Abstract
This review of orbital fractures has three goals: 1) to understand the clinically relevant orbital anatomy with regard to periorbital trauma and orbital fractures, 2) to explain how to assess and examine a patient after periorbital trauma, and 3) to understand the medical and surgical management of orbital fractures. The article aims to summarize the evaluation and management of commonly encountered orbital fractures from the ophthalmologic perspective and to provide an overview for all practicing ophthalmologists and ophthalmologists in training.
Introduction
Blunt trauma to the orbital rim is a frequent cause of both orbital fractures and damage to the surrounding facial bones and soft tissues. Many surgical specialties, including ophthalmologists, otolaryngologists, maxillofacial specialists, neurosurgeons, and plastic surgeons, evaluate and treat orbital fractures.Citation1 A wide range of treating physicians means that varying levels of expertise and experience are involved in the care of patients with periorbital trauma. The goal of this review is to summarize the evaluation and management of commonly encountered orbital fractures from the ophthalmologic perspective by focusing on the common fractures encountered by ophthalmologists and dividing them into three main categories: 1) orbital floor, 2) medial wall, and 3) zygomatic.
Relevant anatomy
Orbital floor
The adult orbital floor comprises the maxillary, zygomatic, and palatine bones. It is the shortest of all the walls, measuring 35–40 mm. The floor terminates at the posterior edge of the maxillary sinus. The orbital floor lies in close proximity to the inferior rectus muscle, which can have pathologic involvement in an adjacent fracture (). The infraorbital groove, canal, and foramen are contiguous and tunnel through the maxilla, encasing the maxillary branch of the trigeminal nerve. This branch exits the foramen as the infraorbital nerve, providing sensory innervations to the ipsilateral floor and middle of the face. The infraorbital artery, a tributary of the maxillary artery, and the infraorbital vein are also found within the infraorbital groove exiting the infraorbital canal. Infraorbital nerve dysfunction occurs and is often the only complaint following pure orbital floor fracture. This sensory disturbance traditionally has not been an indication for repair.
Medial wall
The medial wall comprises the frontal process of the maxilla, the lacrimal bone, the orbital plate of the ethmoid bone, and the sphenoid body. The area damaged most easily by trauma is the very thin lamina papyracea (0.2–0.4 mm thick), which separates the orbit from the ethmoidal sinuses. The lacrimal sac lies anteriorly along the medial wall in the lacrimal groove formed by the maxilla and lacrimal bone.
At the junction of the medial wall and orbital roof are the anterior and posterior ethmoidal foramina. Through these foramina, the anterior and posterior ethmoidal arteries and nerves course between the orbit and the anterior cranial fossa. These structures can be injured directly at the time of trauma, and the surgeon must be aware of their location during repair in order to avoid intraoperative bleeding.
Also of anatomic importance is the medial rectus muscle, which is intimately related to the medial wall. One of the most obvious signs of medial wall fracture is a motility disturbance, usually deficient adduction or abduction, caused by damage to or entrapment of the medial rectus (). Other significant, medially located structures that must be accounted for in medial wall trauma include the medial canthal tendon, trochlea, and lacrimal drainage system.
Zygomatic
The zygomatic bone occupies a prominent and important position in the facial skeleton. The zygoma forms a significant portion of the floor and lateral wall of the orbit and forms a portion of the zygomatic arch, otherwise known as the malar eminence. It plays a key role in the determination of facial morphology, namely in maintaining normal facial width and prominence of the cheek.
Sicher and DeBrul and, later, Manson et al describe facial anatomy in terms of structural pillars or buttresses.Citation2,Citation3 These buttresses help give the zygoma an intrinsic strength so that blows to the cheek usually result in fractures of the zygomatic complex at the suture lines and not of the zygomatic bone itself.
Branches of the fifth and seventh cranial nerves lie within the bounds of the middle of the face. During surgical repair of zygomatic fractures, the temporal and zygomatic branches of the seventh nerve and the zygomaticotemporal and zygomaticofacial branches of the fifth nerve must be avoided in order to prevent complications of paresis and paresthesias, respectively.
