Abstract
Purpose
To analyze factors related to long-term progression of visual field defects (VFD) in patients with normal tension glaucoma (NTG) under medical therapy.
Patients and methods
Clinical data from 622 eyes of 311 primary open-angle glaucoma and NTG patients were collected from April 2006 to March 2016. Of these patients, those with normal intraocular pressure (IOP); glaucomatous VFD judged by Anderson’s criteria; corrected visual acuity ≥0.7; receiving more than 6 years medical therapy; having undergone ≥10 visual field tests performed at 6-month intervals using a Humphrey field analyzer (Swedish Interactive Threshold Algorithms standard, C 24-2 program); and having reliability coefficients of visual field testing <33% and mean deviation (MD) more than −20 decibels in the initial visual field test were included in data analysis. The relationship between MD slope deterioration at final observation and consecutive decreases in MD value during the observation period, as well as clinical characteristics and IOP-related factors, were analyzed.
Results
Of 134 eyes in 134 NTG patients meeting all eligibility criteria, significant MD slope deterioration was observed in 80 eyes (59.7%). MD slope deterioration was significantly associated with consecutive decreases in MD values (Cochran–Armitage trend test: P=0.0000; univariate logistic regression analysis: P<0.0001). While no significant relationship was observed between central corneal thickness, refractive error, or prevalence of disc hemorrhage, consecutive decreases in MD value was significantly related to MD slope deterioration (univariate logistic regression analysis: P<0.0001). A reduction of IOP during the follow-up period was significantly related to nondeterioration of the MD slope (multivariate logistic regression analysis: P=0.0020).
Conclusion
In this 6-year observation of NTG patients treated with medical therapy, the occurrence of three or more consecutive decreases in MD value was significantly associated with visual field deterioration. Reduction in IOP was postulated to be contributing in the prevention of VFD progression.
Introduction
Standard automated perimetry is typically employed for the assessment of glaucomatous visual field defects (VFD), as it provides a quantitative, objective assessment of the severity and progression of VFD.Citation1 In order to manage glaucoma effectively, it is critical to detect the progression of VFD in its earliest stages; however, this strategy requires frequent repeat testing of visual fields.Citation2,Citation3 We have previously reported that three or more consecutive decreases in mean deviation (MD) could be an indicator of the early progression of VFD detected at the final observation in patients with primary open-angle glaucoma (POAG) and normal tension glaucoma (NTG).Citation4
Reductions in intraocular pressure (IOP) may prevent visual field deterioration.Citation4 While decrease in IOP has been effective in preventing VFD progression in POAG eyes,Citation5–Citation7 a few studies have reported its contribution to preventing long-term VFD progression in NTG eyes.Citation8–Citation11 Accordingly, we focused on NTG patients who had been treated with medical therapy and followed for at least 6 years and analyzed the relationship between MD slope at final observation and consecutive decreases in MD values over time. We also assessed several factors that may affect VFD progression, such as disc hemorrhage (DH),Citation12 refractive error,Citation9 and central corneal thickness (CCT),Citation13 which were not investigated in our previous report.
Patients and methods
Study design
This was a retrospective study.
Patients
This study was conducted in compliance with the Declaration of Helsinki and Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan. All participants provided written informed consent for data collection at the time of their initial visit. Prior to the present study, we gave the opportunity to participants to opt out of the study.
From April 2006 through March 2016, data were collected from 311 POAG and NTG patients undergoing treatment with topical glaucoma medications. Patients who had undergone routine ophthalmologic examinations during the follow-up period, including measurement of IOP and visual fields, were included in the study. Eligible patients fulfilled all of the following criteria: 1) diagnosis of NTG at baseline; 2) age 20 years or older at the start of the follow-up period; 3) measurement of baseline IOP by Goldmann applanation tonometry before the start of treatment; 4) testing of visual fields with a Humphrey field analyzer (Zeiss-Humphrey, San Leandro, CA, USA) without alteration of the strategy (Swedish Interactive Threshold Algorithms standard) or C 24-2 program; 5) accurately measurable IOP (excluding those with history of keratorefractive surgery, ocular injury, and keratoconus); 6) no history or complication of apparent retinal disease; and 7) MD greater than −20 decibels (dB) during visual field testing at the start of the follow-up period.
