Abstract
Purpose
To evaluate the outcome for scleral fixation of a foldable acrylic intraocular lens (IOL) in aphakic post-pars plana vitrectomy eyes for vitreoretinal disease.
Methods
The medical records of 15 patients were reviewed. We evaluated such factors as the underlying vitreoretinal disease, preoperative expected refraction and postoperative actual refraction, best corrected visual acuity (BCVA), corneal endothelial cell density, and intraoperative and postoperative complications.
Results
The most common cause of underlying vitreoretinal disease was retinal detachment, which was found in 8 cases. The mean refractive error was −0.10 diopters (D). The mean minimum angle of resolution (logMAR) values of BCVA were 0.27 preoperatively and 0.14 postoperatively. The mean corneal endothelial cell density was 2400 cells/mm2 preoperatively and 2187 cells/mm2 postoperatively. No significant differences were observed in either the logMAR values of BCVA or the corneal endothelial cell density before and after surgery. No intraoperative complications occurred in any of the patients. Postoperative complications occurred in a total of 7 eyes, and the most severe complications comprised 4 cases of transient ocular hypertension.
Conclusion
The results for the scleral fixation of foldable acrylic IOLs were good in aphakic post-vitrectomy eyes.
Introduction
Intraocular lenses (IOLs) are universally preferred over either aphakic spectacles or contact lenses as a method of visual rehabilitation in aphakic patients.Citation1 However, depending on the condition of the posterior capsule and ciliary zonule, the insertion of an IOL on the capsule may simply cause such problems as IOL displacement into the vitreous cavity, decentration, or tilting.Citation2 Therefore, scleral fixation of IOLs is required in some cases. However, the scleral fixation of an IOL can also lead to many complications, such as a decrease in the corneal endothelial cell density,Citation3,Citation4 refractive error after surgery,Citation5 IOL dislocation,Citation3–Citation6 vitreous hemorrhage,Citation3–Citation6 infection through the suture,Citation7 and retinal detachment.Citation3–Citation5
Although the scleral fixation of an IOL in aphakic eyes after a previous pars plana vitrectomy combined with lensectomy has become more common owing to the progress made in vitrectomy surgical techniques in recent years, only a few studiesCitation1,Citation8–Citation10 have so far been reported.
To fill this gap in knowledge, we retrospectively evaluated the secondary scleral fixation of a foldable acrylic IOL in aphakic eyes after previous pars plana vitrectomy combined with lensectomy for vitreoretinal disease.
Patients and methods
The medical records of 15 patients (15 eyes; 10 men, 5 women) who underwent scleral fixation of a foldable acrylic IOL in aphakic postvitrectomy eyes were reviewed between September 2006 and November 2009. Only one experienced surgeon of the Dokkyo Medical University Koshigaya Hospital, Saitama, Japan, performed all surgery. All patients had been followed for a minimum of 6 months (mean follow-up month ± standard deviation, 13.3 ± 6.9 months). The mean age of the patients was 63.3 ± 6.7 years. All patients had clinically significant cataracts preoperatively. The secondary implantation of an IOL was planned when the vitreoretinal disease had subsided and remained stable for a minimum of 3 months (7.2 ± 4.1 months).
The axial length was measured using the IOL Master (Carl Zeiss Meditec Co Ltd), a noncontact optical coherent biometry device. The IOL power was calculated using the SRK/T (Sanders–Retzlaff–Kraff theoretical) formula. Postoperative refraction was calculated as an awareness refraction that was converted to the spherical equivalent refraction, and the postoperative refraction, postoperative best corrected visual acuity (BCVA), and corneal endothelial cell density were measured at 6 months or longer postoperatively (15.1 ± 5.5 months).
The underlying vitreoretinal disease, preoperative expected refraction and postoperative actual refraction, preoperative and postoperative BCVA, preoperative and postoperative corneal endothelial cell density, and rate of intraoperative and postoperative complications were examined. The decimal visual acuity data were converted into logarithms of the minimum angle of resolution (logMAR) values. Transient ocular hypertension was defined as a pressure over 25 mmHg, and transient ocular hypotension was defined as that under 5 mmHg. “Transient” means a certain period of time ranging from a few days to 2 weeks at most.
Surgical technique
The surgical technique was individualized because of the complicated nature of the eyes due to a history of previous surgery. An infusion cannula utilizing a 20-gauge vitrectomy system was used to prevent eyeball collapse during surgery. The infusion cannula was placed 3.5 mm from the limbus in the inferotemporal quadrant before scleral fixation to clear the retropupillary space and maintain the intraocular pressure (IOP) during surgery. In 2 patients who had been administered intraocular silicone oil, the scleral fixation of the IOL was performed after the pars plana removal of the silicone oil.
