Abstract
Background
The purpose of this study was to investigate postoperative clinical outcomes in patients with neovascular glaucoma (NVG) who underwent trabeculectomy or EX-PRESS implantation and to identify predictors of successful EX-PRESS implantation.
Methods
The study designed as a retrospective observational analysis and was set in a single tertiary center. Eighty-nine patients (89 eyes) with NVG, were treated using trabeculectomy alone (Trab group; n=39) or EX-PRESS implantation (EX group; n=50). All patients with a history of glaucoma surgery were excluded. The main outcome measures were postoperative intraocular pressure (IOP), visual acuity (VA), number of medications, complications, additional therapy, and success rate.
Results
The mean follow-up duration was 4.6 months in the Trab group and 4.2 months in the EX group. There was no significant difference in IOP between the groups except at 1-month follow-up (P=0.045). The number of patients with early postoperative hypotony, a shallow anterior chamber, hyphema, or anterior chamber irrigation was significantly lower in the EX group than in the Trab group (P=0.016, 0.008, 0.019, and 0.014, respectively). The other outcomes, ie, VA, number of medications, and success rate, were similar between the two groups. In the EX group, the success rate was significantly lower in 15 patients with a history of vitrectomy compared to that in 35 patients without a history of vitrectomy (P=0.047).
Conclusion
Implantation of an EX-PRESS device may be more effective and safer than trabeculectomy alone in patients with NVG. However, a history of vitrectomy may affect the surgical success rate when using EX-PRESS.
Introduction
Neovascular glaucoma (NVG) is a refractory glaucoma that occurs in several ocular ischemic diseases including diabetic retinopathy, retinal vein occlusion, and carotid artery occlusion, causing severe pain and loss of vision.Citation1 Treatment of NVG aims to improve ocular ischemia and reduce intraocular pressure (IOP) and includes panretinal photocoagulation, injection of an antivascular endothelial growth factor agent, and antiglaucoma medications.Citation2 It is often difficult to reduce medically uncontrollable IOP in NVG eyes, thus necessitating trabeculectomy, implantation of an Ahmed glaucoma valve, or cyclophotocoagulation. However, several surgical complications have been observed.Citation3–Citation5
EX-PRESS (Alcon Laboratories, Inc., Fort Worth, TX, USA) is a small, nonvalved, stainless steel drainage device used as an alternative to standard trabeculectomy in patients with glaucoma.Citation6 The EX-PRESS P-50 model used in this study was 2.6 mm long with a 50 µm internal diameter. Unlike standard trabeculectomy, no iridectomy or sclerectomy is performed in EX-PRESS implantation, which leads to shorter operating time and reduced risk of surgical complications. Previous reports have demonstrated that EX-PRESS implantation achieved better postoperative results and was safer than trabeculectomy alone.Citation6–Citation10 However, subjects in most of the previous studies did not have NVG. Although a few reports showed that EX-PRESS implantation reduced IOP postoperatively in eyes with NVG,Citation11,Citation12 its therapeutic effect in patients with NVG is not fully understood. To the best of our knowledge, there have been no reports comparing the effects of EX-PRESS implantation with those of trabeculectomy alone in patients with NVG.
The aim of this study was to investigate postoperative clinical outcomes in patients with NVG who underwent trabeculectomy or EX-PRESS implantation and to identify predictors of successful EX-PRESS implantation in eyes with NVG.
Methods
Patients
We retrospectively identified 89 patients with NVG who underwent trabeculectomy or EX-PRESS implantation in the Department of Ophthalmology at the Gunma University Graduate School of Medicine, between September 2007 and September 2015. Inclusion criteria were as follows: 1) presence of iris neovascularization diagnosed using slit-lamp examination or gonioscopy, 2) age range from 21 to 90 years, and 3) increased IOP, which could not be controlled by antiglaucoma medication alone. All patients with a history of previous glaucoma surgery were excluded. The patients were divided into two groups based on whether they underwent trabeculectomy alone (Trab group; n=39) or EX-PRESS implantation (EX group; n=50). This study was approved by the institutional review board of Gunma University Hospital (No 2016-058) and conformed to the guidelines under the Declaration of Helsinki. Written informed consent was obtained from all patients for the treatment and retrospective review of their medical records.