As parameters of VFD progression, MD slope deterioration and consecutive decreases in MD value were calculated using data from reliable visual field tests for more than 6 years (≥10 times at 6-month intervals) meeting the following two criteria: 1) fixation losses <33%; and 2) false-positive or false-negative <33%. Patients with a history of glaucoma surgery with a corrected visual acuity of <0.7 were excluded. This study involved a single eye per patient. If both eyes satisfied all criteria, the eye with a lower MD value was included. There were no restrictions on the type or number of topical glaucoma medications used, and patients of both sexes were enrolled. Ultimately, 134 eyes of 134 patients met all eligibility criteria.
The study protocol was approved by the Institutional Review Board of Kyoyukai RiverSide Clinic in Sapporo, Japan. This study was registered to UMIN (ID: UMIN000022334) in advance of data collection.
Investigations
MD values and MD slope were calculated with the use of HfaFiles Version 5.0 software (Beeline, Tokyo, Japan). As previously reported, “deterioration of MD slope” was defined if the MD slope showed significantly (P<0.05) negative value calculated by the least-square method at the final visual field test.Citation4 “Deterioration of MD value” was defined as a decrease in the MD value by more than 0.05 dB between two consecutive tests. “Consecutive deterioration” was defined as a successive decrease in MD values between follow-up visits. Similarly, “triple deterioration” and “quadruple deterioration” were defined as three or four consecutive decreases in MD value, respectively. The largest number of consecutive decreases was used for analysis.
In advance of initiation of treatment, IOP was measured four or more times, and baseline IOP was defined as the mean value of all IOP values excluding the first IOP measurement value. For the purposes of this study, “mean IOP” was defined as the mean of all IOP values measured every 3 months during the follow-up period. IOP fluctuation was calculated as the standard deviation (SD) of the mean follow-up IOP, and the maximum and minimum IOP during the follow-up period were also determined. The difference between baseline IOP and mean IOP was defined as ΔIOP, and the IOP reduction rate was determined by calculating ΔIOP as a percentage of baseline IOP. DH was assessed by ophthalmoscopy (Kowa, Nagoya, Japan) at each visit, and fundus photography (Kowa) was performed every 6 months. CCT was measured with Cirrus HD-OCT 400 Version 5.1 (Zeiss-Humphrey).
Statistical analysis
Patients’ identifying information was concealed before data entry. The Cochran–Armitage trend test and logistic regression analysis were performed to analyze the relationship between MD slope and consecutive decreases in MD value.
Clinical characteristics (such as prevalence of DH) and IOP-related factors were compared between the two groups – patients with deterioration of MD slope and those without deterioration – using the Welch’s t-test, Fisher’s exact test, or the Wilcoxon rank-sum test depending on the scale of the data. The relationship between various factors and the deterioration of MD slope were evaluated with multivariate logistic regression analysis using the presence or absence of MD slope deterioration as the objective variable and the consecutive decrease of MD values or the IOP reduction rate versus baseline as explanatory variables.
Analyses were performed with EZR Version 1.32 software (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which provides a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). The level of significance was set at 5% (two-sided). All analyses were inspected by Satista Co. Ltd. (https://www.satista.jp/medical/).
Results
Of 622 eyes of 311 POAG and NTG patients, 134 eyes from 134 NTG patients fulfilled all eligibility criteria, consisting of 82 female and 52 male patients with a mean ± SD age of 57.7±11.3 years (range, 28–80 years; all results are given as mean ± SD [range] unless otherwise indicated). The follow-up period was 8.05±0.82 years (6–12 years). Baseline IOP was 14.96±1.98 mmHg (10.7–20.0 mmHg); refractive error was −3.19±3.56 diopters (D) (−13.3 to +6.8 D); and CCT was 520.5±32.7 μm (440–606 μm). The initial MD value was −7.46±5.53 dB (−19.11 to +1.15 dB), and the final MD value was −10.35±6.49 dB (−26.39 to +0.26 dB) ().
