Abstract
Pseudoexfoliation is a ubiquitous syndrome of multifactorial origin affecting elderly people by increasing the risk of cataract and secondary glaucoma development. Despite modern techniques and technologies for cataract surgery, pseudoexfoliation syndrome represents a challenge for surgeons because of the increased weakness of the zonular apparatus and limited pupil dilation. Due to the inherent difficulties during surgery, the risk of vitreous loss in these patients is several times higher than in cataract patients without pseudoexfoliation. Using currently available surgical devices (ophthalmic viscosurgical device, iris retractors and ring dilators, capsular tension ring, etc.), the risk of intraoperative complications may be much reduced, allowing the surgeon to handle difficult cases with greater confidence and safety. This review analyzes the methodologic approach to the patient with zonular laxity with the aim of providing useful advices to limit the risks of intraoperative and postoperative complications. From the preoperative planning, to the intraoperative management of the small pupil and phacodonesis, and to the postoperative correction of capsule phimosis and intraocular lens dislocation, a step approach to the surgical management of pseudoexfoliation patients is illustrated.
Introduction
Cataract still remains the world’s leading cause of blindness and visual impairment in the elderly population, despite the decreasing number of people affected.Citation1 If age is the main risk factor for cataract progression, pseudoexfoliation syndrome (PXF) represents an independent additional hazard for the development of nuclear sclerosis and indication for cataract surgery.Citation2,Citation3
PXF syndrome is a multifactorial, genetically determined, age-related and environmentally influenced disorder of the elastic fiber structure, characterized by excessive production and accumulation of an elastotic material within a multitude of intra and extraocular tissues.Citation4 For this reason, PXF is a diffuse disease with ocular and systemic manifestations.
In all populations, the prevalence of PXF increases markedly with age as the deposition of the typical white fibrillar material, that characterizes this disease, progressively accumulates during life. With an occurrence as low as 0% in the middle age group (49–54 years), this value increases up to 6.25% among elderly patients of 85 years or more in the Australian populationCitation2 and up to 5% in the USA,Citation5 with both men and women equally affected. Also known as the “Viking disease”, PXF is more common in Scandinavia and in other Northern Europeans with low climatic temperature, though the disease is reported in all population types and races.Citation6,Citation7 It is estimated that in Sweden, an 87-year-old individual has 61% chance of having PXF.Citation8
Pseudoexfoliation is diagnosed by the deposition of white, “dandruff-like”, fluffy material, virtually in all the structures of the human eye, but more importantly in the anterior segment: corneal endothelium, anterior capsule, lens zonules, iris, and trabecular meshwork. The material is composed of amyloid, laminin, elastic fibers, collagen, and basement membrane.Citation9,Citation10 The same material seen in the ocular district has been found in other parts of the human body such as heart, lung, liver, kidney, cerebral meninges, and blood vessels,Citation11 indicating that PXF is a multiorgan disease. This may explain why patients with ocular PXF may present a history of systemic hypertension, abdominal aorta aneurysm, angina, cardiovascular disease, and stroke.Citation12,Citation13 Despite all these, life expectancy does not differ between persons with and without PXF.Citation14
The pathogenesis of PXF is multifactorial, where geographical and environmental factors, together with genetic predisposition, explain the different incidence of this syndrome across the world. A documented association with mutations in the lysyl oxidase-like 1 gene (LOXL1) at the locus 15q22,Citation15 which codes for elastic fiber components of extracellular matrix, suggests a genetic factor for the inheritance of this disease. For this reason, it has been suggested that PXF is a form of elastosis resulting from the overproduction of elastic microfibrillar components such as fibrillin-1.Citation16 The systemic origin of the disease explains why patients with unilateral involvement manifest PXF signs in the normal fellow eye at a later time, indicating that PXF is a generalized, bilateral disorder with a markedly asymmetric clinical presentation at onset. Patients with unilateral signs of the disease are usually younger than those with bilateral involvement.