Surgical technique
In both groups, a 50% depth square scleral flap, measuring ~2.5×2.5 mm, was created after a fornix-based incision of the conjunctiva. Sponges soaked in mitomycin C (0.4 mg/mL) were applied under the scleral flap and conjunctiva for 3 minutes and irrigated with 200 mL of physiological saline. In the EX group, a P-50 EX-PRESS device was then implanted through the puncture wound using a 25-gauge needle from the limbus toward the anterior chamber. In the Trab group, sclerostomy and peripheral iridectomy were performed. The scleral flap and conjunctiva were sutured with 10-0 nylon in both groups. When cataract surgery was also required, phacoemulsification and aspiration combined with implantation of an intraocular lens were performed after application of mitomycin C to the other wounds. All patients were treated with 1.5% levofloxacin and 0.1% betamethasone for 4–8 weeks after glaucoma surgery. During the early postoperative period, laser suture lysis and needling were performed, depending on postoperative IOP and bleb morphology.
Clinical outcome measures
Postoperative data were obtained on days 1 and 3, at weeks 1 and 2, and at months 1, 3, and 6. IOP was measured using a Goldmann applanation tonometer. Best-corrected visual acuity (BCVA) was recorded as decimal values and converted to logarithm of the minimum angle of resolution (logMAR) for statistical analysis.
Definitions
Success was defined as 5 mmHg ≤ IOP ≤21 mmHg, with or without medications. In this study, need for laser suture lysis or needling was not considered as indication of failure of the procedure. Failure was defined as two consecutive IOP measurements outside the above-mentioned range 2 weeks after glaucoma surgery, the need for further glaucoma surgery including cyclophotocoagulation, or worsening of BCVA to no light perception. Early hypotony was classified as IOP <5 mmHg within 2 weeks after surgery. BCVA in eyes without form vision was defined as counting fingers (0.005), hand motion (0.0025), light perception (0.00125), or no light perception (0.0001), as described previously.Citation13
Statistical analysis
The data were represented as mean ± SD. Two-group comparisons were performed using paired or unpaired t-test. Categorical data were tested for differences using chi-square or Fisher’s exact test. Success of treatment was investigated using Kaplan–Meier survival analysis and log-rank test. P<0.05 was considered to be statistically significant. Statistical analysis was performed using SPSS version 22 (IBM Corporation, Armonk, NY, USA) and GraphPad Prism version 6 (GraphPad Software, Inc., La Jolla, CA, USA).
Results
Preoperative clinical characteristics of the patients are shown in . There were no significant differences in any of the baseline demographics or clinical characteristics between the two groups. All patients were Japanese and exhibited rubeosis iridis in preoperative slit-lamp examination or gonioscopy. The average follow-up duration was 4.6±2.0 months in the Trab group and 4.2±2.0 months in the EX group (P=0.79).
Table 1 Baseline demographic and clinical characteristics of 89 patients with neovascular glaucoma
IOP and visual acuity (VA) outcomes
Preoperative and postoperative IOP values are shown in . IOP values in the Trab group and the EX group were 35.1±8.6 mmHg and 33.4±10.2 mmHg (baseline), 16.4±11.9 mmHg and 15.7±9.5 mmHg (day 1), 10.6±8.3 mmHg and 10.9±6.9 mmHg (day 3), 9.5±7.5 mmHg and 12.6±8.2 mmHg (week 1), 14.4±7.2 mmHg and 15.8±7.6 mmHg (week 2), 18.3±9.2 mmHg and 17.5±7.6 mmHg (month 1), 17.9±9.9 mmHg and 15.8±4.7 mmHg (month 3), and 15.3±5.0 mmHg and 17.8±6.4 mmHg (month 6), respectively. Compared with baseline, both groups showed a statistically significant decrease in IOP at all follow-up time points (P<0.001). The Trab group had a significantly lower mean IOP than the EX group at month 1 (P=0.045). However, no statistically significant difference between the two groups was found at other time points.
Figure 1 Preoperative and postoperative clinical outcomes comparing trabeculectomy alone and EX-PRESS implantation.