Table 1 Patient characteristics, IOP data, and visual field data
During the observation period, a consecutive decrease in MD values was observed in 97% of the eyes (130/134). Among these, a triple or quadruple consecutive decrease in MD values was observed in 54.5% of eyes (73/134) (). We found significant deterioration of MD slope at the final observation in 59.7% of eyes (80/134); the mean change in MD slope was −0.22±0.22 dB/yr (). A consecutive decrease in MD values was significantly correlated with deterioration of MD slope, both by trend analysis (P=0.0000) and univariate logistic regression analysis (odds ratio: 2.19; 95% confidence interval [CI]: 1.44–3.34; P<0.0001) ().
Figure 1 Distribution of number of eyes in which consecutive decrease in MD value was observed.
Abbreviation: MD, mean deviation.
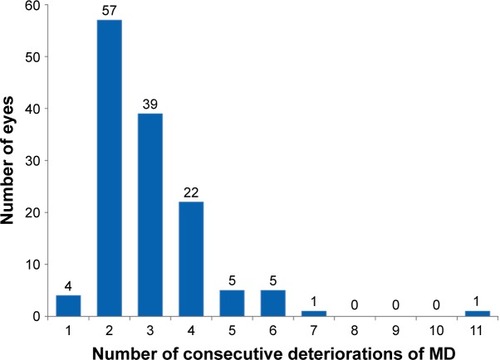
Figure 2 Distribution of number of eyes with MD slope value at the final visual field test.
Abbreviation: MD, mean deviation.
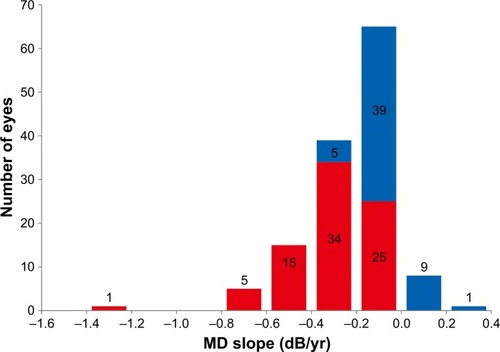
Table 2 Results of trend analysis and univariate logistic regression analysis
Mean IOP during the observation period was 12.01±0.88 mmHg (8.8–15.0 mmHg), and mean IOP fluctuation was 0.97±0.22 mmHg (0.6–2.0 mmHg). The IOP reduction rate relative to baseline was 18.82%±8.48% (−0.3% to 35.9%). DH was observed in 21.6% of eyes (29/134).
No significant differences in clinical characteristics were evident between groups with or without MD slope deterioration. Although there was no significant difference in initial and observation period MD values between the two groups, MD slope was significantly steeper in the MD slope deterioration group than in the nondeterioration group (−0.32 dB/yr versus −0.06 dB/yr; P<0.0001).
There were no significant differences in the prevalence of DH, degree of refractive error, and CCT between the two groups. However, the IOP reduction rate was significantly greater in the nondeterioration group than in the MD slope deterioration group (P=0.0053) (). Multivariate analysis revealed that the number of consecutive decreases in MD value was significantly associated with deterioration of the MD slope (odds ratio: 2.43; 95% CI: 1.55–3.80; P<0.0001), while IOP reduction rate was significantly associated with nondeterioration of MD slope (odds ratio: 0.92; 95% CI: 0.88–0.97; P=0.0020) ().
Table 3 Comparison of variables between groups with and without MD slope deterioration
Table 4 Results of multivariate logistic regression analysis
Discussion
During the 6-year follow-up period of the present study, the occurrence of three or more consecutive decreases in MD values was significantly related to MD slope deterioration in patients with NTG who were taking topical glaucoma medications. In contrast, reduction of IOP may play a role in the nondeterioration of MD slope.
In a previous study, we reported that three or more consecutive decreases in MD during follow-up is a risk factor for significant deterioration of MD slope in patients with POAG and NTG, and that eyes with MD slope nondeterioration had significantly higher rates of reduction in IOP.Citation4 However, our previous study included POAG patients in whom a decrease of abnormally elevated IOP is likely to prevent VFD progression; in contrast, IOP levels are within the normal range in NTG patients. In the present study, we examined a variety of factors that may affect VFD progression in patients with NTG.