PXF is generally recognized late in life as the course of the disease is for long time subclinical and the degree of ocular involvement and visual loss is often asymmetrical or more rarely unilateral. The diagnosis of PXF is of paramount importance as this disease is a major risk factor for complications during cataract surgery and the most frequent cause of secondary glaucoma.Citation17 Intraoperative and postoperative complications may arise from the weakened capsule and zonular apparatus (zonulopathy) secondary to the progressive proteolytic disintegration of the suspensory ligament, responsible for the instability of the crystalline lens during surgery, capsular rupture, zonular dialysis, vitreous loss, nuclear luxation, decentration or dislocation of the intraocular lens (IOL) with time. Further difficulties during surgery result from poor or inadequate pupil dilation (iridopathy), secondary to atrophic changes of the iris sphincter and stroma characterized by transillumination defects. Postoperative anterior chamber inflammation and fibrinous reaction occur frequently in PXF patients due to an acquired weakened blood-aqueous barrier.Citation18 Corneal endothelial morphological and functional changes (endotheliopathy) are seen in eyes affected with PXF, explaining the greater susceptibility of these eyes to surgical trauma, resulting in transitory and permanent corneal decompensation.Citation19
Modern techniques and instruments for cataract surgery have profoundly improved the confidence toward the surgical approach and operative management of PXF cases; however, the higher risk of complications with surgery still suggests the need for greater expertise and surgical skill for these patients.Citation17 The aim of this paper is to review the surgical approach to the pseudoexfoliative cataract, in light of current scientific knowledge and modern surgical techniques, specifically addressing the management of patients at preoperative, intraoperative, and postoperative steps.
Preoperative
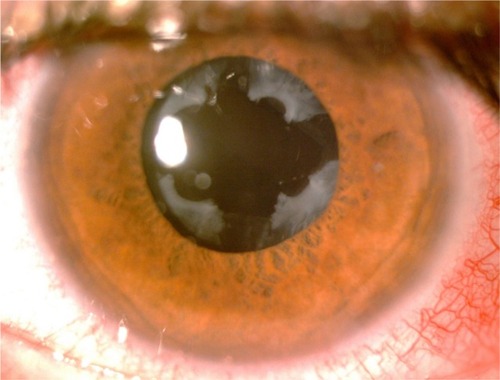
The signs of PXF can be identified on slit-lamp examination. Biomicroscopy, after pupil dilation, has a high sensitivity and specificity on recognizing the presence of fibrillar material over the lens surface and iris even at early stages of the disease. The diagnosis of PXF is based on slit lamp observation of the typical gray-white flakes at the pupillary margin and fibrillary deposits over the anterior lens capsule, mostly concentrated in the pupillary area, often separated from the peripheral residues by a clear zone (). Sometimes in the presence of an advanced cataract, with a dimmed red reflex, signs of PXF are more difficult to identify as the whitish flakes do not contrast with the color of the lens. Once the diagnosis of cataract and the indication for surgery have been established, signs of reduced zonular integrity should be explored in order to assess the risk of complications during surgery. The degree of zonular laxity does not strictly correlate with the amount and extension of pseudoexfoliative material visible over the lens surface, but more with the age of the patient. Typical signs of zonular weakness are phacodonesis, with eye movements, and sometimes a reduction of the anterior chamber depth due to a forward shift of the lens. Changes in anterior chamber depth may be localized when zonular dehiscence develops involving only some hours of the capsular lens ligament. The incidence of phacodonesis and/or lens subluxation has been reported between 8.4% and 10% in PXF patients.Citation20
Figure 1 Slit lamp photograph showing signs of cataract and pseudoexfoliation.