Abbreviations: D, day; EX, EX-PRESS implantation; IOP, intraocular pressure; logMAR, logarithm of the minimum angle of resolution; M, month; Trab, trabeculectomy alone; W, week.
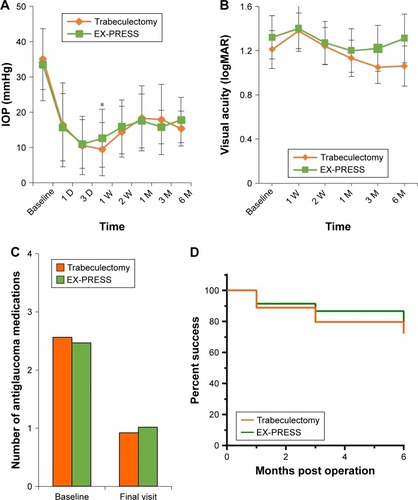
As shown in , the mean BCVA values in the Trab group and the EX group at baseline were 1.15 logMAR and 1.24 logMAR, which changed to 1.03 logMAR and 1.15 logMAR at 3 months, and 1.02 logMAR and 1.24 logMAR at 6 months, respectively. There was no statistically significant difference in VA between the two groups throughout the 6-month follow-up period. One patient in the EX group lost light perception.
Required medications and success rate
At baseline and at the final follow-up visit, the mean number of medications was 2.56±0.90 and 0.92±1.27, respectively, in the Trab group and 2.54±1.36 and 1.06±1.30, respectively, in the EX group. Both groups showed a statistically significant reduction in the number of medications at the final visit compared with that at baseline (P<0.001; ). There were no significant differences in the number of medications between baseline and the final visit in either group (). Kaplan–Meier survival analysis of all patients showed success rates of 72.1% and 78.0% in the Trab group and the EX group, respectively, 6 months after surgery (P=0.51; ).
Complications and additional interventions
Postoperative complications observed are shown in . Early postoperative hypotony was observed in 14 (35.9%) eyes in the Trab group and in seven (14.0%) eyes in the EX group (P=0.016). A shallow anterior chamber was observed in seven (17.9%) eyes in the Trab group and in one (2.0%) eye in the EX group (P=0.019). Hyphema developed in 13 (33.3%) eyes in the Trab group and five (10.0%) eyes in the EX group (P=0.008). Rates of other complications, including choroidal detachment, bleb leak, hypotony maculopathy, and endophthalmitis, were not significantly different between the two groups. No device-related complications were observed in the EX group.
Table 2 Postoperative complications after trabeculectomy alone and after EX-PRESS implantation in patients with neovascular glaucoma
Additional interventions are shown in . Laser suture lysis was performed as needed in 24 (61.5%) eyes in the Trab group and in nine (18.0%) eyes in the EX group (P=0.859). Needling was required in 11 (28.2%) eyes in the Trab group and in seven (14.0%) eyes in the EX group (P=0.116). Postoperative anterior chamber irrigation was performed more often in the Trab group (5/39 eyes) than in the EX group (0/50 eyes; P=0.014). Difference in frequency of repeat glaucoma surgery and cyclophotocoagulation between the two groups was not statistically significant (P=0.579 for both).
Table 3 Additional surgical treatment after trabeculectomy alone and after EX-PRESS implantation in patients with neovascular glaucoma
Surgical risk factors for failure of EX-PRESS implantation
No previous study has investigated surgical risk factors for failure of EX-PRESS implantation in patients with NVG. Factors potentially influencing operative success rates in this study are listed in . We classified the 50 patients who underwent EX-PRESS implantation into the following subgroups: young age (<60 years), previous vitrectomy, preoperative intravitreal bevacizumab, and combined cataract surgery (). Kaplan–Meier survival curves for these subgroups are shown in . A history of vitrectomy was identified as a risk factor for failure of EX-PRESS implantation in patients with NVG (, ; P=0.047). We also found that young age, preoperative intravitreal bevacizumab, and combined cataract surgery were not significant predictors of the surgical outcome (; ; P=0.13, 0.91, and 0.093, respectively).