Significant deterioration of the MD slope occurred in 59.3% of patients with NTG. Previous long-term observational studies of NTG have indicated that progression of VFD occurs in approximately 50% of patients (46.3%–53%).Citation8,Citation10,Citation14 Progression of NTG can also be assessed by morphological changes.Citation15 However, trend analysis and calculation of the MD slope are generally employed for assessment of VFD, since the definition of progression according to morphological data has not been fully established. According to a definition of VFD deterioration as MD slope exceeding 0.5 dB/yr, Komori et alCitation10 reported a frequency of VFD progression of 53%. In the present study, incidence of VFD progression was 59%, which was slightly higher than previous reports.Citation8–Citation11 We defined VFD progression as a significant decrease in MD slope determined by regression analysis; mean MD slope value was −0.32 dB/yr. Even in normal individuals, MD values decline by 0.06–0.08 dB/yr with increasing age.Citation16 VFD progression criteria in the present study, therefore, were considered appropriate for NTG patients under long-term observation. Trend analysis and the odds ratio of univariate logistic regression analysis for consecutive decreases of MD versus deterioration of MD slope was 2.26, indicating that the deterioration of the MD slope was significantly related to consecutive decrease in MD values. Thus, consecutive decreases in MD values predict subsequent worsening of VFD in NTG patients, and suggest the necessity of additional treatment.
DH,Citation8,Citation10 myopia,Citation9 and CCTCitation17 are documented risk factors for VFD progression in NTG. However, some studies have shown these factors to be unrelated to VFD progression.Citation14,Citation18–Citation20 In our current study, no apparent difference was observed among these factors when compared between groups (eyes with deterioration of MD slope and those with nondeterioration). The multiple disparate pathologies of NTG may be responsible for varying results among different studies.
Factors related to IOP, in contrast, have shown consistent relationships to the progression of VFD in most previous reports. However, there are differences among IOP-related factors, ie, peak IOP,Citation14 changes in IOP,Citation21 or the IOP reduction rate,Citation8 and their degree of influence over VFD progression. In our study, only IOP reduction rate was significantly greater in patients without MD slope deterioration than in those with deterioration.
Long-term studies of NTG have reported baseline IOPs of 15–16 mmHg and mean IOPs during the observation period of 13–14 mmHg.Citation8–Citation10,Citation14 In the present study, baseline IOP was not significantly different between the MD slope deterioration group and the nondeterioration group (14.7 mmHg versus 15.4 mmHg), but the rates of IOP reduction during the observation period were significantly different between groups. However, the numerical difference in rates was not large −17.2% IOP reduction rate in the MD slope deterioration group and 21.5% in the nondeterioration group – suggesting that other factors may need to be considered. Accordingly, we conducted multivariate logistic regression analysis to statistically examine the relationships among variables that were significant according to univariate analysis. Since this was a retrospective observational study, we calculated the odds ratio rather than the risk ratio. Our results demonstrated that progression of VFD was related to the number of consecutive decreases in MD value, while the IOP reduction rate was related to nondeterioration of VFD.
We also investigated predictions of future VFD deterioration in NTG patients with the naïve Bayes method.Citation22 Assuming that consecutive decreases in MD values and reduction of IOP occur independently, 10,000 simulations were conducted, and a classification rule (deterioration/nondeterioration) was prepared. From this, the concordance rate was 69.8% and its 95% CI was 69.6%–70.0%. Effective methods for predicting the progression of glaucomatous VFD have not yet been established. For example, the concordance rate of ophthalmologists for predicting progression of VFD is nearly 60%.Citation23 Therefore, the present simulation was supportive of consecutive decreases in MD values and IOP reduction rate as prognostic factors for VFD progression in NTG patients.
Conclusion
In the present study population, a 20% reduction of IOP from baseline may slow the progression of VFD, a result that emphasizes the importance of controlling IOP in patients with NTG.
Acknowledgments
This was an investigator–industry collaborative study, funded by Santen Pharmaceutical Co., Ltd. (Osaka, Japan). Santen Pharmaceutical Co. Ltd. participated in the design of the study, suggestions of the statistical method, interpretation of the data, and preparation and review of the manuscript, but had no role in the collection and analysis of data.
