Abstract
Purpose
Four cases of corneal ectasia after small-incision lenticule extraction (SMILE) have been reported. In this review, we provide an overview of the published literature on corneal ectasia after SMILE and risk factors associated with this complication.
Methods
Case reports were identified by a search of seven electronic databases for pertinent heading terms between 2011 and July 2017. We identified patient characteristics and surgical details including preoperative topography, central corneal thickness, and anterior keratometry (Km). Residual stromal bed (RSB) values not reported were computed using VisuMax ReLEx SMILE software Version 2.10.10. Preoperative ectasia risk was measured using the Randleman Ectasia Risk Score System (ERSS). Percent tissue alteration was calculated for each patient as described by Santhiago et al.
Results
Seven eyes of four patients developed corneal ectasia post SMILE. Two patients had abnormal topography in both eyes. One patient had abnormal topography in one eye. Only one patient was noted to have normal topography in both eyes and later developed ectasia in one eye in the absence of any known risk factors. The mean Randleman ectasia risk score was 4±3 (range: 1–8). The mean calculated percent tissue altered (PTA) was 38%±6% (range: 30%–47%).
Conclusion
A majority of reported ectasia cases occurred in patients with subclinical keratoconus. These conditions may be exacerbated by SMILE and should be considered absolute contraindications to the procedure. Three patients were identified to have high risk based on the ERSS, and one patient exhibited a PTA ≥40%. We formulated a modification to the current calculation of PTA that takes into account the differences in tissue altered between SMILE and laser in situ keratomileusis (LASIK). More studies are needed to fully quantify the risk of ectasia. For now, we propose adopting the same exclusion criteria used for LASIK in the SMILE procedure until more specific metrics have been validated.
Introduction
After the US Food and Drug Administration (FDA) approval of laser in situ keratomileusis (LASIK), early laser platform users began reporting incidents of keratectasia.Citation1,Citation2 It was unclear whether these preliminary instances of ectasia were isolated consequences of a newly developed technology or the first of many cases to come.Citation3 In the following years, the high volume of LASIK procedures performed revealed ectasia to be a persistent, albeit rare, postoperative complication. Detection of ectasia became easier as prognostic markers, such as the Randleman Ectasia Risk Score System (ERSS) and percent tissue altered (PTA), accrued in the literature and surgical predictability increased. To date, the prevalence of ectasia after LASIK has been estimated to be quite low, between 0.04% and 0.6%.Citation4 Nevertheless, the sensitivity of current risk assessment modalities remains disputed due to the highly multifactorial nature of ectasia.Citation5,Citation6
Small-incision lenticule extraction (SMILE) is an alternative to LASIK that has demonstrated less dry eye symptoms, a lack of flap-related complications, and less injury to the subbasal nerve plexus.Citation7–Citation12 With the exception of a small side cut incision through which the refractive lenticule is extracted, SMILE preserves the collagen networks of the anterior stroma that account for ~60% of the total corneal tensile strength.Citation13,Citation14 Even though SMILE is thought to reduce the probability of iatrogenic ectasia compared to LASIK, only four cases have been reported in the literature.Citation15 In this review, we provide a concise summary of these cases and reiterate the importance of a conservative approach to performing SMILE on patients with suspicious topographies.
Methods
A literature review was performed using the following electronic databases: PubMed, Scopus, Ovid Medline, Embase, ScienceDirect, Google Scholar, and Cochrane Library. Publications were drawn between the dates of 2011 and July 2017. Key words used in the search queries included “ectasia” or “keratoconus” and “small incision lenticule extraction” or “SMILE” or “ReLEx SMILE”. There were no language restrictions.
We reviewed patient characteristics information including age, sex, manifest refraction, cylinder, and spherical equivalent. Preoperative information such as topography, central corneal thickness (CCT), and anterior keratometry (Km) was also noted. The preoperative risk of ectasia in reported cases was measured using the Randleman ERSS.
Two of the case reports did not include parameter data such as cap diameter, cap thickness (CT), optical zone, and maximum lenticule thickness (LT).Citation16,Citation17 In addition, three of the four patients did not have residual stromal bed (RSB) values reported. For these specific eyes, maximum LT and PTA were calculated using VisuMax ReLEx SMILE software Version 2.10.10 (Carl Zeiss Meditec AG, Jena, Germany), assuming the conventional parameters for a cap diameter of 7.10 mm, CT of 120 μm, and optical zone of 6.50 mm. RSB values were then calculated using CT and maximum LT subtracted from CCT.