Iridodonesis in the presence of phacodonesis is often less remarkable in PXF probably due to an increased rigidity of the ischemic atrophic iris.Citation21 Poor pupil dilation is expected in most patients with PXF due to extracellular infiltration and degeneration of the dilator and sphincter muscles with atrophy of the pigment epithelium and stroma.Citation22 In some cases, the formation of posterior synechiae further reduces the response to mydriatics.Citation23 The degree of maximum pupil dilation should be addressed preoperatively to ensure adoption of appropriate surgical measures. Among these, preoperative nonsteroidal anti-inflammatory drugs (NSAIDs) may be given to help maintain maximum achievable pupil dilation during surgery.Citation24
Specular microscopy studies in eyes with and without PXF reported an endothelial cell count 5% to 9% lower than in age-matched controls.Citation19,Citation25 In PXF patients, not only the cell density but also the cell morphology is altered with a decrease of cell hexagonality and an increase of coefficient of variation. PXF endotheliopathy may result from several causes of direct and indirect damage to the endothelial cells. Accumulation of PXF material between endothelial cells and Descemet’s membrane is a possible cause of direct cellular degeneration,Citation26,Citation27 whereas elevated intraocular, iris ischemia and increased flare intensity, caused by blood-aqueous barrier breakdown, may indirectly alter the homeostasis of endothelial cells.Citation28,Citation29 For the above-mentioned reasons, variations of endothelial cell morphology and density are expected to be funded preoperatively in patients with PXF, and they may be responsible for an increased risk of corneal decompensation after surgery.Citation30
Raised intraocular pressure is frequently expected in patients with PXF and the prevalence of glaucoma has been reported as high as 26% and up to 49% at the time of cataract surgery.Citation31,Citation32 PXF is the most frequent cause of secondary glaucoma as the results of an increased outflow resistance due to the chronic deposition of pigmented material freed from iris and in addition of exfoliative material throughout the tra-becular meshwork, Schlemm canal and collector channels.Citation33 The estimated incidence of glaucoma in PXF patients is three to four times greater in patients with than without PXF.Citation34,Citation35 Owing to the high level of the intraocular pressure exhibited in these patients, the risk of glaucoma development and progression is elevated.Citation36 Kim et alCitation37 found that PXF patients present a thinner and possibly weaker lamina cribrosa, suggesting a particular susceptibility of these patients to the development of optic nerve cupping. Whether or not cataract surgery may protect against the development of glaucoma in PXF is debatable. According to some studies, the prolonged pressure-lowering effect occurring after surgery may reduce the risk of glaucoma developing over time.Citation38,Citation39
Intraoperative
In the era of phacoemulsification, PXF still represents a relevant challenge for the surgeon. The concurrent presence of poor pupil dilation and zonular weakness is responsible for the increased risk of intraoperative complications that may occur during surgery more frequently than in cataractous eyes without PXFCitation17 ().
Table 1 Preoperative risk factors and intraoperative and postoperative complications in PXF patients with cataract surgery
Minimum sufficient pupil dilation (4–5 mm) may be achieved using a highly viscous cohesive ophthalmic viscosurgical device (OVD) or a combination of two OVDs with different rheological properties. In this case, a dispersive OVD is placed first to coat the corneal endothelium, and then a cohesive OVD is injected centrally to deepen the anterior chamber, flatten the anterior lens capsule, and maintain adequate pupil mydriasis in order to facilitate capsulorhexis creation.Citation40 It is worth noting that in the presence of a weak zonular apparatus, over-inflating of the anterior chamber may cause stretching and further damage to the zonules.