A 3.5 mm superior scleral tunnel incision was made in all patients. The anterior chamber was filled with sodium hyaluronate 1% or sodium hyaluronate 3.0%–chondroitin sulfate 4.0%. An ab externo method with a 27-gauge needle was used. After a conjunctival peritomy was performed, 2 partial thickness limbus-based triangular scleral flaps were created opposite each other at the 8 o’clock and 2 o’clock positions. The intraocular part of the suture was pulled out through the scleral incision. The free ends of the sutures were tied to the 2 haptics at the site corresponding to the maximum spread of each haptic of a foldable acrylic IOL (VA-65BB, Hoya Corp). The VA-65BB IOL has a 6.5 mm optic, an overall length of 13.0 mm, and poly(methyl methacrylate) haptics with a microscopic indentation 1.3 mm from the tip (). The IOL was secured by slowly pulling the external sutures to introduce the haptics into the ciliary sulcus. The needle attached to the 10-0 polypropylene suture was then passed through the partial thickness of the sclera, and the suture was then tied to itself. The loop of the knot was buried under the scleral flap.
Figure 1 The foldable acrlylic intraocular lens has distended poly(methyl methacrylate) haptics, and each haptic has a microscopic indentation 1.3 mm from the tip.

After irrigation/aspiration was done to remove any residual viscoelastic material, a balanced salt solution was injected from the corneal side port to control the IOP and observe the wound adaptation. In eyes with inadequate wound sealing, a single or continuous 10-0 nylon suture was placed at the site of the scleral tunnel incision.
Statistical analysis
The paired t-test was used to compare the preoperative logMAR values at BCVA, and the corneal endothelial cell density with the postoperative values.
Results
Underlying vitreoretinal disease
The underlying vitreoretinal diseases were rhegmatogenous retinal detachment (n = 8 eyes; 53.3%); proliferative diabetic retinopathy (n = 3 eyes; 20.0%); IOL displacement into the vitreous cavity (n = 2; 13.3%); endophthalmitis after epiretinal membrane surgery (n = 1; 6.7%); and eye trauma with a vitreous hemorrhage (n = 1; 6.7%).
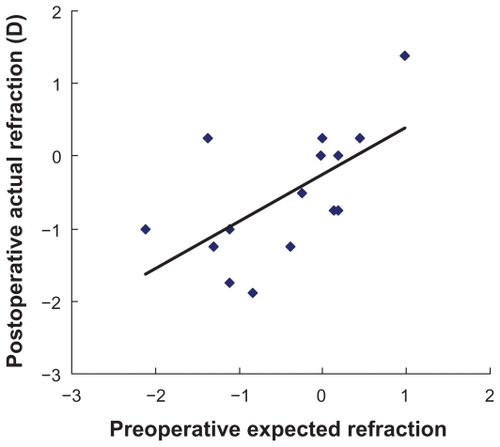
Preoperative expected refraction and postoperative actual refraction
shows a comparison of the preoperative expected refraction with the actual postoperative refraction. An average refractive error, calculated as the preoperative expected refraction from the postoperative refraction, was −0.10 ± 0.77 diopters (D) (range −1.04 to 1.62 D).
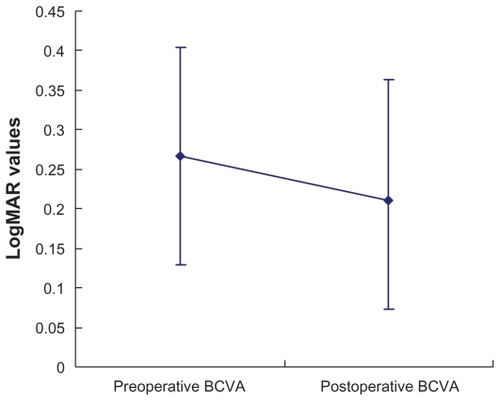
Preoperative and postoperative BCVA
The preoperative BCVAs ranged from 0.03 to 1.2, and the postoperative best corrected decimal visual acuities ranged from 0.09 to 1.2. shows the preoperative and postoperative BCVA in the logMAR value. The preoperative BCVA was 0.27 ± 0.42 (range −0.079 to 1.522), and the postoperative BCVA was 0.14 ± 0.31 (range −0.079 to 0.398). No significant difference was seen between the eyes before and after the surgery (P = 0.05; paired t-test).
