Abstract
Purpose
We report a case of a sympathetic ophthalmia that occurred after 23-gauge transconjunctival sutureless vitrectomy for a retinal detachment.
Case report
A 41-year-old Japanese woman underwent combined phacoemulsification with intraocular lens implantation and 23-gauge transconjunctival sutureless vitrectomy for a rhegmatogenous retinal detachment in the right eye. Endolaser photocoagulation and silicone oil tamponade were used to manage inferior retinal holes. Four weeks after the surgery, she returned with a 5-day history of reduced vision and metamorphopsia in her left eye. Slit-lamp examination showed a shallow anterior chamber in the right eye and moderate anterior uveitis bilaterally. Silicone oil bubbles and pigment dispersion were observed in the subconjunctival space adjacent to the right eye’s superonasal sclerotomy site. Fundus examination showed multifocal serous retinal detachments in both eyes. A diagnosis of sympathetic ophthalmia was made and the patient was treated with intensive topical and systemic steroids. The subretinal fluid cleared in both eyes following treatment. Twelve months after the onset of inflammation, the patient’s condition was stable on a combination of oral cyclosporine and topical steroids. Sunset glow retinal changes remain, but there has been no evidence of recurrent inflammation.
Conclusion
Sympathetic ophthalmia can develop after 23-gauge transconjunctival sutureless vitrectomy despite its smaller sclerotomy size. We recommend that special care should be taken to inspect for adequate closure of sclerotomy sites at the end of this operation.
Introduction
Sympathetic ophthalmia, a bilateral granulomatous panuveitis, is a rare condition that can occur after a penetrating eye injury or intraocular surgery.Citation1 Although the risk of sympathetic ophthalmia following conventional 20-gauge vitrectomy has previously been suggested,Citation2,Citation3 there is only one reported case of sympathetic ophthalmia following transconjunctival sutureless vitrectomy (23- or 25-gauge).Citation4 We present a further case that confirms that there is a risk of developing sympathetic ophthalmia after transconjunctival sutureless vitrectomy despite its smaller sclerotomy size.
Case report
A 41-year-old Japanese woman presented with blurred vision in her right eye. Her best-corrected visual acuity was 0.3 in the right eye and 1.0 in the left eye, and the corresponding intraocular pressures were 16 mmHg and 17 mmHg. Anterior segment slit-lamp examination showed tobacco dust in the anterior vitreous cavity of the right eye. Fundus examination revealed a right, flat, inferior, macula-off retinal detachment. Several retinal holes within regions of equatorial lattice degeneration were observed in the area of the detached retina, which formed fibrous strands in the subretinal space. The patient had no history of ocular trauma or surgery. Examination of the left eye showed nothing out of the ordinary.
The patient underwent combined phacoemulsification with intraocular lens implantation and 23-gauge transconjunctival sutureless vitrectomy under local anesthesia. Endolaser and silicone oil tamponade were used to treat the inferior retinal holes. Postoperatively she developed a massive hyphema and hypotony and underwent surgical irrigation and aspiration of the hyphema 14 days after the initial surgery.
Four weeks after the initial surgery, the patient returned with a 5-day history of reduced vision and metamorphopsia in her left eye. Her best-corrected visual acuity was 0.03 in the right eye and 0.15 in the left eye, and the corresponding intraocular pressures were 7 mmHg and 16 mmHg. Slit-lamp examination showed a shallow anterior chamber in the right eye with a moderate anterior uveitis bilaterally. Silicone oil bubbles and pigment dispersion were observed in the subconjunctival space adjacent to the right eye’s superonasal sclerotomy site. Fundus examination revealed multifocal serous retinal detachments in both eyes (), which were confirmed by optical coherence tomography (). Optical coherence tomography also showed a membranous reflex in the subretinal space of the left eye that suggests the presence of an inflammatory product such as fibrin (). Fluorescein angiography of the left eye showed multiple points of dye leakage at the level of the retinal pigment epithelium during the early phase and multilobular dye pooling during the late phase (). An audiogram revealed mild hearing loss at higher frequency ranges. Examination of the cerebrospinal fluid revealed a mild pleocytosis. Human leukocyte antigen (HLA) typing showed HLA-A24, HLA-B54, HLA-B61, and HLA-DR4. An association with HLA-DR4 has previously been reported among Japanese patients with Vogt-Koyanagi-Harada disease and sympathetic ophthalmia.Citation5
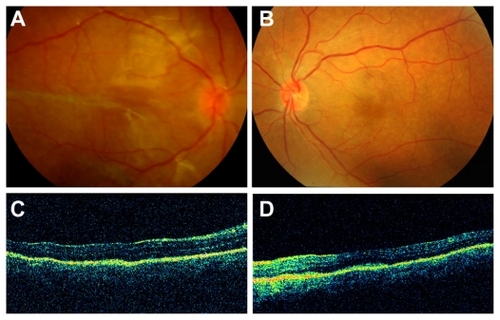
Figure 1 Images obtained after the onset of sympathetic ophthalmia. Fundus photograph of the right (A) and left eye (B); optical coherence tomography images of the right (C) and left eye (D) fundi; early-phase (E) and late-phase (F) fluorescein angiography of the left eye.
