posterior capsule tear resulting in vitreous loss and lens nucleus drop. Thus, it is considered crucial for residents to master the skills in performing capsulorrhexis to minimize the rates of cataract surgery complications. Because capsulorrhexis and lens nucleus cracking and chopping are among the initial steps of phacoemulsification cataract extraction surgery which have a steep learning curve, some attending physicians would prefer to teach phacoemulsification starting from reverse order: the trainee surgeon performs I/A and IOL insertion after the supervisor completes capsulorrhexis and phacoemulsification of the lens.Citation28,Citation32,Citation33 This reverse teaching approach could deprive the chances of novice surgeons to practice performing the tasks that have the steepest learning curves, but this approach is better for patient care and safety.
The paradox of traditional apprenticeship-based surgical training is that today’s patients can be harmed in the training of tomorrow’s surgeons. Moreover, the patient can be an unforgiving teacher. The trainees are exposed to real-time pressures during surgery on actual patients, especially when the majority of cataract extraction surgeries are performed under local anesthesia. The rate of posterior capsule tear among trainee surgeons has been shown to vary from 4.8% to 15%.Citation10–Citation16 Experienced surgeons tend to have much lower complication rates, with a vitreous loss rate of 0.53%–1.63%.Citation34–Citation36 Simulation surgical training allows the trainees to experience the consequences of their decisions and actions as they learn new skills without putting patients at risk. The construct validity of a number of training modules on the Eyesi simulator has been reported.Citation19–Citation23,Citation37 Saleh et al evaluated the repeatability and reproducibility of the capsulorrhexis, nucleus cracking and chopping, navigation, bimanual training, and anti-tremor modules in 18 residents.Citation37 Mahr and Hodge showed construct validity of anterior segment anti-tremor and forceps training modules in 15 participants comprising residents and experienced surgeons, and the experienced surgeons showed statistically significant better scores and faster time to complete the designated tasks.Citation19
Our simulation course was implemented based on a training program that had been established by the International Forum of Ophthalmic Simulation (IFOS) using the Eyesi simulator.Citation24 Saleh et al compared the entry and exit proficiency scores of 16 novice eye surgeons in performing the four validated modules (navigation, anti-tremor, capsulorrhexis, and nucleus cracking and chopping training) and showed a significant improvement for all these tasks in addition to the overall scores.Citation24 Our survey found that the proficiency-based Eyesi simulation course had boosted the confidence of ophthalmic residents in performing the most difficult tasks in phacoemulsification, regardless of their training status and prior experience in cataract surgery on actual patients. Our simulation course did not have an impact on the residents’ confidence in performing hydrodissection and effective use and stability of phacoemulsification probe and secondary instruments within the eye, which highlights the necessity of utilizing and assessing the effect of the hydrodissection/hydrodelineation and instruments insertion/removal training modules on Eyesi in the future.
The encouraging results of our survey lay the foundation for future research to evaluate the efficacy of virtual reality simulation phacoemulsification training on patient-related outcomes. Three retrospective studies had reported improved outcomes in the operating theatre associated with Eyesi simulation training.Citation38–Citation40 Belyea et al reported a significant decrease in phacoemulsification time and power use (2.4 vs 1.9 minutes, P < 0.002; 28.2% vs 25.3%, P < 0.0001, respectively) following training on Eyesi.Citation39 Baxter et al found that the complication rates of cataract surgeries performed by resident trainees who had Eyesi training were lower than those previously reported in the literature.Citation40,Citation41 McCannel et al found a significant decrease in the number of errant continuous curvilinear capsulorrhexes during cataract surgery after a capsulorrhexis-intensive training curriculum on the Eyesi simulator (15.7% vs 5.0% in the postintervention cohort; P < 0.0001).Citation38 Two prospective studies have been performed.Citation41,Citation42 Pokroy et al found significant decrease in operation time but nonsignificant difference in complication rates before and after training with Eyesi.Citation41 Recently, Thomsen et al reported that Objective Structured Assessment of Cataract Surgical Skill (OSACSS) scores when performing phacoemulsification on actual patients significantly improved by 32% in novice surgeons and 38% in intermediate-level surgeons who performed >75 surgeries even after adjusted for the effect of learning curve in a prospective, cohort study.Citation42
Our study was limited by lack of evaluation of patient-related outcomes associated with Eyesi simulation training and small sample size. We did not use other simulation modalities, such as porcine eyes, MicroVisTouch (ImmersiveTouch, Chicago, IL, USA), and PhacoVision (Melerit Medical, Linkoping, Sweden), for comparison with the Eyesi platform. Hence, we cannot ascertain whether any one of these simulation tools were just as effective as Eyesi in surgical training of novice surgeons at the initial stages of their learning curves. We reported subjective rankings perceived by the trainees without self-evaluations on surgical videos or objective rankings by experienced attending physicians. Using the OSACSS, Casswell et al studied the agreement between trainees and their evaluators in grading their own performances in surgical tasks during phacoemulsification on actual patients and found that senior trainees were more able to assess their performance than junior trainees, supporting the notion that trainees progress from being relatively unconsciously incompetent to becoming consciously competent during their surgical training.Citation43
Conclusion
Our study identified the updated perceptions on training barriers from ophthalmic residents. The responses of our survey reflected that ophthalmic residents were satisfied with the outcome of a structured Eyesi training course using validated training modules followed by a proficiency test. Our study has demonstrated level 1 evidence of the Kirkpatrick model in the evaluation of educational intervention.Citation44 The efficacy of virtual reality simulation cataract surgery training has only been proven to a certain extent.Citation45 Current evidence and assessment of simulator-based training is characterized by a scattered focus and lack of rigorous methodologies to ensure effective skills transfer to the operation theatre.Citation45 The ultimate goal of simulator use is to improve patient safety and outcomes by trainees. Given the wide adoption of simulator-based training by universities and tertiary ophthalmic centers in many parts of the world, there is an imminent need for a robust clinical trial to justify the efficacy of implementing virtual reality simulator training modules in structured phacoemulsification surgery training programs.