Disclosure
Santo K, Hizaki H, and Hashimoto M are employees of Santen Pharmaceutical Co., Ltd. The authors report no other conflicts of interest in this work.
References
- HeijlALindgrenGOlssonJA package for the statistical analysis of visual fieldsDoc Ophthalmol Proc Ser198749153168
- ChauhanBCGarway-HeathDFGoñiFJPractical recommendations for measuring rates of visual field change in glaucomaBr J Ophthalmol200892456957318211935
- CrabbDPGarway-HeathDFIntervals between visual field tests when monitoring the glaucomatous patient: wait-and-see approachInvest Ophthalmol Vis Sci20125362770277622427597
- NaitoTYoshikawaKMizoueSRelationship between consecutive deterioration of mean deviation value and progression of visual field defect in open-angle glaucomaClin Ophthalmol201592217222226648689
- ChandlerPALong-term results in glaucoma therapyAm J Ophthalmol196049222124613809130
- GrantWMBurkeJFJrWhy do some people go blind from glaucoma?Ophthalmology19828999919987177577
- BrubakerRFDelayed functional loss in glaucoma. LII Edward Jackson Memorial LectureAm J Ophthalmol199612154734838610790
- KimMKimDMParkKHKimTWJeoungJWKimSHIntraocular pressure reduction with topical medications and progression of normal-tension glaucoma: a 12-year mean follow-up studyActa Ophthalmol2013914e270e27523406253
- SakataRAiharaMMurataHContributing factors for progression of visual field loss in normal-tension glaucoma patients with medical treatmentJ Glaucoma201322325025423059475
- KomoriSIshidaKYamamotoTResults of long-term monitoring of normal-tension glaucoma patients receiving medical therapy: results of an 18-year follow-upGraefes Arch Clin Exp Ophthalmol2014252121963197025128961
- LeeJKongMKimJKeeCComparison of visual field progression between relatively low and high intraocular pressure groups in normal tension glaucoma patientsJ Glaucoma201423855356023751927
- KitazawaYShiratoSYamamotoTOptic disc hemorrhage in low-tension glaucomaOphthalmology19869368538573737131
- ViswanathanDGoldbergIGrahamSLRelationship of change in central corneal thickness to visual field progression in eyes with glaucomaGraefes Arch Clin Exp Ophthalmol201325161593159923494444
- ErdemEWilliamsAKucharSDWaisbourdMSpaethGLLong-term (>8 years) evaluation of progression in patients with low-pressure glaucomaEur J Ophthalmol201525649049525982210
- BanegasSAAntónAMorillaAEvaluation of the retinal nerve fiber layer thickness, the mean deviation, and the visual field index in progressive glaucomaJ Glaucoma2016253e229e23526020689
- SuzumuraHYoshikawaKMizoueSHyodoRKimuraTAssessment of retinal sensitivity using a time-saving strategy in normal individualsClin Ophthalmol201261873187823185115
- GordonMOBeiserJABrandtJDThe Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucomaArch Ophthalmol2002120671472012049575
- MitchellPHourihanFSandbachJWangJJThe relationship between glaucoma and myopia: the Blue Mountains Eye StudyOphthalmology1999106102010201510519600
- MedeirosFASamplePAZangwillLMBowdCAiharaMWeinrebRNCorneal thickness as a risk factor for visual field loss in patients with preperimetric glaucomatous optic neuropathyAm J Ophthalmol2003136580581314597030
- SohnSWSongJSKeeCInfluence of the extent of myopia on the progression of normal-tension glaucomaAm J Ophthalmol2010149583183820231010
- FukuchiTYoshinoTSawadaHThe relationship between the mean deviation slope and follow-up intraocular pressure in open-angle glaucoma patientsJ Glaucoma201322968969723722866
- YagerRRAn extension of the naive Bayesian classifierInf Sci20061765577588
- LinAPKatzLJSpaethGLAgreement of visual field interpretation among glaucoma specialists and comprehensive ophthalmologists: comparison of time and methodsBr J Ophthalmol201195682883120956271