Muscle attachments along the zygomatic arch include the origin of the masseter, the zygomaticus major, and some fibers of the temporalis fascia. It is vital to limit subperiosteal dissection during repair in order to maintain the bony connections of the muscles of facial animation. Whitnall’s tubercle, which serves a critical role in the maintenance of eyelid contour as the attachment site for the lateral canthal tendon, is located on the zygomatic bone, 2 mm behind the lateral orbital rim.Citation4
Evaluation
History
The physician must first determine the mechanism of facial trauma. A history of the eye being struck by an object larger than the diameter of the orbital rim is commonly associated with a “blowout” fracture. This can involve the medial wall, but the orbital floor is involved more commonly. The cause of this type of fracture is thought to be from increased intraorbital pressure, which causes the orbital bones to break at their weakest point. Another theory is that compression of the inferior orbital rim causes direct buckling of the orbital floor. A history of trauma such as a fist blow directly to the naso-orbital region is commonly offered by patients with isolated medial wall fractures. A mechanism of injury that involves a blow to the side of the face from a fist, from an object, or secondary to a motor vehicle accident can be associated with zygomatic trauma. However, each fracture type can present from a variety of mechanisms.
Physical examination
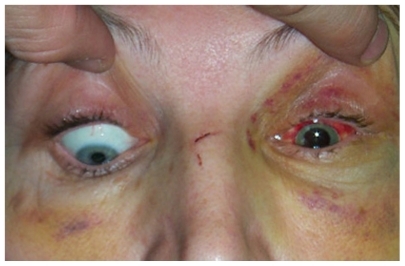
The primary step in assessing a patient after a trauma, especially for those patients involved in multisystem trauma, requires evaluation of airway, breathing, and circulatory status. Also, a full evaluation of the globe must be performed. Patients with periorbital trauma frequently present with traumatic pathology of the globe that can threaten visual outcome, especially if not identified in a prudent manner. Patients with orbital fractures can present with traumatic irits, corneal abrasion, hyphema, acute glaucoma, lens trauma, vitreous hemorrhage, commotio retinae, retinal tears and detachment, and traumatic optic neuropathy.Citation5 Decreased visual acuity, color vision, and, most importantly, an afferent papillary defect can alert the physician to the presence of traumatic optic neuropathy. Careful evaluation for possible globe rupture must be performed. The majority of pathologies can be present even in visually asymptomatic patients.Citation6 Treatment of any vision-threatening conditions should almost always preclude repair of the fracture until stable.
In addition to the common fracture types described as follows, one must remember that less common fractures, eg, to the orbital roof, can be present singly or in conjunction with other fractures. Orbital roof fractures can necessitate early neurosurgical consultation if complications such as pneumocephalus, hematoma, or cerebrospinal fluid (CSF) leaks are present.
Once these steps have been taken, the ophthalmologist can move on to the other specific findings seen in orbital fractures.
Orbital floor
After an orbital floor fracture, external examination may reveal only periorbital edema and ecchymosis. If the orbital rim is involved in the fracture, the patient may demonstrate a palpable bony “step-off ” and complain of pain with palpation of the rim. Ipsilateral injury to the infraorbital nerve can cause hypesthesia, dysesthesia, or hyperalgesia. Hertel exophthalmometry may demonstrate either proptosis or enophthalmos and should be documented. Unusually severe orbital edema may be associated with more severe fractures and can cause proptosis. Once the edema has subsided (usually 1–2 weeks), enophthalmos may be present. However, one must consider proptosis from retrobulbar or peribulbar hemorrhage as well; if present and severe, it can be vision threatening.
Limited vertical movement may be due to entrapment of the inferior rectus or the perimuscular fascia into the fracture site (). In the case of possible entrapment, one must assess for the signs of the oculocardiac reflex: bradycardia, nausea, and syncope.Citation7 Also, a subclass of orbital fracture with entrapment is the so-called “trapdoor” fracture in children.Citation8 These fractures show minimal bony displacement and can present with an external examination that appears to be relatively benign. Children may be more prone to pure trapdoor fractures than adults, and incarceration of the muscle in such fractures can lead to permanent damage of the neuromuscular complex. In addition to entrapment, limitation of extraocular muscle motility due to orbital edema or traumatic palsy of the third nerve branch to the inferior rectus may cause decreased extraocular movements. If a question exists, forced duction testing may help to clarify the etiology.