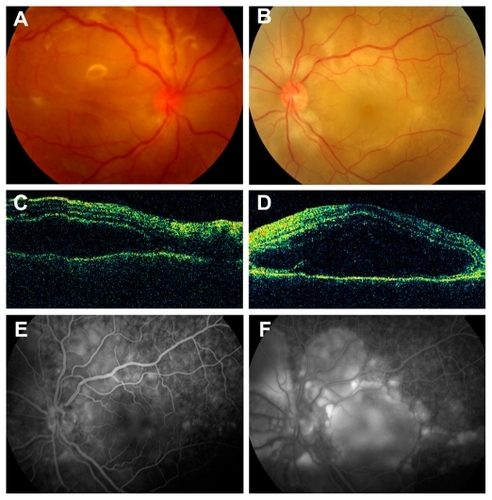
A diagnosis of sympathetic ophthalmia was made, and the patient was treated with two cycles of pulsed-steroid therapy (1 g of intravenous methylprednisolone for 3 days, followed by 40 mg of oral prednisone) in addition to intensive topical steroids (0.1% betamethasone). The subretinal fluid cleared in both eyes following treatment (); however, the hypotony and shallow anterior chamber in the right eye failed to resolve. The dose of oral prednisone was gradually reduced and eventually replaced by oral cyclosporine treatment. Currently, 12 months after the onset of inflammation, she is managed with oral cyclosporine (150 mg daily) and topical 0.1% betamethasone. The stigma of sunset glow fundal changes remains present, but there has been no evidence of recurrent inflammation. Her best-corrected visual acuity is 0.1 in the right eye and 1.2 in the left eye, and the corresponding intraocular pressures are 7 mmHg and 17 mmHg.
Discussion
A prospective population-based study in the United Kingdom and Republic of Ireland demonstrated that ocular surgery, particularly retinal surgery, has a greater risk of sympathetic ophthalmia than that of accidental trauma.Citation6,Citation7 The incidence of sympathetic ophthalmia reported in their population was 0.03/100,000; developing in 0.125% of patients following vitrectomy, and in 0.074% of patients following external retinal detachment surgery.Citation6,Citation7
Recent advancements in microsurgical techniques have led to increased adoption of transconjunctival sutureless vitrectomy using 23- or the smaller 25-gauge microinstruments.Citation8,Citation9 These vitrectomy systems permit the use of smaller wounds, which theoretically results in less postoperative inflammation. However, there is also a growing concern that transconjunctival sutureless vitrectomy may be associated with an increased incidence of wound leak and subsequent ocular hypotony.Citation10
Our case emphasizes that there is a risk of sympathetic ophthalmia in patients who undergo transconjunctival sutureless vitrectomy, particularly when this technique is performed with inadequate closure of the sclerotomy sites. Although the exact mechanism of developing sympathetic ophthalmia is not clear and is most likely multifactorial, lack of wound closure leads to a disturbed blood–retinal barrier and exposes ocular antigens, which may contribute to the development of sympathetic ophthalmia. Another possibility is that a massive hyphema with hypotony complicated the postoperative course, which may have led to wound disruption and uveal prolapse. With the rapid increase in popularity for the use of transconjunctival sutureless vitrectomy and expanding indications we may expect to see this complication more frequently over the coming years, especially in patients with specific genetic predispositions and risk factors. We recommend that special care should always be taken to check for wound leakage at the end of this surgery and when using sutures at the sclerotomy sites when self-sealing wounds are not achieved.
Disclosure
The authors report no conflicts of interest in this work.
References
- CastiblancoCAdelmanRSympathetic ophthalmiaGraefes Arch Clin Exp Ophthalmol2009247328930218795315
- GassJSympathetic ophthalmia following vitrectomyAm J Ophthalmol19829355525587081353
- CroxattoJGalentinePCupplesHHarperDReaderAZimmermanLSympathetic ophthalmia after pars plana vitrectomy-lensectomy for endogenous bacterial endophthalmitisAm J Ophthalmol19819133423466782885
- ChaDWooSAhnJParkKA case of sympathetic ophthalmia presenting with extraocular symptoms and conjunctival pigmentation after repeated 23-gauge vitrectomyOcul Immunol Inflamm201018426526720662657
- OhnoSImmunogenetic and molecular genetic studies on ocular diseasesNippon Ganka Gakkai Zasshi19929612155815791362479
- KilmartinDDickAForresterJProspective surveillance of sympathetic ophthalmia in the UK and Republic of IrelandBr J Ophthalmol200084325926310684834
- KilmartinDDickAForresterJSympathetic ophthalmia risk following vitrectomy: should we counsel patients?Br J Ophthalmol200084544844910781505
- FujiiGde JuanEJHumayunMInitial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgeryOphthalmology2002109101814182012359600
- EckardtCTransconjunctival sutureless 23-gauge vitrectomyRetina200525220821115689813
- SpirnMComparison of 25, 23 and 20-gauge vitrectomyCurr Opin Ophthalmol200920319519919390437