Compliance with ethics guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 1964 Declaration of Helsinki, as revised in 2013.
Results
Seven eyes of four patients who underwent bilateral SMILE for myopia and myopic astigmatism correction were noted to develop ectasia.Citation16–Citation19 The mean refractive error was −3.56±2.11 (range: −1.5 to −6.75 D) with a mean cylinder of −1.12±0.38 (range: −0.5 to −1.25). The mean manifest refraction spherical equivalent (MRSE) was −4.13±2.08 (range: −2.25 to −7.25). Preoperative patient characteristics and lenticule parameters are listed in and , respectively.
Table 1 Patient characteristics
Table 2 Pachymetric analysis of SMILE lenticule and corneal thickness alteration
Cases of post-SMILE ectasia were reported in China, Egypt, Finland, and India. All patients were male with an average age of 26±5 years (range: 19–33 years). None of the patients studied reported a family history of keratoconus. The mean preoperative CCT was 520±29 μm (range: 513–559 μm). All patients had preoperative corrected distance visual acuity (CDVA) of 20/20 or better. The mean reported preoperative anterior Km was 42.28±1.6 (range: 40.4–45.1). The mean calculated RSB was 321±35 (range: 288–389). The mean Randleman Ectasia Risk Score was 4±3 (range: 1–8) with five eyes categorized as being at high risk and three eyes being identified as low risk for ectasia after LASIK. The mean calculated PTA was 38%±6% (range: 30%–47%) with six eyes having a PTA <40% and two eyes having a PTA >40%. Based on proposed PTA safety thresholds, two eyes were recognized to be at high risk for ectasia.
Two patients were diagnosed with subclinical keratoconus in both eyes. One patient was diagnosed with unilateral mild keratoconus (OD) preoperatively and normal topography in the other eye (OS) that progressed to bilateral ectasia.Citation16 The fourth patient had normal topography in both eyes preoperatively, which later progressed to unilateral ectasia (OS).Citation19 Overall, five eyes of the four patients displayed abnormal preoperative topographies but underwent SMILE nevertheless. The diagnosis of postoperative ectasia in these patients was made in an average of 6.4 months (range: 1–12 months) after surgery.
Discussion
SMILE is believed to have less of a biomechanical impact on the integrity of the cornea than LASIK.Citation20,Citation21 Tissue removal in SMILE occurs much deeper than in LASIK, avoiding the interruption of the strong interweaving, steeper angles, and sheer stress of the anterior stroma.Citation22 Specifically, SMILE is thought to result in greater stromal collagen stiffness and less deformations in the RSB when compared to LASIK.Citation23 Although the theoretical risk of ectasia may be reduced, it is not completely eliminated due to the disruption of stroma that follows any refractive surgery.Citation24 In the four cases described, preoperative abnormal topography was noted in three patients with post-SMILE ectasia. Ectasia occurred soon after surgery in these patients. This suggests that SMILE may not be suitable for patients exhibiting subclinical keratoconus, similar to LASIK. One case reported ectasia with normal preoperative topography, signifying that abnormal topography may not be the only risk factor for developing ectasia after SMILE.
An RSB of <300 μm is thought to be a risk factor for ectasia after LASIK.Citation25 Although this principle has been applied to SMILE, practitioners currently do not know what the safety threshold for RSB should be. It has been hypothesized that leaving a thinner RSB may be a viable parameter for achieving higher myopic correction in SMILE. Practitioners who recognize the improved biomechanics of SMILE have proposed extracting a deeper lenticule and leaving a lower safety threshold RSB given the preserved integrity of the stronger anterior stroma.Citation26 For example, an RSB of 220 μm may be attainable with conservative estimations using a CT of 120 μm, comprising a corneal epithelium of 40 μm and an anterior stroma of 80 μm. This would result in a theoretically unaltered stromal tissue of 380 μm, if the tensile strength of 80 μm of anterior stroma is considered equivalent to that of 160 μm of posterior stroma.Citation27 However, this hypothesis may not hold true given that patients in this review developed ectasia despite having an RSB of >300 μm. shows that five eyes had the safety threshold RSB within ±10 μm.