Medial wall
Isolated medial wall fractures frequently remain undetected. Clinical findings suggestive of a medial wall fracture, in addition to periorbital edema and ecchymosis, and subconjunctival hemorrhage (all nonspecific) include subcutaneous emphysema due to damage to the ethmoidal air cells, epistaxis, and CSF rhinorrhea. Entrapment of the medial rectus muscle can be seen. Pseudo-Duane’s retraction syndrome or retraction of the globe and narrowing of the palpebral fissure on attempted abduction may occur with medial wall fracture associated with medial rectus entrapment, and it is pathognomonic for this complication.
It is important to be alert for CSF rhinorrhea because it represents injury to the meninges and thus is an indication for prophylactic broad-spectrum antibiotics and neurosurgical consultation.
Medial wall fractures with ethmoid–orbital fractures can cause damage to the nasolacrimal drainage system and the medial canthal ligament. In some of these fractures, the medial canthal tendon is injured, resulting in traumatic telecanthus.
Zygomatic
External examination can reveal significant malar depression with step defects at the infraorbital rim, frontozygomatic suture, and zygomatic buttress of the maxilla intraorally. Fractures of the zygomatic bone evoke pain on palpation in 70% of patients. Paresthesias in the distribution of the infraorbital, zygomaticofacial, or zygomaticotemporal nerves can be seen.
Posterior displacement of the fracture fragment may disrupt movement of the mandible, causing difficulty with mastication. Inferior displacement of the lateral canthal angle may indicate inferior migration of the fractured zygomatic bone.
Although these are not true orbital blowout fractures, entrapment of orbital contents, enophthalmos, and diplopia with restriction of motility may occur because of the contributions of the zygomatic bone to the orbital floor. Use of the Hertel exophthalmometer in the assessment of relative enophthalmos or proptosis may be unreliable or impossible because the lateral orbital rim, which is displaced in most zygomatic complex fractures, serves as a reference point for this instrument. One can also use the Naugle exophthalmometer in these cases, which uses the frontal bone as a reference.
Imaging
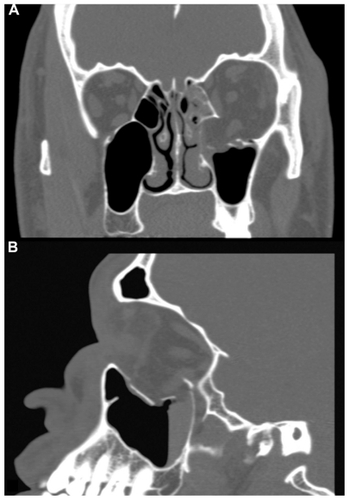
For most orbital fractures, the imaging study of choice is the computed tomography (CT) scan. A CT scan with axial and coronal views is optimal. Imaging should be done with thin cuts (2–3 mm), paying specific attention to the orbital floor and optic canal. When the patient has severe head and neck trauma, the radiologist may have difficulty positioning the patient to obtain coronal views. Because these views are generally the most helpful for evaluating the integrity of the orbital floor, very thin axial cuts should be obtained to allow reconstructed coronal views to be created.
The CT scan offers distinct advantages over other imaging modalities.Citation9 The size and morphology of the fracture can be determined, which aids in not only clinical assessment but also surgical planning. A CT scan can determine whether the fracture involves the optic canal. A CT scan can also reliably demonstrate whether acute proptosis in a patient is secondary to orbital hemorrhage, a potential vision-threatening emergency, or orbital emphysema. A CT scan can also help detect entrapment of the rectus muscles, recognized by displacement of the muscle into the fracture site, with or without bone displacement.
Management
Treatment
Medical
Patients should be advised to avoid blowing their nose for several weeks after the injury to prevent orbital emphysema and possible visual compromise. Nasal decongestant sprays are often used. Many physicians also use prophylactic antibiotics to prevent possible orbital cellulitis from bacterial spread if a fracture creates a direct orbital communication with the sinuses. When orbital edema is severe, steroids may be used to decrease orbital edema, whether or not surgery is indicated.
Surgical
The criteria for surgical intervention in blowout fractures of the medial and, more commonly, inferior orbital wall are controversial and often debated. Currently, three general guidelines are commonly agreed on for surgical intervention.Citation10
Diplopia due to limitation of motility with a positive forced duction test and radiologic confirmation of an orbital fracture suggests entrapment of the rectus muscle or the perimuscular tissues. If diplopia is still present days after trauma, repair is indicated. Diplopia may be present initially after trauma but may resolve as the orbital edema or hemorrhage subsides. In a “white-eye” or “trapdoor” fracture in children, several studies have demonstrated more complete resolution of diplopia if these cases are operated on very early or as soon as the diagnosis is made. Careful examination of the CT scan is essential, because there is often no loss of the floor and a lack of blood in the maxillary sinus. For “non-trapdoor” types, many clinicians believe that if diplopia is present 10–14 days after trauma, then it will not resolve without intervention.