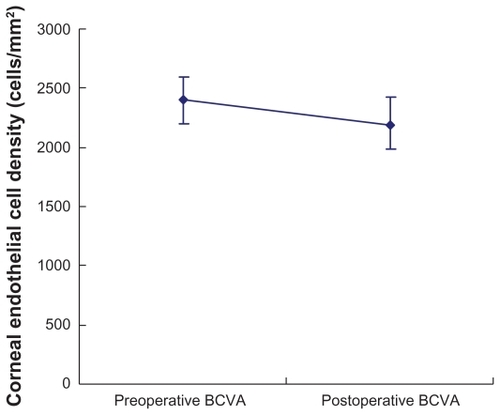
Preoperative and postoperative corneal endothelial cell density
shows the preoperative and postoperative corneal endothelial cell density. The mean preoperative corneal endothelial cell density was 2400 ± 199 cells/mm2 (range 1164 to 2653 cells/mm2), and the postoperative corneal endothelial cell density was 2187 ± 238 cells/mm2 (range 1031 to 2646 cells/mm2). No significant difference was seen between the eyes before and after surgery (P = 0.10; paired t-test).
Intraoperative and postoperative complications
No intraoperative complications occurred. The postoperative complications were transient ocular hypertension (n = 4); transient ocular hypotension (n = 1); IOL dislocation (n = 1); and vitreous hemorrhage (n = 1). Because there was some overlap in these cases, we counted the total number of eyes. Although transient ocular hypertension, transient ocular hypotension, and vitreous hemorrhage resolved without treatment during the observation course, the 2 eyes with IOL dislocation required further surgery to repair the dislocation. The one eye that had iris capture is still under close observation.
Discussion
The actual refractive errors reported in a previous study on the scleral fixation of IOLs in aphakic vitrectomized eyes were observed to shift approximately −0.8 (D) toward myopia in comparison with the findings observed after normal cataract surgery.Citation9 These data are useful because used IOLs were previously limited to AQ-110NV and have been studied in many cases.Citation9 Hotta and Hotta, in their investigation, limited the used IOLs to only one kind and focused on refractive errors.Citation9 No controls were included in this study, thus leading to a slight shift toward myopia. However, as the refractive error was over ±1.50 (D) for only 2 eyes, we therefore considered these findings to be representative of good results.
In a previous study on the scleral fixation of the intraocular lenses in aphakic vitrectomized eyes reported by Ahn et al, which was similar to our present study, the postoperative BCVA significantly improved in comparison with the preoperative BCVA after 6 months.Citation10 The postoperative BCVA was measured at 6 months or later postoperatively, and no significant difference was observed in the eyes of these patients in comparison with the preoperative BCVA described in this study.
Ohtani et al divided scleral fixation of IOL into 2 groups and compared the first group of being continuously performed after cataract surgery with the secondary group of being performed a few days after surgery.Citation3 The postoperative corneal endothelial cell density significantly decreased at 12 months after the surgery compared with that observed before the surgery in both groups. However, no significant differences were observed between the groups.Citation3 The postoperative corneal endothelial cell density was measured at 6 months or more postoperatively, and no significant difference in the eyes of these patients was seen in comparison with the preoperative corneal endothelial density described in this study.
Shimomura et al reported that ocular hypertension occurred in 8 of 19 eyes after scleral fixation of the IOL, but none of the eyes required glaucoma surgery.Citation11 Krause et al reported that ocular hypertension occurred in 52 of the 119 eyes in their study after scleral fixation of the IOL, and 11 of these eyes needed subsequent glaucoma surgery.Citation4 Fortunately, none of the eyes needed glaucoma surgery in this study. Pre-existing glaucoma tended to occur in association with the ocular hypertension, but pars plana infusion lowered the rate of ocular hypertension after surgery.Citation4 Pars plana infusion was used in all cases in this study. No ocular hypertension after surgery occurred in any of the patients. To reduce postoperative complications, such as retinal detachment in scleral fixation of the IOL, the use of pars plana vitrectomy without severe vitreoretinal disease has lately been growing in popularity.Citation11 Because pars plana vitrectomy itself may pose additional risks, more study is needed to establish the efficacy of the pars plana vitrectomy modality without any evidence of severe vitreoretinal disease.