The Randleman ERSS for LASIK incorporates a number of ectasia risk factors that may be relevant to SMILE. For example, the ERSS evaluates CCT, age, myopia, RSB, and topography to measure a patient’s postoperative risk.Citation28–Citation30 Based on the data in , five out of eight ectatic eyes (62.5%) in this review would have been identified as high risk by this system based on abnormal topography alone. Screening with this system would have likely precluded three patients from undergoing LASIK. Thus, the Randleman system may also have a practical use in the routine evaluation of patients before SMILE. Utilizing a calculated PTA, only two out of eight eyes (25%) were classified as high risk. In these patients, the Randleman system was a more sensitive screening metric. Santhiago et alCitation31–Citation33 had previously reported that a PTA >40% was more predictive of ectasia risk than moderate-to-high ERSS values for LASIK patients. Based on the cases reviewed, PTA alone may not be sensitive or specific enough for ectasia risk after SMILE. However, it should be noted that Santhiago et al applied this >40% cutoff to patients presenting with normal topography. In patients with abnormal topography, such as those in this study, they suggested that the safety threshold for PTA in SMILE may be lower than that in LASIK, but no specific cutoff was endorsed.Citation34
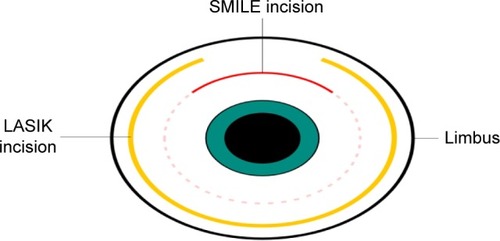
Currently, SanthiagoCitation35 has put forth a revised evaluation of PTA, specific for SMILE, which examines the relationship of the LT, CT, and CCT such that PTA = (CT + LT)/CCT. From a conceptual basis, the amount of tissue altered in SMILE is less compared to that in LASIK. We believe that this notion necessitates the use of a correction factor to the original formula put forth by Santhiago et al. Vertical side cuts through the corneal lamellae are thought to weaken corneal structural integrity more than horizontal delamination incisions during LASIK flap creation.Citation36 If this concept holds true for SMILE, the ratio of vertical incision between these two procedures can be determined. We began by computing the ratio of incision length to total circumference for each procedure as illustrated in . For a LASIK flap diameter of 8.75 mm, a hinge angle of 55°, and a flap circumference of 27.5 mm, the actual LASIK flap incision length would be 23.3 mm. Assuming a SMILE cap diameter of 7.5 mm, small-incision angle of 90°, and cap circumference of 23.6 mm, the small-incision length would be equal to 5.89 mm. The resulting ratio of small-incision length to total SMILE cap circumference (S) would be 0.25. Similarly, the ratio of LASIK flap incision length to total flap circumference (L) would be 0.85. Therefore, the ratio of S/L would be equal to 0.30. This ratio can be interpreted theoretically as SMILE inducing 70% less disruption of anterior corneal lamellae than LASIK for an identical myopic correction.
Figure 1 Schematic representation of SMILE incision and LASIK flap incision with respect to the corneal limbus.
Abbreviations: SMILE, small-incision lenticule extraction; LASIK, laser in situ keratomileusis.
We offer a modified PTA (mPTA) formula that accounts for this difference in anterior corneal lamellae disruption between the two procedures using the ratio discussed earlier. This mPTA should be calculated using the formula, mPTA = [(S/L) × CT + LT]/CCT, and the mean mPTA was found as 22%±6% (range: 15%–32%). Although no safety threshold PTA value for SMILE has been endorsed, we believe that an mPTA value of approximately 20% may be considered as high risk. If we apply this threshold to the patients in this study, five out of eight eyes (62.5%) would have been identified as high risk. This threshold could be used to assess patient ectasia risk for SMILE and may even be lower in patients with abnormal topography. Still, we cannot say for certain that our modified formula will result in a PTA for SMILE that is sensitive or specific. More specific biomechanical data from post-SMILE ectasia cases are needed to fully delineate the association between PTA and the risk for postoperative ectasia.