Posterior synechiae, if present, should be lysed with a blunt spatula and at the same time pupil may be mechanically stretched using two iris manipulators. Careful manipulation is required due to the ischemic fragile iris in PXF patients. Whenever pupil dilation with OVD provides an insufficient view of the cataract, adequate mydriasis can be achieved using iris hooks or pupillary rings to ensure ample and stable dilation throughout surgery.Citation41
The degree of zonular weakness may be assessed as soon as the surgeon begins the capsulorhexis. Difficulties on puncturing the anterior capsule are the first sign of a diminished anterior capsule tension. In this case, a 25-gauge sharp needle bent at the tip may help perform the initial capsulotomy, with minimal pressure applied to the zonular apparatus. Furthermore, in the case of severe zonular weakness, capsule tearing may result due to the lack of resistance forces counteracting the pull of the rhexis forceps, leading to the creation of an excessively small capsulotomy that may complicate phacoemulsification. Using a bimanual technique, counteraction may be achieved with an iris hook, placed to engage the already torn anterior capsule, while forceps continue the capsulorhexis. Ideally, a well-centered 5–6 mm circular continuous capsulorhexis should be adequate to provide access to phacoemulsification maneuvers, IOL support, and implantation of devices that aid in the maintenance of capsular stability during and after surgery.
The presence of whitish scaly material over the lens surface may be mistaken for the anterior capsule layer with the difference that these are typically fragile and tear abnormally when compared with the true anterior capsule. The use of trypan blue to stain the anterior capsule may help recognize this layer when in doubt.Citation42,Citation43 Following a complete capsulorhexis, viscodissection, prior to hydrodissection, allows better corticocapsular cleavage than hydrodissection alone, making cortex removal easier and safer by reducing traction on the lens zonules.
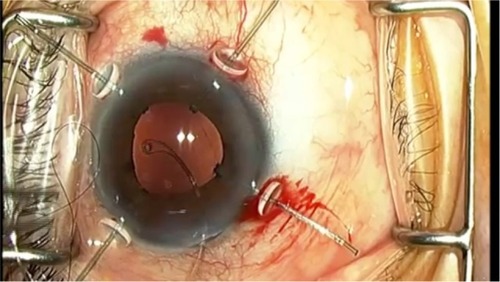
Depending on the severity of the zonular instability, the surgeon may use a capsular tension ring (CTR) and/or capsular retractors to support the capsular bag during all steps of phacoemulsification, cortical cleaning, and IOL implantation. In the case of extensive zonular dialysis, more than one device may be employed. Capsule retractors help support the zonular-lens complex in the anteroposterior direction, facilitating hydrodissection and cataract fragmentation, while CTR allows even distension of the capsular bag, supporting areas of zonular dehiscence by redistributing the zonular tension around the capsule and allowing optimal IOL centration. Several reports have shown that CTR implant reduces intraoperative complication in PXF eyes, suggesting the use of this device in cases of mild zonulopathy and phacodonesis.Citation44–Citation46 In the case of more extensive zonular weakness, CTR alone may not prevent intraoperative or postoperative late dislocation of the IOL-bag complex. In these cases, capsule retractors should be used during all steps of hydrodissection and phacoemulsification () followed by the implantation of a modified CTR sutured to the sclera to assure anteroposterior stability of the IOL-bag complex.Citation47
Figure 2 Intraoperative photograph showing capsule retractors stenting the capsular bag during phacoemulsification.
