Abstract
Purpose
To assess the outcome of cataract surgery with hydrophilic acrylic intraocular lens (IOL) implantation in children with congenital and developmental cataracts.
Method
A retrospective review of medical records of children with congenital or developmental cataracts who underwent cataract surgery with hydrophilic IOL implantation, from January 2011 to December 2014 in a tertiary eye hospital in Nepal. Primary posterior capsulotomy, anterior vitrectomy, and IOL implantation was done in children 8 years or younger, while older children underwent only lens aspiration and IOL implantation.
Results
A total of 178 eyes of 120 children underwent cataract surgery with primary IOL implantation. Mean age at the time of surgery was 6.9 years (range: 3 months to 15 years). Average follow-up time was 13.7 (±5.9) months. Associated ocular anomalies were present in 84 (47.1%) eyes. Postoperative complications were found in 33 eyes (18.13%) with inflammatory membrane being the most common (10.1%). Two eyes (1.1%) developed endophthalmitis. Second intervention was needed in 12 (6.5%) eyes. Preoperative vision of less than 6/60 was present in 105 eyes (57.69%). Final best corrected visual acuity of 6/12 or better was found in 81 (44.5%) eyes.
Conclusion
Our study shows that hydrophilic IOL is suitable for use in children. Results of this study are comparable with other studies on pediatric cataract surgeries using hydrophobic acrylic intraocular lenses. Low cost hydrophilic lens implantation is an effective approach in managing pediatric cataract surgery in developing countries like Nepal.
Keywords:
Introduction
Pediatric cataracts is one of the leading causes of childhood visual impairment and blindness in developing countries.Citation1 Surgery in children is different compared to their adult counterparts in many ways. To have a good pediatric cataract surgery setup in the developing world is challenging. It needs a skilled surgeon, a very good setup of equipment, good anesthesia, and nursing care. There are many controversies in pediatric cataract management regarding timing of surgery, intraocular lens (IOL) power calculation, and the choice of IOL.Citation2,Citation3 The choice of IOL mainly depends upon factors like material biocompatibility, posterior capsule opacification, size of wound, and the cost of IOL, especially in developing countries like Nepal. Many studies have shown good outcome, both in the older practice of using rigid poly(methyl methacrylate) (PMMA) lenses and the newer hydrophobic lenses in children with cataracts.Citation4–Citation7 However, there is only a handful of studies showing the outcome of hydrophilic lenses in the pediatric age group.Citation8,Citation9 This study describes the outcome of pediatric cataract surgery with hydrophilic IOL implantation in Nepalese children.
Method
This study is a retrospective review of charts of all the children with congenital and developmental cataracts who underwent surgery in Tilganga Institute of Ophthalmology between January 2011 to December 2014. Children with traumatic cataract, complicated cataracts, and secondary IOL implantations were excluded. The study was approved by the Institutional Review Board of Tilganga Institute of Ophthalmology and it adheres to the tenets of the Declaration of Helsinki. Informed consent was obtained from parents of the children included in the study. All the information was collected from the charts including demographics, laterality of cataract, presenting symptoms, associated ocular abnormalities, preoperative and final best corrected visual acuity, postoperative complications, second surgery, and the follow-up time. Visual acuity in children up to 3 years was determined by the central, steady and maintained fixation method. In children 3–6 years old, visual acuity was determined by E chart at 3 m distance with matching optotype and in older children by the Snellen’s acuity chart. Anterior segment examination was done either by the handheld slit lamp (Kowa, Japan) or the operating microscope. Posterior segment examination was done by indirect ophthalmoscope (Heine Optotechnik, Germany) or B scan ultrasound in dense media opacity.
IOL
IOL power calculation was done in all children under general anesthesia by handheld keratometer (Nidek, Aichi, Japan) and A scan (Alcon Laboratories, Inc., Fort Worth, TX, USA). The type of IOL used was poly(2-hydroxyethyl methacrylate) material (poly-hema) with ultraviolet absorber produced in Fred Hollows intraocular lens lab, Tilganga Institute of Ophthalmology. The IOL power was reduced by 20% in children aged 2 years and younger and 10% in children 2–8 years of age.
Surgical technique
The pupils were dilated with a combination of 1% tropicamide and 10% phenylephrine. All the children underwent surgery under general anesthesia. The two ports were made in limbus in 2 and 10 o’ clock position to enter the anterior chamber by using a microvitroretinal blade. The entire surgery was done by an automated vitrectomy machine (Alcon Accurus). Anterior capsule vitrectorhexis and the lens aspiration was done using a 20 gauge ocutome (Alcon Accurus). The 10 o’ clock wound was enlarged with 3.4 mm keratome. IOL implantation was done using an injector. In cases where vitrectomy was indicated, primary posterior vitrectorhexis and anterior vitrectomy were performed done through the same limbal ports using bimanual ocutome and going underneath the IOL. Wound was closed using 8-0 Vicryl sutures. Primary posterior vitrectorhexis and anterior vitrectomy were performed in children 8 years or younger, older children with nystagmus, mental retardation, or those not cooperative enough for the subsequent Yag capsulotomy. Other children underwent only lens aspiration and IOL implantation.