Disclosure
The authors report no conflicts of interest in this work.
References
- BourneRRStevensGAWhiteRACauses of vision loss worldwide, 1990–2010: a systematic analysisLancet Glob Health201316e339e34925104599
- PascoliniDMariottiSPGlobal estimates of visual impairment: 2010Br J Ophthalmol201296561461822133988
- MichonJJLauJChanWSEllweinLBPrevalence of visual impairment, blindness, and cataract surgery in the Hong Kong elderlyBr J Ophthalmol200286213313911815334
- WongTYZhengYJonasJBPrevalence and causes of vision loss in East Asia: 1990–2010Br J Ophthalmol201498559960424390167
- Waiting time for cataract surgery [webpage on the Internet]Hong KongHospital Authority2018 [updated December 31, 2016] Available from: https://www.ha.org.hk/visitor/ha_visitor_text_index.asp?Parent_ID=214172&Content_ID=214184Accessed January 14, 2017
- GrilloHCEdwardDChurchill and the “rectangular” surgical residencySurgery2004136594795215523385
- RandlemanJBWolfeJDWoodwardMLynnMJCherwekDHSrivastavaSKThe resident surgeon phacoemulsification learning curveArch Ophthalmol200712591215121917846361
- RandlemanJBSrivastavaSKAaronMMPhacoemulsification with topical anesthesia performed by resident surgeonsJ Cataract Refract Surg200430114915414967283
- BadozaDAJureTZuninoLAArgentoCJState-of-the-art phacoemulsification performed by residents in Buenos Aires, ArgentinaJ Cataract Refract Surg199925121651165510609212
- RutarTPorcoTCNaseriARisk factors for intraoperative complications in resident-performed phacoemulsification surgeryOphthalmology2009116343143619167084
- HashemiHMohammadpourMJabbarvandMNezamdoostZGhadimiHIncidence of and risk factors for vitreous loss in resident-performed phacoemulsification surgeryJ Cataract Refract Surg20133991377138223870438
- LeeJSHouCHYangMLKuoJZLinKKA different approach to assess resident phacoemulsification learning curve: analysis of both completion and complication ratesEye200923368368718239676
- TayanithiPPungpapongKSiramputPVitreous loss during phacoemulsification learning curve performed by third-year residentsJ Med Assoc Thai200588Suppl 9S89S93
- SinghAStewartJMPhacoemulsification performed by residentsJ Cataract Refract Surg2007335755 author reply 755–75617466830
- LomiNSharmaRKhokharSDadaTVanathiMAgarwalTRisk factors for intra-operative complications during phacoemulsification performed by residentsInt Ophthalmol201636340140626494477
- FeldmanBHGeistCEAssessing residents in phacoemulsificationOphthalmology20071148158617678697
- TaravellaMJDavidsonRErlangerMGuitonGGregoryDTime and cost of teaching cataract surgeryJ Cataract Refract Surg201440221221624461498
- HoslerMRScottIUKunselmanARWolfordKROltraEZMurrayWBImpact of resident participation in cataract surgery on operative time and costOphthalmology20121191959821924500
- MahrMAHodgeDOConstruct validity of anterior segment anti-tremor and forceps surgical simulator training modules: attending versus resident surgeon performanceJ Cataract Refract Surg200834698098518499005
- PrivettBGreenleeERogersGOettingTAConstruct validity of a surgical simulator as a valid model for capsulorhexis trainingJ Cataract Refract Surg201036111835183821029889
- LeTDAdatiaFALamWCVirtual reality ophthalmic surgical simulation as a feasible training and assessment tool: results of a multicentre studyCan J Ophthalmol2011461566021283159
- NathooNNgMRamsteadCLJohnsonMCComparing performance of junior and senior ophthalmology residents on an intraocular surgical simulatorCan J Ophthalmol20114618788
- SelvanderMAsmanPVirtual reality cataract surgery training: learning curves and concurrent validityActa Ophthalmol201290541241721054818