Phacoemulsification technique is not dissimilar from the one routinely used for other complicated cataract cases. The “chop technique”, using vertical and horizontal chopping, allows minimum zonular stress with the advantage of restraining surgical maneuvers to the center of the anterior chamber, avoiding the capsule equator and the pupil. Vitreous prolapse from a zonule defect may be present before surgery or occur during surgery at any time. Limited anterior vitrectomy and tamponade using a cohesive OVD help complete cataract removal and cortex aspiration. Filling the anterior chamber with OVD before removing instruments from the eye prevents collapsing with further anterior herniation of vitreous. In a retrospective comparative study conducted on a large series of cataract procedures, Shingleton et alCitation48 reported a 4% frequency of vitreous loss in PXF patients compared to 0% in patients without PXF. Authors of this paper attributed the causes of vitreous loss to zonular weakness rather than capsule tears in these patients. A review study of surgical complications during phacoemulsification reported a 10% risk of vitreous loss and capsule rupture in PXF patients.Citation17
Lens cortex removal may be difficult and traumatic for the capsule and zonules. The presence of a CTR has the controversial effect of helping cortex removal by stenting the capsular equator, facilitating its separation from the capsule, and at the same time lens cortex may make it more difficult to aspirate when trapped behind a capsular tension device. Profuse and repeated cortical hydration may help soften cortex material and facilitate its aspiration. In all cases, slow-motion careful tangential stripping, in combination with gentle centripetal traction, should allow for accurate cortical removal.Citation49
The choice of the IOL to implant in PXF patients is related to the evaluation of the state and future risk of capsular instability. In the presence of zonular weakness, following a CTR implant, a one-piece or three-piece acrylic IOL may be implanted according to the surgeon preference. One-piece IOL requires less manipulation and carries a lower probability of damage to the capsule and zonules and therefore may be considered the IOL of choice in these patients. In consideration of the risk of capsule contraction and IOL decentration, toric IOLs, as well as multifocal IOLs, constitute a possible cause of early or late unsatisfactory visual outcome. Likewise, any IOL placed in the sulcus should be avoided in PXF patients due to the probability of decentration and posterior dislocation. When a complete capsular diaphragm is missing, any anterior chamber angle-supported IOL should not be implanted in consideration of the elevated risk of glaucoma and corneal decompensation secondary to endothelial cell abnormalities.
Postoperative
A complicated postoperative course may be expected in PXF patients due to the abnormalities of the ocular structures and to the difficulties encountered during surgery ().
A higher degree of postoperative anterior chamber inflammation is expected in PXF due to the chronic alteration of the blood-aqueous barrier that accompanies the iris ischemic changes seen in these patients. At preoperative, patients with PXF show a baseline level of aqueous protein concentration several times greater than what is measured in cataractous eyes without PXF.Citation50,Citation51 Due to the probability of protracted and complicated surgery, with iris manipulation and possible vitreous loss, severe postoperative fibrinous uveitis is frequently expected in these patients. As a result of the intense and prolonged inflammation posterior synechiae, capsule contraction and cystoid macular edema may complicate the postoperative course of PXF patients. Topical NSAIDs after surgery have proved effective in reducing the amount of aqueous protein release and the percentage of patients showing increased macular thickness.Citation52 Pressure spikes may occur as result of aqueous protein release and are more frequently seen in patients with pre-existing glaucoma.
An increased risk of endothelial cells loss may be expected in PXF as a result of more complicated and prolonged surgery, often requiring complex manipulation of cataract, iris, and IOL. A three times greater percentage of endothelial cell loss is estimated in patients with PXF.Citation25 However, despite the abnormal endothelium seen in these patients, the risk of irreversible corneal decompensation with surgery is low.Citation19
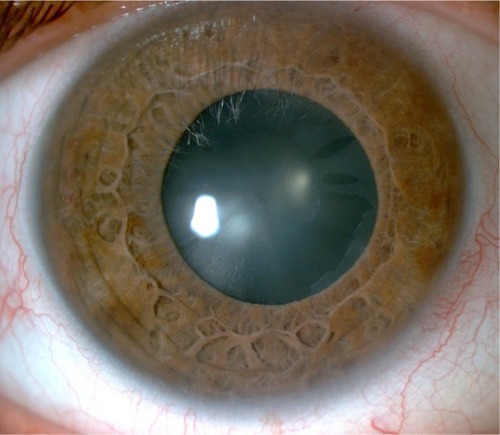
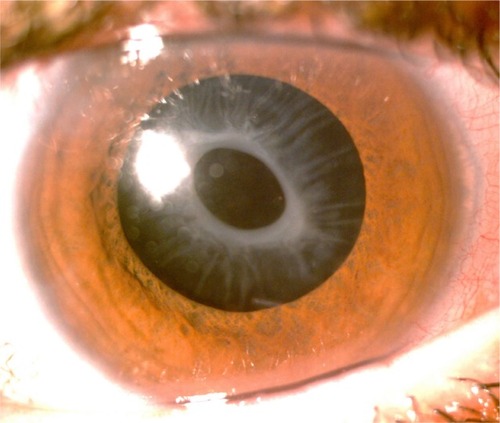
Capsular phimosis with IOL decentration and late in-the-bag IOL dislocation are among the most dreaded complications occurring after surgery (). Capsular shrinkage determines centripetal traction on the weakened lens zonules, inducing tilt and decentration of the IOL with possible dislocation of the entire IOL-bag complex. Radial anterior relaxing Nd:YAG laser capsulotomy allows the release of the capsular traction over the peripheral zonules, thus potentially avoiding or delaying dislocation of the IOL in the vitreous cavity (). Laser or surgical capsulotomy should be performed as soon as the capsular opening starts to shrink in order to avoid worsening of zonular damage.Citation53
Figure 3 Slit lamp photograph showing anterior capsule opacification and phimosis after cataract surgery with in-the-bag IOL implantation.