Results
A total of 178 eyes of 120 children were included in the study. Mean age was 6.9 (±3.6 SD). There were eight children below the age of 2 years and four children below 6 months. Male to female ratio was 1.4. On presentation, nystagmus was present in 17.9% and strabismus in 12.3% of eyes. shows demographics and clinical characteristics of children. Of 178 eyes, only lens aspiration and IOL implantation was done in 75 (42%) eyes whereas in 103 (58%) eyes lens aspiration and anterior vitrectomy with IOL implantation were carried out. Mean follow-up time was 13.7 (±5.9) months. Postoperative complications were present in 18.3% of operated eyes (). The most common complication was inflammatory membrane (10%) followed by visual axis opacification (7%). Two eyes developed endophthalmitis. Twelve (6.4%) eyes required second intervention. Out of two eyes with endophthalmitis, one was treated with intravitreal injection, the other needed core vitrectomy (). Preoperative best corrected visual acuity and the final visual acuity at last follow-up was recorded. In 46 (25%) eyes visual acuity was measured by fixation preference method. compares the pre- and postoperative visual acuity in the children. Visual acuity improved from mean logMAR of 1.5 (±0.6) before surgery to 0.3 (±0.2) at the final follow-up. Preoperative vision of less than 6/60 was present in 105 eyes (57.69%). Final best corrected visual acuity of 6/12 or better was found in 81 (44.5%) eyes. shows diagrammatic representation of pre- and postoperative vision compared in these children.
Figure 1 Pre- and postoperative vision compared.
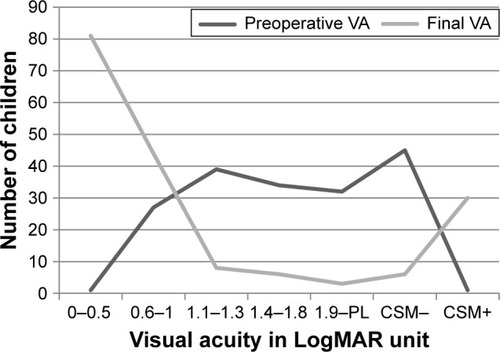
Table 1 Demographics and clinical characteristics of children
Table 2 Postoperative complications
Table 3 Second interventions
Table 4 Pre- and postoperative vision
Discussion
IOL design and biocompatibility plays an important role in visual and surgical outcomes in pediatric cataract.Citation10 Foldable acrylic hydrophobic lenses have been the IOL of choice for many years with good results.Citation11 The rigid gas permeable PMMA lens has also been used by many surgeons, especially in developing countries.Citation12–Citation15 The most important reason being the cost and easy availability. There are studies on the use of PMMA lenses in pediatric cataract surgeries with postoperative outcomes comparable with the foldable acrylic lenses.Citation16 When using PMMA lenses, the wound size needs to be large. So there is chance of induced astigmatism. The use of hydrophilic lenses in the adult population has been reported by many studies, with mixed outcomes.Citation17,Citation18 However, there are very few studies on the use of hydrophilic lenses in a pediatric population. Most of these studies have shown good surgical and visual outcomes in the pediatric population. The Fred Hollows intraocular lens lab has been producing lenses in Tilganga Institute for the last 20 years. However, use of foldable lenses in children has been in practice only recently. It is cheap and easily available for the pediatric population.
Most of the children in our population were in the age group of 2 to 8 years. This indicates late presentation of cataract. The other reason being our practice of only using IOLs around the age of 18 months in bilateral cases. In unilateral cases, we use IOLs at a younger age. Almost 18% of eyes had nystagmus and 10% had already developed strabismus at the time of presentation, also indicating the late presentation of cataract. The follow-up time in our population was shorter than the study done by Kleinmann et al.Citation9 They had a mean follow-up of 47 months. Postoperative complications were found in 18.5% of operated eyes, which is comparable with other similar studies. The rate of visual axis opacification in our study was lower than in the studies done by Kleinmann et al using hydrophilic lenses and Vasavada et al using hydrophobic acrylic lenses.Citation9,Citation19 Contrary to the study done by Kleinmann et al, we have excluded traumatic cataracts. There were 12 children (6.4%) who needed second intervention. shows the rate of posterior capsule opacification in studies using hydrophobic lenses compared to our study. Most of the postoperative inflammatory membrane were resolved with frequent prednisolone acetate eye drops. Five of these children received oral corticosteroids. Endophthalmitis is one of the rare complications after pediatric cataract surgery.Citation20,Citation21 Two eyes developed endophthalmitis in our study. Both of these children had poor medication compliance and were living in poor hygienic conditions.