Conclusion
We have reviewed four cases of postoperative ectasia following SMILE. Ectasia was found to be more common in patients with underlying corneal pathology but was also seen in a patient with normal topography. Thus, ectasia may be a risk inherently associated with the SMILE procedure. If implemented, the Randleman’s criteria would have precluded three patients from undergoing SMILE, whereas PTA alone would have only identified one patient as high risk for ectasia. We propose that SMILE may cause 70% less disruption of the anterior corneal lamellae when compared to LASIK and offer a modified formula for PTA in SMILE. A low threshold for mPTA, approximately 20%, could indicate a high risk for ectasia after SMILE. However, determination of an accurate calculation of PTA must be developed using data from patients who had ectasia after SMILE in the absence of risk factors.
There have been >750,000 cases of SMILE performed worldwide, and only four cases of ectasia have been reported. We currently lack the sufficient long-term follow-up evidence needed to thoroughly assess ectasia risk, but we assume that the risk will be similar to, if not less than, post-LASIK ectasia. Further studies should examine the patient characteristics that predispose individuals to develop ectasia after SMILE in the absence of risk factors and compare those to similar patients who developed ectasia following LASIK. Additionally, a thorough review of the screening protocols currently used before SMILE may illuminate areas for improvement using corneal biomechanical and wavefront principles. Until specific risk screening metrics for SMILE have been validated, caution should be exercised in patients with abnormal topography. For now, we recommend the same contraindication criteria for LASIK be adopted to the SMILE procedure.
Data availability
All data generated or analyzed during this study are included in the tables provided in this published review or referenced to the appropriate source.
Acknowledgments
This study was funded by an unrestricted grant from Research to Prevent Blindness (RPB), New York, NY, USA.
Editorial assistance in preparation of this manuscript was provided by Mitchell T Tingey of Brigham Young University, Andrew E Bean of the McGovern Medical School, and Yasmyne C Ronquillo, MD, of HDR Research, Hoopes Vision.
Disclosure
The authors report no conflicts of interest in this work.
References
- SeilerTIatrogenic corneal ectasia after LASIK – is the end in sight?Klin Monbl Augenheilkd2005222542915912462
- RadASJabbarvandMSaifiNProgressive keratectasia after laser in situ keratomileusisJ Refract Surg2004205 supplS718S72215521275
- PallikarisIGKymionisGDAstyrakakisNICorneal ectasia induced by laser in situ keratomileusisJ Cataract Refract Surg200127111796180211709254
- RandlemanJBEvaluating risk factors for ectasia: what is the goal of assessing risk?J Refract Surg201026423623720415319
- RandlemanJBRussellBWardMAThompsonKPStultingRDRisk factors and prognosis for corneal ectasia after LASIKOphthalmology2003110226727512578766
- DuppsWJJrEctasia risk: a multifactorial conundrumJ Cataract Refract Surg201541469970025840291
- MoshirfarMMcCaugheyMVReinsteinDZShahRSantiago-CabanLFenzlCRSmall-incision lenticule extractionJ Cataract Refract Surg201541365266525804585
- IvarsenAAspSHjortdalJSafety and complications of more than 1500 small-incision lenticule extraction proceduresOphthalmology2014121482282824365175
- ReinsteinDZCarpGIArcherTJGobbeMOutcomes of small incision lenticule extraction (SMILE) in low myopiaJ Refract Surg2014301281281825437479
- SekundoWKunertKSBlumMSmall incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective studyBr J Ophthalmol201195333533920601657
- VestergaardAHGrauslundJIvarsenARHjortdalJØEfficacy, safety, predictability, contrast sensitivity, and aberrations after femtosecond laser lenticule extractionJ Cataract Refract Surg201440340341124480564
- BlumMTäubigKGruhnCSekundoWKunertKSFive-year results of small incision lenticule extraction (ReLEx SMILE)Br J Ophthalmol20161009119226746577