Abbreviation: IOL, intraocular lens.
Conclusion
Cataract surgery in settings of PXF carries a significant risk of complications in the form of capsule rupture, vitreous loss, nucleus luxation, and IOL dislocation. PXF material involving most ocular tissues determines progressive weakening of the zonular ligament with consequent loss of lens stability. A planned approach to cataract surgery using the advanced techniques of phacoemulsification, specific OVDs, and capsule support devices significantly reduces the risk of complications during surgery. Postoperative surveillance is required to monitor and treat postoperative intraocular pressure, anterior chamber inflammation, IOL decentration, and cystoid macular edema.
Employing all these measures, cataract surgery can yield satisfactory visual outcomes in PXF patients.
Disclosure
The authors report no conflicts of interest in this work.
References
- BourneRRStevensGAWhiteRACauses of vision loss worldwide, 1990–2010: a systematic analysisLancet201316e339e34925104599
- KanthanGLMitchellPBurlutskyGRochtchinaEWangJJPseudoexfoliation syndrome and the long-term incidence of cataract surgery: the Blue Mountains eye studyAm J Ophthalmol201315518388.e123036566
- EkströmCBotling TaubeAPseudoexfoliation and cataract surgery: a population-based 30-year follow-up studyActa Ophthalmol201593877477726095907
- Schöltzer-SchrehardtUPseudoexfoliation syndrome: the puzzle continuesJ Ophthalmic Vis Res20127318718923264859
- HillerRSperdutoRDKruegerDEPseudoexfoliation, intraocular pressure and senile lens changes in a population-based surveyArch Ophthalmol19821007108010827092647
- AasvedHThe geographical distribution of fibrillopathia epitheliocapsularis, so-called senile exfoliation or pseudoexfoliation of the anterior lens capsuleActa Ophthalmol (Copenh)19694737928105394642
- ThyghesenJPrevalence and distribution of exfoliation syndromeGlaucoma Topics Trends2006456
- AströmSStenlundHLindénCIncidence and prevalence of pseudoexfoliation and open-angle glaucoma in northern Sweden: II. Results after 21 years of follow-upActa Ophthalmol Scand200785883283717986292
- ParekhPGreenWRStarkWJAkpekEKElectron microscopic investigation of the lens capsule and conjunctival tissues in individuals with clinically unilateral pseudoexfoliation syndromeOphthalmology20081154614619.e217698197
- ConwayRMSchöltzer-SchrehardtUKüchleMNaumannGOPseudoexfoliation syndrome: pathological manifestations of relevance to intraocular surgeryCin Exp Ophthalmol2004322199210
- Schöltzer-SchrehardtUMKocaMRNaumannGOVolkholzHPseudoexfoliation syndrome. Ocular manifestation of a systemic disorder?Arch Ophthalmol199211012175217561463418
- SchumacherSSchöltzer-SchrehardtUMartusPLangWNaumanGOPseudoexfoliation syndrome and aneurysm of the abdominal aortaLancet2001357925335936011211000
- MitchellPWangJJSmithWAssociation of pseudoexfoliation syndrome with increased vascular riskAm J Ophthalmol199712456856879372724
- SvenssonREkstromCPseudoexfoliation and mortality: a population-based 30-year follow-up studyActa Ophthalmol201593216216424674619
- ThorleifssonGMagnussonKPSulemPCommon sequence variants in the LOXL1 gene confer susceptibility to exfoliation glaucomaScience200731758431397140017690259