Table 5 Posterior capsule opacification in studies using hydrophobic lenses compared to our study
Visual outcomes in our study were similar to the studies done by Kleinmann et al.Citation9 We achieved more than 6/12 vision in 47% eyes. Out of 45 eyes with poor fixation, 30 achieved central, steady, and maintained fixation postoperatively. This result is comparable with Kleinmann et al and Panahi-Bazaz et al’s work.Citation9,Citation10
In conclusion, our study shows that foldable hydrophilic lenses are safe to use in children. Visual and surgical outcomes were comparable with other studies using hydrophobic lenses. A prospective comparative study with hydrophobic acrylic lenses may be considered for future study to reach a conclusion. Managing pediatric cataracts in a low resource setting is challenging. The cost of a hydrophilic lens is US$15–US$20 each, while the cost of a hydrophobic lens is US$100–US$150 each. We locally produce hydrophilic lenses in our IOL lab. Hence, hydrophilic lenses are a cheap, easy, and effective approach to managing pediatric cataract surgeries in developing countries like Nepal.
Acknowledgments
This paper was presented at the 43rd annual meeting of American Association of Pediatric Ophthalmology and Strabismus, Vancouver, Canada as an e poster presentation. The poster’s abstract was published in “e Posters” Journal of American Association of Pediatric Ophthalmology and Strabismus (JAAPOS), August 2016, volume 20, issue 4.
Disclosure
The authors report no conflicts of interest in this work.
References
- FosterAGilbertCRahiJEpidemiology of cataract in childhood: a global perspectiveJ Cataract Refract Surg199723Suppl 16016049278811
- LloydICAshworthJBiswasSAbadiRVAdvances in the management of congenital and infantile cataractEye (Lond)200721101301130917914433
- VasavadaARNihalaniBRPediatric cataract surgeryCurr Opin Ophthalmol2006171546116436925
- TrivediRHWilsonMEJrSingle-piece acrylic intraocular lens implantation in childrenJ Cataract Refract Surg20032991738174314522293
- NihalaniBRVasavadaARSingle-piece AcrySof intraocular lens implantation in children with congenital and developmental cataractJ Cataract Refract Surg20063291527153416931267
- RoweNABiswasSLloydICPrimary IOL implantation in children: a risk analysis of foldable acrylic v PMMA lensesBr J Ophthalmol200488448148515031160
- AasuriMKFernandesMPathanPPComparison of acrylic and polymethyl methacrylate lenses in a pediatric populationIndian J Ophthalmol200654210510916770027
- Panahi-BazazMRZamaniMAbazarBHydrophilic acrylic versus PMMA intraocular lens implantation in pediatric cataract surgeryJ Ophthalmic Vis Res20094420120723198075
- KleinmannGZauggBAppleDJBleikJPediatric cataract surgery with hydrophilic acrylic intraocular lensJ AAPOS201317436737023928003
- WilsonMEElliottLJohnsonBPeterseimMMRahSWernerLPandeySKAcrySof acrylic intraocular lens implantation in children: clinical indications of biocompatibilityJ AAPOS20015637738011753259
- TuncerSGucukogluAGozumNCataract extraction and primary hydrophobic acrylic intraocular lens implantation in infantsJ AAPOS20059325025615956945
- RainaUKMehtaDKMongaSAroraRFunctional outcomes of acrylic intraocular lenses in pediatric cataract surgeryJ Cataract Refract Surg20043051082109115130647
- HennigASchroederBGilbertCBilateral pediatric cataract surgery: outcomes of 390 children from Nepal and Northern IndiaJ Pediatr Ophthalmol Strabismus201350531231923565713
- WilsonMEHennigATrivediRHThomasBJSinghSKClinical characteristics and early postoperative outcomes of pediatric cataract surgery with IOL implantation from Lahan, NepalJ Pediatr Ophthalmol Strabismus201148528629120873695
- ThakurJReddyHWilsonMEJrPediatric cataract surgery in NepalJ Cataract Refract Surg20043081629163515313283
- KüchleMLausenBGusek-SchneiderGCResults and complications of hydrophobic acrylic vs PMMA posterior chamber lenses in children under 17 years of ageGraefes Arch Clin Exp Ophthalmol2003241863764112883914
- KugelbergMWejdeGJayaramHZetterströmCTwo-year follow-up of posterior capsule opacification after implantation of a hydrophilic or hydrophobic acrylic intraocular lensActa Ophthalmol200886553353618081899
- HeatleyCJSpaltonDJKumarAJoseRBoyceJBenderLEComparison of posterior capsule opacification rates between hydrophilic and hydrophobic single-piece acrylic intraocular lensesJ Cataract Refract Surg200531471872415899448
- VasavadaARTrivediRHNathVCVisual axis opacification after AcrySof intraocular lens implantation in childrenJ Cataract Refract Surg20043051073108115130646
- AgarkarADesaiREndophthalmitis after cataract surgery in childrenJ AAPOS2015194e34e35
- SmithJPouloseAOlitskySEEndophthalmitis following pediatric cataract surgery with a good outcomeJ Pediatr Ophthalmol Strabismus200643423924016915904
- RashidRHassanJAfzalFManagement of pediatric cataract with acrylic foldable intraocular lens: our experienceChattagram Maa-O-Shishu Hospital Medical College Journal20131212529