Figure 2 Kaplan–Meier survival analysis of surgical outcomes in eyes that underwent EX-PRESS implantation for neovascular glaucoma.
Abbreviation: IVB, intravitreal bevacizumab.
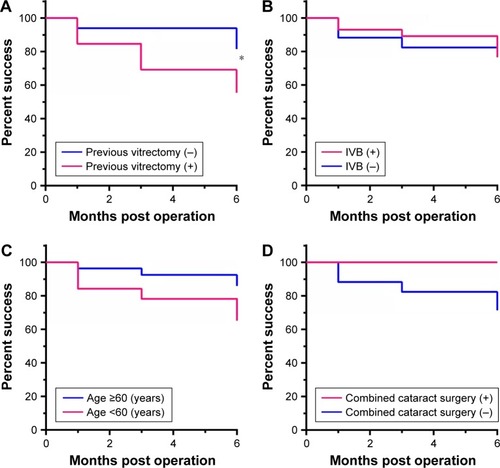
Table 4 Potential predictors of surgical success in patients with neovascular glaucoma who underwent EX-PRESS implantation
Discussion
This study compared postoperative outcomes in patients with NVG who underwent EX-PRESS implantation and those who underwent trabeculectomy. The results showed no statistically significant differences between EX-PRESS insertion and trabeculectomy alone in IOP reduction (except at 1-month follow-up), VA, number of antiglaucoma medications, or success rate. However, EX-PRESS implantation dramatically decreased rates of early postoperative hypotony, shallow anterior chamber, hyphema, and anterior chamber irrigation. In addition, the findings of this study indicated that previous vitrectomy might adversely affect the outcome of EX-PRESS implantation.
Previous studies have reported outcomes of EX-PRESS implantation but have rarely included patients with NVG.Citation6–Citation10 One study showed that EX-PRESS implantation combined with preoperative bevacizumab injection might be effective in patients with NVG; however, that study suffered from the limitations of a small sample size and lack of a control group.Citation11 The EX-PRESS glaucoma filtration device versus trabeculectomy (XVT) study,Citation8 which excluded patients with NVG, compared clinical outcomes of EX-PRESS implantation and trabeculectomy alone and found similar mean IOP, number of medications, and surgical success rates between the two groups. Moreover, the overall surgical complication rate was lower in the EX group than in the Trab group. Considering each surgical complication individually, rates of shallow anterior chamber and hyphema were not significantly different between the two groups in the XVT study. Additionally, a previous study showed that EX-PRESS implantation prevented early postoperative inflammation, compared with trabeculectomy.Citation14 The main complications of trabeculectomy are attributed to overfiltration and bleeding from the iris. In the present study, no patient in the EX group required anterior chamber irrigation because of hyphema; however, five patients (12.8%) in the Trab group required anterior chamber irrigation (P=0.014; ). Eyes with NVG are prone to develop hyphema because the iris in an eye with NVG contains many abnormal vessels, unlike an eye with primary open-angle glaucoma. Iridectomy may be disadvantageous in patients with NVG. Furthermore, early postoperative hypotony and a shallow anterior chamber were observed significantly more frequently in the Trab group than in the EX group because of overfiltration from the scleral wound. A small internal EX-PRESS area appears capable of milder and more stable filtration. The tube versus trabeculectomy (TVT) study reported that Baerveldt glaucoma implant surgery had a higher success rate than trabeculectomy in patients who had undergone previous cataract extraction with implantation of an intraocular lens and/or in patients with uncontrolled glaucoma.Citation15,Citation16 Although Baerveldt glaucoma implant surgery may be suitable for patients with NVG, the operating time required is longer and more advanced operator surgical skills are needed compared with trabeculectomy and EX-PRESS implantation.