- RitchRSchlötzer-SchrehardtUExfoliation (pseudoexfoliation) syndrome: toward a new understanding. Proceedings of the first International Think TankActa Ophthalmol Scand200179221321711284770
- Vazquez-FerreiroPCarrera-HuesoFJPoquet JornetJEFikri-BenbrahimNDiaz-ReyMSanjuan-Cervero’RIntraoperative complications of phacoemulsification in pseudoexfoliation: meta-analysisJ Cataract Refract Surg201642111666167527956295
- WalinderPEOliviousEONordellSIThoburnWEFibrinoid reaction after extracapsular cataract extraction and relationship to exfoliation syndromeJ Cataract Refr Surg1989155526530
- WirbelauerCAndersNPhamDTWollensakJCorneal endothelial cell changes in pseudoexfoliation syndrome after cataract surgeryArch Ophthalmol199811621451499488264
- MorenoJDuchSLajaraJPseudoexfoliation syndrome: clinical factors related to capsular rupture in cataract surgeryActa Ophthalmol (Copenh)19937121811848333262
- BartholomewRSLens displacement associated with pseudocapsular exfoliationBr J Ophthalmol197054117447505484741
- RepoLPNaukkarinenAPaljarviLTerasvirtaMEPseudoexfoliation syndrome with poorly dilating pupil: a light and electron microscopic study of the sphincter areaGraefes Arch Clin Exp Ophthalmol199623431711768720716
- MardinCYSchöltzer-SchrenhardtUNaumannGO“Masked” pseudoexfoliation syndrome in unoperated eyes with circular posterior synechiae: clinical-electron microscopic correlationArch Ophthalmol2001119101500150311594951
- Rodriguez-GarciaAHernandez-CamarenaJCLopez-JaimeGRNava-GarciaJAEffect of topical nonsteroidal anti-inflammatory drugs on pupillary size during uncomplicated cataract surgeryJ Refract Surg201733423624228407163
- HayashiKManabeSYoshimiraKKondoHCorneal endothelial damage after cataract surgery in eyes with pseudoexfoliation syndromeJ Cataract Refr Surg2013396881887
- Schöltzer-SchrehardtUMDörflerSNaumannGOCorneal endothelial involvement in pseudoexfoliation syndromeArch Ophthalmol199311156666748489451
- NaumannGOSchöltzer-SchrehardtUKeratopathy in pseudoexfoliation syndrome as a cause of corneal endothelial decompensation: a clinicopathologic studyOphthalmology200010761111112410857831
- AsanoNSchöltzer-SchrehardtUNaumannGOA histopathologic study of iris changes in pseudoexfoliation syndromeOphthalmology19951029127912909097764
- KückleMVinoresSAMahlowJGreenWRBlood-aqueous barrier in pseudoexfoliation syndrome: evaluation by immunohistochemical staining of endogenous albuminGraefes Arch Clin Exp Ophthalmol1996234112188750845
- QuirogaLLansinghVCSamudioMPenaFYCarterMJCharacteristics of the corneal endothelium and pseudoexfoliation syndrome in patients with senile cataractClin Exp Ophthalmol201038544945520456430
- YildrimNYasarEGursoyHColakEPrevalence of pseudoexfoliation syndrome and its association with ocular and systemic diseases in Eskisehir, TurkeyInt J Ophthalmol201710112813428149789
- DroslumLHaaskjoldEDavangerMPseudoexfoliation syndrome and extracapsular cataract extractionActa Ophthalmol (Copenh)19937167657708154250
- Schöltzer-SchrehardtUNaumannGOTrabecular meshwork in pseudoexfoliation syndrome with and without open-angle glaucoma. A morphometric, ultrastructural studyInvest Ophthalmol Vis Sci1995369175017647635652