- SalehGMLamparterJSullivanPMThe International Forum of Ophthalmic Simulation: developing a virtual reality training curriculum for ophthalmologyBr J Ophthalmol201397678979223532612
- SalehGMGaubaVMitraALitwinASChungAKBenjaminLObjective structured assessment of cataract surgical skillArch Ophthalmol2007125336336617353407
- TaravellaMJDavidsonRErlangerMGuitonGGregoryDCharacterizing the learning curve in phacoemulsificationJ Cataract Refract Surg20113761069107521596249
- GolnikKCHaripriyaABeaverHCataract surgery skill assessmentOphthalmology20111181020942094.e2
- DooleyIJO’BrienPDSubjective difficulty of each stage of phacoemulsification cataract surgery performed by basic surgical traineesJ Cataract Refract Surg200632460460816698480
- PrakashGJhanjiVSharmaNGuptaKTitiyalJSVajpayeeRBAssessment of perceived difficulties by residents in performing routine steps in phacoemulsification surgery and in managing complicationsCan J Ophthalmol200944328428719491983
- ChristakisPGBraga-MeleRMIntraoperative performance and postoperative outcome comparison of longitudinal, torsional, and transversal phacoemulsification machinesJ Cataract Refract Surg201238223424122153315
- WoodfieldASGowerEWCassardSDRamanthanSIntraoperative phacoemulsification complication rates of second- and third-year ophthalmology residents: a 5-year comparisonOphthalmology2011118595495821539981
- SuryawanshiMGogatePKulkarniANBiradarABhomajPComparison of the posterior capsule rupture rates associated with conventional (start to finish) versus reverse methods of teaching phacoemulsificationMiddle East Afr J Ophthalmol201623216316727162446
- FischerAFPiresEMKleinFSiqueira BisnetoOSorianoESMoreiraHPrograma de ensino de facoemulsificação CBO/ALCON: resultados do Hospital de Olhos do Paraná [CBO/ALCON teaching method of phacoemulsification: results of Hospital de Olhos do Paraná]Arq Bras Oftalmol2010736517520 Portuguese21271027
- NarendranNJaycockPJohnstonRLThe Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous lossEye2009231313718327164
- BellCMHatchWVCernatGUrbachDRSurgeon volumes and selected patient outcomes in cataract surgery: a population-based analysisOphthalmology2007114340541017174399
- MisraABurtonRLIncidence of intraoperative complications during phacoemulsification in vitrectomized and nonvitrectomized eyes: prospective studyJ Cataract Refract Surg20053151011101415975471
- SalehGMTheodorakiKGillanSThe development of a virtual reality training programme for ophthalmology: repeatability and reproducibility (part of the International Forum for Ophthalmic Simulation Studies)Eye201327111269127423970027
- McCannelCAReedDCGoldmanDROphthalmic surgery simulator training improves resident performance of capsulorhexis in the operating roomOphthalmology2013120122456246123796766
- BelyeaDABrownSERajjoubLZInfluence of surgery simulator training on ophthalmology resident phacoemulsification performanceJ Cataract Refract Surg201137101756176121840683
- BaxterJMLeeRSharpJAFossAJIntensive Cataract Training Study GIntensive cataract training: a novel approachEye201327674274623598673
- PokroyRDuEAlzagaAImpact of simulator training on resident cataract surgeryGraefes Arch Clin Exp Ophthalmol2013251377778123007233
- ThomsenASBach-HolmDKjaerboHOperating room performance improves after proficiency-based virtual reality cataract surgery trainingOphthalmology2017124452453128017423
- CasswellEJSalamTSullivanPMEzraDGOphthalmology trainees’ self-assessment of cataract surgeryBr J Ophthalmol2016100676677126347527
- HardenRMGrantJBuckleyGHartIRBEME guide no. 1: best evidence medical educationMed Teach199921655356221281174
- ThomsenASSubhiYKiilgaardJFla CourMKongeLUpdate on simulation-based surgical training and assessment in ophthalmology: a systematic reviewOphthalmology2015122611111130.e125864793