Enophthalmos that is greater than 2 mm 14 days after trauma and cosmetically significant to the patient can be an indication for surgery. Orbital edema that is present initially may mask any enophthalmos. Therefore, exophtalmometry must be rechecked once the orbital edema has subsided. This usually occurs between 10 days and 2 weeks after injury.
A fracture involving one half or more of the orbital floor, especially when associated with a medial wall defect, usually leads to a cosmetic and/or functional deformity. If left unattended, these fractures tend to result in significant enophthalmos; therefore, the size of the fracture in these cases can be an indication for repair.
One must remember, however, that these guidelines must be treated as such. The clinician must always take into account the clinical scenario and the patient’s condition and wishes.
When surgery is indicated, many believe that it is usually best performed as close to 2 weeks from the trauma date as possible. This allows the swelling to subside and a more accurate examination of the orbit to be performed. Additionally, the scarring usually has not advanced enough to prohibit adequate surgical correction. However, there are many clinicians within ophthalmology and elsewhere who feel that earlier or even later intervention should be employed when possible.Citation11
Surgical technique
Although much of the surgical care of orbital fractures is beyond the scope of this article, a brief description of surgical technique follows. Surgical approach to the orbital floor varies. It can be accessed through a conjunctival approach, through cutaneous exposure, or through a transantral approach. Of note, endoscopic approaches via a transmaxillary and transnasal route have been described.Citation12–Citation16 Despite being described more than a decade ago, these endoscopic approaches have yet to find widespread acceptance. Proponents of the endoscopic approach point to several advantages of traditional approaches when used in the right setting. Primarily, enhanced visualization and avoidance of adverse affects to the eyelid are mentioned.
Once access is achieved, this allows for exploration and release of displaced or entrapped soft tissue. This will hopefully alleviate any motility disturbances due to entrapment. In addition, repair of the bony defect with removal or repositioning of bony fragments allows for restoration of the partition between the orbit and maxillary sinus, thereby restoring orbital volume. Several types of implants are used to assist in reconstructing orbital anatomy. The ideal implant should be easy to insert and manipulate, inert, not prone to infection or extrusion, easily anchored to surrounding structures, and reasonably priced. It should not rouse fibrous tissue formation. Most orbital floor defects can be repaired with synthetic implants composed of porous polyethylene, silicone, metallic rigid miniplates, Vicryl mesh, resorbable materials, or metallic mesh. Autogenous bone from the maxillary wall or the calvaria can be used, as can nasal septum or conchal cartilage.
For medial fractures, numerous surgical approaches have also been used to explore the medial orbital wall and to repair its fractures. The appropriate approach depends on both the extent of the fracture and its association with other fractures. In the past, the traditional approach used to repair medial wall fractures was the Lynch incision. The Lynch incision provides excellent exposure, but it can result in severe scarring or webbing of the medial canthal skin. More recently, the transcaruncular approach has become a major approach to the medial orbit, as it avoids leaving a visible scar.Citation17,Citation18 As with floor fractures, most repairs involve returning the prolapsed soft tissue into the orbit, reconstructing the broken fragments, and then possibly reinforcing the medial wall with similar numerous implant materials, as mentioned previously.
Some considerations for zygomatic complex fractures not involving the orbital floor or medial wall should also be noted. The literature indicates that 10%–50% of all zygomaticomaxillary complex fractures require no surgical intervention. This is suitable for fractures that are non-displaced or minimally displaced. If surgery is indicated, a more aggressive approach using open reduction techniques and rigid stabilization with plating systems (eg, Synthes or Leibinger) is the standard of care today, particularly for unstable or potentially unstable fractures.Citation19 Lateral orbital wall fractures are almost never seen in isolation and are usually part of a zygomatic complex fracture. They are treated in conjunction with the zygomatic fracture.