- AströmSLindénCIncidence and prevalence of pseudoexfoliation and open angle glaucoma in northern Sweden: I. Baseline reportActa Ophthalmol Scand200785882883117986290
- EkströmCElevated intraocular pressure and pseudoexfoliation of the lens capsule as risk factors for chronic open-angle glaucoma. A population-based five-year follow-up studyActa Ophthalmol (Copenh)19937121891958333264
- VestiEKiveläTExfoliation syndrome and exfoliation glaucomaProg Retin Eye Res200019334536810749381
- KimSSungKRLeeJRLeeKSEvaluation of lamina cribrosa in pseudoexfoliation syndrome using spectral-domain optical coherence tomography enhanced depth imagingOphthalmology201312091798180323622874
- ShingletonBJLaulANagaoKEffect of phacoemulsification on intraocular pressure in eyes with pseudoexfoliation: single surgeon seriesJ Cataract Refract Surg200834111834184119006727
- KristianslundOØsternAERåenMSandvikGFDroslumLDoes cataract surgery reduce the long-term risk of glaucoma in eyes with pseudoexfoliation syndrome?Acta Ophthalmol201694326126526749122
- ArshinoffSADispersive-cohesive viscoelastic soft shell techniqueJ Cataract Refract Surg19992521671739951659
- HashemiHSeyedianMAMohammadpourMSmall pupil and cataract surgeryCurr Opin Ophthalmol20152613925390859
- WollensakGWollensakJDouble contour of the lens capsule edges after continuous curvilinear capsulorhexisGraefes Arch Clin Exp Ophthalmol199723542042079143887
- GreenburgDLCoanEBCapsule-splitting phenomenon during capsulorhexis in pseudoexfoliationJ Cataract Refract Surg20154161306130926100956
- JacobSAgarwalAAgarwalAAgarwalSPatelNLalVEfficacy of a capsular tension ring for phacoemulsification in eyes with zonular dialysisJ Cataract Refract Surg200329231532112648643
- PriceFWJrMackoolRJMillerKMKochPOettingTAJohnsonATInterim results of the United States investigational device study of the ophthec capsular tension ringOphthalmology2005112346046515745774
- BayractarSAltanTKucuksumerYYilmazOFCapsular tension ring implantation after capsulorhexis in phacoemulsification of cataracts associated pseudoexfoliation syndrome; intraoperative complications and early postoperative findingsJ Cataract Refract Surg200127101620162811687362
- CionniRJOsherRHManagement of profound zonular dialysis or weakness with a new endocapsular ring designed for scleral fixationJ Cataract Refract Surg19982410129913069795841
- ShingletonBJHeltzerJO’DonoghueMWOutcomes of phacoemulsification in patients with and without pseudoexfoliation syndromeJ Cataract Refract Surg20032961080108612842671
- MansourAMAntoniosRSAhmedIICentral cortical cleanup and zonular deficiencyClin Ophthalmol2016101919192327784979
- Coca-PradosMThe blood-aqueous barrier in health and diseaseJ Glaucoma201423Suppl 1S36S3825275903
- KuckleMNguyenNXHannappelENaumannGOThe blood-aqueous barrier in eyes with pseudoexfoliation syndromeOphthalmic Res199527Suppl 1136142
- CoassinMIovienoASoldaniABromfenac ophthalmic solution 0.09% as an adjunctive therapy to topical steroids after cataract surgery in pseudoexfoliation syndrome: a randomized clinical trialJ Cataract Refract Surg20164281119112527531286
- LiuEColeSWernerLHengererFMammalisNKohnenTPathologic evidence of pseudoexfoliation in cases of in-the-bag intraocular lens subluxation or dislocationJ Cataract Refract Surg201541592993525935341