Abstract
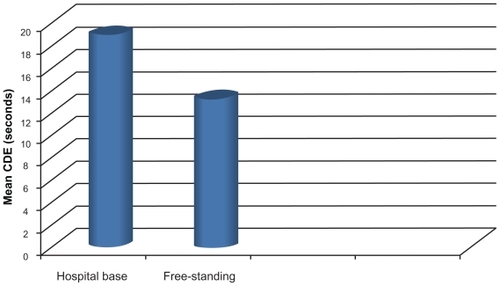
Mean CDE (cumulative dissipated energy) values were compared for an open hospital- based surgical center and a free-standing surgical center. The same model of phacoemulsifier (Alcon Infiniti Ozil) was used. Mean CDE values showed that surgeons (individual private practice) at the free-standing surgical center were more efficient than surgeons (individual private practice) at the open hospital-based surgical center (mean CDE at the hospital-based surgical center 18.96 seconds [SD = 12.51]; mean CDE at the free-standing surgical center 13.2 seconds [SD = 9.5]). CDE can be used to monitor the efficiency of a cataract surgeon and surgical center in phacoemulsification. The CDE value may be used by institutions as one of the indicators for quality control and audit in phacoemulsification.
Introduction
CDE (cumulative dissipated energy) is a built-in device of the Alcon Infiniti phacoemulsification unit (Alcon Labs, Hünenberg, Switzerland). It shows the time taken in seconds to complete a case of phacoemulsification, which reflects how much energy will be expended. Less phacoemulsification time translates to less energy used in the eye, and is considered better for corneal endothelium.Citation1–Citation4 The purpose of this study was to introduce the CDE as a monitor or measure of surgical efficiency in the hope of improving surgical outcomes. CDE data are not currently being widely utilized for this purpose. A higher CDE reading is equated with longer surgical and recovery time, because more energy is dissipated in the eye, resulting in more damage to ocular tissue. Successful phacoemulsification of the cataract with less CDE may correlate with more efficient surgery and better overall outcomes. A previous study used CDE to compare torsional mode with conventional ultrasound mode phacoemulsification.Citation5 Another study utilized the CDE to compare different techniques and settings by different surgeons in phacoemulsification.Citation6
Objective
This study set out to compare mean CDE between surgeons in an open hospital- based surgical center and a free-standing surgical center, using the same model of phacoemulsifier (Alcon Infiniti Ozil). It also intended to establish the mean CDE value in the two institutions as a reference for future training and quality control in cataract surgery.
Method
Ninety cases were retrospectively selected from the records of each institution’s operating room records in one randomly selected month. Because all 180 cases were selected from one randomly selected month of the year and from similar ambulatory settings of the two nearby ambulatory surgical centers with similar descriptive data, the variety of cataract cases (soft vs hard) was expected to be similar. CDE value, taken from the phacoemulsifier, was recorded by the nurse after phacoemulsification. The CDE values of 90 cases from each institution were recorded in an Excel spreadsheet together with age and gender. There is no necessity to record the patient’s identity, which avoids privacy intrusion. The data were then analyzed by SPSS. The ratio of males and females was equal at the hospital and 45.2% versus 54.8% at the surgical center. The age distribution was from 28 to 94 years for the hospital versus 20 to 99 years for the surgical center. This study was approved by the IRB (Institutional Review Board) of the University of Hawaii for ethical issues.
Result
The mean CDE at the hospital-based center was 18.96 seconds (SD = 12.51); for the surgical center it was 13.2 seconds (SD = 9.5) ().
Conclusion
CDE values showed that surgeons at the free-standing ambulatory surgical center were more efficient in phacoemulsification than surgeons at the open hospital-based ambulatory surgical center. The free-standing cataract surgical center may be more efficient in cataract surgery than the open hospital-based ambulatory surgical center.
Discussion
This study intended to use CDE as an objective guide to evaluate the efficiency of phacoemulsification. The open hospital-based ambulatory surgical center has more surgeons (individual private practice) on staff, and each surgeon has a different volume of cataract surgeries. The free-standing cataract surgical center only has four surgeons on staff (individual private practice), and each surgeon has a uniformly large volume of cataract surgeries. Furthermore, the majority of the free-standing surgical center’s cases are cataract surgeries, whereas the hospital-based ambulatory surgical center deals with a variety of different eye cases. Even though the hospital-based ambulatory surgical center is hospital based, it is still an ambulatory center. It is designed for ambulatory care to follow the ambulatory surgery guidelines, as with the free-standing surgical center. Because the cataract surgery was not performed in the main operation room of the hospital but rather in the ambulatory center, cataract cases selected should not be more difficult than those in the free-standing surgical center. Because all 180 cases were selected randomly from one month of the year and from similar ambulatory settings of the two nearby ambulatory surgical centers with similar descriptive data, the variety of cataract cases (soft vs hard) was expected to be similar. This study showed that the high-volume cataract surgeons at the free-standing surgical center had a low mean CDE because of their better efficiency in phacoemulsification. CDE can be used as a monitor for a cataract surgeons’ efficiency in phacoemulsification. A mean CDE value was established for the two institutions in this study. The CDE value may be used by institutions as an indicator of quality control and audit in phacoemulsification.
Disclosure
The authors disclose no conflicts of interest.
References
- PirazzoliBD’EliseoDZiosiMAcciarriREffects of phacoemulcification time on the corneal endothelium using phacofracture and phaco chop techniquesJ Cataract Refract Surg19962279679699041091
- KreislerKRMortensonSWMamalisNEndothelial cell loss following “modern” phacoemulcification by a senior residentOpthalmic Surg1992233158160
- ColvardDMKratzRPMazzoccoTRDavidsonBEndothelial cell loss following phacoemulcification in the pupillary planeAm Intra-Ocular Implant Soc J198174334336
- HayashiKHayashiHHakaoFKayashiFRisk factors for corneal endothelial injury during phacoemulcificationJ Cataract Refract Surg1996228107910848915805
- LiuYZengMLiuXTorsional mode versus conventional ultrasound mode phacoemulcificationJ Cataract Refract Surg200733228729217276271
- ChenMSweeneyHLukeBChenMA retrospective randomized study to compare the energy delivered using CDE with different techniques and OZil® settings by different surgeons in phacoemulcificationClinical Ophthalmology2009340140319688027