Complications
Any orbital surgery carries with it the potential for complications. Citation20 Failure to diagnose fractures that require early treatment may result in intra-operative or postoperative complications due to fibrosis, contracture, and unsatisfactory union. Other postoperative complications may include loss of vision, traumatic optic neuropathy, diplopia, overcorrection or undercorrection of enophthalmos, lower eyelid retraction, bleeding, infection, extrusion of an orbital implant, infraorbital nerve damage with resultant hypoesthesia, orbital congestion, and epiphora. A complete eye examination is needed postoperatively to adequately assess for the sequelae of these complications.
Most complications are the result of either malpositioning the implant or using the wrong size implant. The most common complication, persistent or surgically induced diplopia, can create significant postoperative morbidity for patients. This diplopia is, however, frequently transient or, if present, only persists in extreme gaze and does not require intervention.Citation21 Transient weakness of the rectus muscle may occur after release of the entrapped muscle, resulting in persistent diplopia, but normally it does improve, sometimes up to a few months later. In cases that do require intervention, the addition of prisms to the patient’s spectacles can offer a nonsurgical treatment. However, occasionally, surgical repositioning of the extraocular muscles is required.
Persistent postoperative enopthalmos creates another challenge for the clinician. The cause of this complication is usually inadequate orbital volume restoration during the primary procedure, although orbital fat atrophy can play a role.Citation21 Surgical repositioning of the implant, or placement of additional implant material, can be needed if the enophthalmos is significant.
Disclosure
The authors report no conflicts of interest in this work.
References
- LelliGMiliteJMaherEOrbital floor fractures: evaluation, indications, approach and pearls from an ophthalmologist’s perspectiveFacial Plast Surg200723319019917691067
- SicherHDeBrulELOral Anatomy5th edSt. LouisMosby197078
- MansonPNMarkowitzBMirvisSToward CT-based facial fracture treatmentPlast Reconstr Surg1990852202212 discussion 213–2142300626
- ZinggMLaedrachKChenJClassification and treatment of zygomatic fractures: a review of 1,025 casesJ Oral Maxillofac Surg19925087787901634968
- CookTOcular and periocular injuries from orbital fracturesJ Am Coll Surg2002195683183412495316
- MellemaPADewanMALeeMSSmithSDHarrisonARIncidence of ocular injury in visually asymptomatic orbital fracturesOphthal Plast Reconstr Surg2009254306308
- SiresBSStanleyRBJrLevineLMOculocardiac reflex caused by orbital floor trapdoor fracture: an indication for urgent repairArch Ophthalmol19981169559569682717
- BansagiZCMeyerDRInternal orbital fractures in the pediatric age group: characterization and managementOphthalmology2000107582983610811070
- NgPChuCYoungNSooMImaging of orbital floor fracturesAustralas Radiol19964032642688826732
- American Academy of OphthalmologySection 7: Orbit, eyelids, and lacrimal systemBasic and Clinical Science CourseSan FranciscoAmerican Academy of Ophthalmology2008101106
- Dal CantoAJLinbergJVComparison of orbital fracture repair performed within 14 days versus 15 to 29 days after traumaOphthal Plast Reconstr Surg2008246437443
- CheongECChenCTChenYREndoscopic management of orbital floor fracturesFacial Plast Surg200925181619206023
- PhamAMStrongEBEndoscopic management of facial fracturesCurr Opin Otolaryngol Head Neck Surg200614423424116832179
- FarwellDGStrongEBEndoscopic repair of orbital floor fracturesOtolaryngol Clin North Am200740231932817383511
- StrongEBKimKKDiazRCEndoscopic approach to orbital blowout fracture repairOtolaryngol Head Neck Surg2004131568369515523449
- MikiTWadaJHaraokaJInabaIEndoscopic transmaxillary reduction and balloon technique for blowout fractures of the orbital floorMinim Invasive Neurosurg200447635936415674754
- GrahamSMThomasRDCarterKDThe transcaruncular approach to the medial orbital wallLaryngoscope2002112698698912160296
- KimSHelen LewMChungSHRepair of medial orbital wall fracture: transcaruncular approachOrbit20052411915764109
- SmythAGA modified miniplate for use in malar complex fracturesBr J Oral Maxillofac Surg19953331691707654662
- SmithBGroveAGuiborPFractures of the orbitDuane’s Clinical Ophthalmology2 Philadelphia, PALippincott-Raven1994
- ColePKaufmanYHollierLPrinciples of facial trauma: orbital fracture managementJ Craniofac Surg200920110110419165002