Ahn et al reported the underlying vitreoretinal diseases in 21 eyes of patients who underwent scleral fixation of an IOL in aphakic vitrectomized eyes to be proliferative diabetic retinopathy in 9 eyes; proliferative vitreoretinopathy in 5 eyes; traumatic retinal detachment in 3 eyes; intraocular foreign body in 2 eyes; and uveitic retinal detachment in 2 eyes.Citation10 Hotta and Hotta also reported the underlying vitreoretinal diseases, which included retinal detachment in 17 eyes; diabetic retinopathy in 7 eyes; and other causes in 6 eyes.Citation9 Ahn et al reported a higher rate of proliferative diabetic retinopathyCitation10 in comparison with this study. On the other hand, the findings reported by Hotta and HottaCitation9 were similar to those described in this study with regard to the underlying vitreoretinal diseases.
The VA-65BB, which is a foldable IOL that can be inserted through a 3.0 mm incision, was used in this study. Fass and Herman reported that large incisions were prone to demonstrate either intraoperative or postoperative hypotony, an especially dangerous situation for eyes that were essentially empty of any vitreous support.Citation8 As P366UV and CZ70BD IOLs require large incisions, their frequency of use may decrease in the future. Fass and Herman described a surgical technique for aphakic postvitrectomy eyes in which a foldable acrylic IOL was used to facilitate 4-point fixation with no tilt and good centration through a 2.75 to 3.0 mm incision.Citation8
Scleral fixation of the IOL tends to prolong the duration of surgery, thus resulting in a longer illumination of the retina by the surgical microscope. This is a risk factor for light-induced retinopathy.Citation12 As yellow IOL protects the retina against light exposure,Citation13 the use of a yellow IOL, either with or without pars plana vitrectomy, will therefore likely increase in the future.
There are several studies in the literature similar to this report.Citation1,Citation10 However, one important advantage of our study in comparison with the others is the fact that only one experienced surgeon performed all the surgery. Some differences tend to occur when different surgeons perform a large amount of surgery and thus result in reduced accuracy.
The removal of a cataract during a vitrectomy is performed to improve the surgeon’s visualization. The lens capsule was removed completely during vitrectomy. It is possible to maintain the part of anterior capsule for subsequent foldable IOL implantation without sutures. However, the remaining anterior capsule has a risk of developing irido-capsular synechias, which may complicate the secondary IOL implantation and also negatively affect the occurrence of postoperative refractive errors.
However, only a few studies of this kindCitation1,Citation8–Citation10 have so far been reported, and the findings presented in this study are therefore considered to be useful. We conclude that scleral fixation of foldable acrylic IOLs in aphakic post-vitrectomy eyes can be safely performed because no severe problems have been found with regard to refraction, corneal endothelial cell density, or intraoperative and postoperative complications.
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- JohnstonRLCharterisDGPars plana vitrectomy and sutured posterior chamber lens implantationCurr Opin Ophthalmol20011221622111389350
- IinoTOhshitaMYamamotoTAb externo sulcus fixation by single unilateral suture of the intraocular lens hapticsGanka20054713351340
- OhtaniSMiyataKOnoKOutcome of sulcus fixation of the posterior chamber lensJpn J Clin Ophthalmol200054531535
- KrauseLBechrakisHeimannHImplantation of scleral fixed sutured posterior chamber lens: a retrospective analysis of 119 casesInt Ophthalmol20092920721218401553
- TsuikiETaniguchiHKitaokaTEvaluation of transscleral fixation of intraocular lensGanka Rinsyo Ihou20049810771080
- GaneshAAl-ZuhaibiSMitraSVisual rehabilitation by scleral fixation of posterior chamber intraocular lens in Omani children with aphakiaOphthalmic Surg Lasers Imaging20094035436019634738
- TashitaAMitamuraYOhtsukaKA case of endophthalmitis 8 years after transscleral fixation of intraocular lensAtarashii Ganka200421258260
- FassONHermanWKSutured intraocular lens placement in aphakic post-vitrectomy eyes via small-incision surgeryJ Cataract Refract Surg2009351492149719683142
- HottaKHottaJPostoperative refractive error of secondary intraocular lens implantation after simultaneous vitrectomy and lensectomyGanka Rinsyo Ihou2006100227230
- AhnJKYuHGChungHTransscleral fixation of a foldable intraocular lens in aphakic vitrectomized eyesJ Cataract Refract Surg2003292390239614709302
- ShimomuraCYamadaTNosoKCause and outcome of scleral fixation of intraocular lensJpn J Clin Ophthalmol20076114091412
- MutohTMatsumotoYChikudaMTwo cases of light-induced retinopathy during scleral fixation of intraocular lensGanka20095118171821
- TanitoMKaidzuSAndersonREProtective effects of soft acrylic yellow filter against blue light-induced retinal damage in ratsExp Eye Research20068314931504