- RandlemanJBGrossniklausHEDawsonDGMcCareyBEEdelhauserHFDepth-dependent cohesive tensile strength in human donor corneas: implications for refractive surgeryJ Refract Surg2008241S85S8918269156
- ReinsteinDZArcherTJGobbeMThe Key Characteristics of Corneal Refractive Surgery: Biomechanics, Spherical Aberration, and Corneal Sensitivity After SMILE, in Small Incision Lenticule Extraction (SMILE)Cham, SwitzerlandSpringer2015123142
- YangERobertsCMehtaJA review of corneal biomechanics after LASIK and SMILE and the current methods of corneal biomechanical analysisClin Exp Ophthalmol2016616
- MattilaJSHolopainenJMBilateral ectasia after femtosecond laser-assisted small incision lenticule extraction (SMILE)J Refract Surg201632749750027400083
- El-NaggarMTBilateral ectasia after femtosecond laser–assisted small-incision lenticule extractionJ Cataract Refract Surg201541488488825747164
- WangYCuiCLiZCorneal ectasia 6.5 months after small-incision lenticule extractionJ Cataract Refract Surg20154151100110625953471
- SachdevGSachdevMSSachdevRGuptaHUnilateral corneal ectasia following small-incision lenticule extractionJ Cataract Refract Surg20154192014201826603410
- Sinha RoyADuppsWJJrRobertsCJComparison of biomechanical effects of small-incision lenticule extraction and laser in situ keratomileusis: finite-element analysisJ Cataract Refract Surg201440697198024857440
- WuDWangYZhangLWeiSTangXCorneal biomechanical effects: small-incision lenticule extraction versus femtosecond laser-assisted laser in situ keratomileusisJ Cataract Refract Surg201440695496224751146
- JesterJVWinklerMJesterBENienCChaiDBrownDJEvaluating corneal collagen organization using high-resolution nonlinear optical macroscopyEye Contact Lens201036526026420724856
- SevenIVahdatiAPedersenIBContralateral eye comparison of SMILE and flap-based corneal refractive surgery: computational analysis of biomechanical impactJ Refract Surg201733744445328681903
- KlingSHafeziFCorneal biomechanics – a reviewOphthalmic Physiol Opt201737324025228125860
- BinderPSTrattlerWBEvaluation of a risk factor scoring system for corneal ectasia after LASIK in eyes with normal topographyJ Refract Surg201026424125020166627
- ReinsteinDZArcherTJRandlemanJBMathematical model to compare the relative tensile strength of the cornea after PRK, LASIK, and small incision lenticule extractionJ Refract Surg201329745446023820227
- EuroTimesReasons to SMILE – interview with Dan ReinsteinJacobSEYE ContactEuropean Society of Cataract and Refractive Surgeons (ESCRS)Dublin, Ireland2016
- RandlemanJBWoodwardMLynnMJStultingRDRisk assessment for ectasia after corneal refractive surgeryOphthalmology20081151375017624434
- GiriPAzarDTRisk profiles of ectasia after keratorefractive surgeryCurr Opin Ophthalmol201728433734228594648
- RandlemanJBTrattlerWBStultingRDValidation of the ectasia risk score system for preoperative laser in situ keratomileusis screeningAm J Ophthalmol2008145581381818328998
- SanthiagoMRSmadjaDGomesBFAssociation between the percent tissue altered and post-laser in situ keratomileusis ectasia in eyes with normal preoperative topographyAm J Ophthalmol2014158187.e195.e124727263
- SanthiagoMRGiacominNTSmadjaDBecharaSJEctasia risk factors in refractive surgeryClin Ophthalmol20161071372027143849
- SanthiagoMRSmajdaDWilsonSERandlemanJBRelative contribution of flap thickness and ablation depth to the percentage of tissue altered in ectasia after laser in situ keratomileusisJ Cataract Refract Surg201541112493250026452432
- SanthiagoMRSmadjaDWilsonSEKruegerRRMonteiroMLRandlemanJBRole of percent tissue altered on ectasia after LASIK in eyes with suspicious topographyJ Refract Surg201531425826525884581
- SanthiagoMRPercent tissue altered and corneal ectasiaCurr Opin Ophthalmol201627431131527096376
- Knox CartwrightNETyrerJRJaycockPDMarshallJEffects of variation in depth and side cut angulations in LASIK and thin-flap LASIK using a femtosecond laser: a biomechanical studyJ Refract Surg201228641942522692524