An earlier study reported that previous vitrectomy was a risk factor for failure of trabeculectomy with mitomycin C in patients with NVG.Citation3,Citation17 However, a history of vitrectomy had significant influence on operative success rates in the EX group, in this study as well. Four patients with previous vitrectomy in the EX group were defined as surgical failures because of an increase in IOP. This could be explained by the fact that vitrectomy causes diffusion of vasoformative factors, inflammation, and conjunctival scarring, as does standard trabeculectomy.Citation3 Previous studies have reported that intravitreal bevacizumab injection may be effective in patients with NVG.Citation18–Citation20 We injected bevacizumab preoperatively (<1 month) in 26 eyes in the Trab group and in 29 eyes in the EX group. The effect was similar, whether bevacizumab was injected preoperatively or not (P=0.91). In our study, intravitreal bevacizumab was not administered if involutional neovascular vessels were clearly evident in the iris, which might explain why this treatment had no effect on the surgical success rate. Interestingly, in the present study, all patients who underwent EX-PRESS implantation in combination with cataract surgery had a successful surgical outcome (n=12, 100%). Furthermore, a previous study indicated that EX-PRESS implantation combined with phacoemulsification cataract extraction was safe and effective.Citation6 Therefore, at the very least, combined cataract surgery might not have a negative impact on the surgical outcome when EX-PRESS implantation is performed.
The limitations of this study included its short duration of follow-up (6 months), which was because patients with excellent therapeutic effect returned to their family doctor within 12 months of surgery. Long-term operative outcomes were not assessed in this study and need to be addressed in future studies. In summary, we compared postoperative clinical outcomes in NVG after EX-PRESS implantation and those after trabeculectomy alone. Although no significant difference in surgical success rates between the two groups was found, implantation of an EX-PRESS device was significantly advantageous for prevention of postoperative overfiltration and hyphema in patients with NVG. EX-PRESS implantation may improve postoperative quality of vision in such patients. However, previous vitrectomy may have a negative effect on the surgical outcome after implantation of an EX-PRESS device in patients with NVG.
Acknowledgments
We are grateful to the optometrists of Gunma University for their assistance with the acquisition of the data used in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- BrownGCMagargalLESchachatAShahHNeovascular glaucoma. Etiologic considerationsOphthalmology19849143153206201791
- Sivak-CallcottJAO’DayDMGassJDTsaiJCEvidence-based recommendations for the diagnosis and treatment of neovascular glaucomaOphthalmology20011081017671776 quiz1777, 180011581047
- TakiharaYInataniMFukushimaMIwaoKIwaoMTaniharaHTrabeculectomy with mitomycin C for neovascular glaucoma: prognostic factors for surgical failureAm J Ophthalmol20091475912918918.e119195639
- ShenCCSalimSDuHNetlandPATrabeculectomy versus Ahmed glaucoma valve implantation in neovascular glaucomaClin Ophthalmol2011528128621468334
- NetlandPAIshidaKBoyleJWThe Ahmed glaucoma valve in patients with and without neovascular glaucomaJ Glaucoma201019958158620164790
- TraversoCEDe FeoFMessas-KaplanALong term effect on IOP of a stainless steel glaucoma drainage implant (Ex-PRESS) in combined surgery with phacoemulsificationBr J Ophthalmol200589442542915774918
- GoodTJKahookMYAssessment of bleb morphologic features and postoperative outcomes after Ex-PRESS drainage device implantation versus trabeculectomyAm J Ophthalmol20111513507513.e121236403
- NetlandPASarkisianSRJrMosterMRRandomized, prospective, comparative trial of EX-PRESS glaucoma filtration device versus trabeculectomy (XVT study)Am J Ophthalmol20141572433440.e324210765
- MarisPJJrIshidaKNetlandPAComparison of trabeculectomy with Ex-PRESS miniature glaucoma device implanted under scleral flapJ Glaucoma2007161141917224744
- SugiyamaTShibataMKojimaSUekiMIkedaTThe first report on intermediate-term outcome of Ex-PRESS glaucoma filtration device implanted under scleral flap in Japanese patientsClin Ophthalmol201151063106621847337
- Guven YilmazSYildirimSDegirmenciCAtesHEvaluation of Ex-PRESS mini glaucoma shunt implantation with preoperative intra-cameral bevacizumab injection in refractory neovascular glaucomaEur J Ophthalmol201626657558026951529
- KatoNTakahashiGKumegawaKKabataYTsuneokaHIndications and postoperative treatment for Ex-PRESS((R)) insertion in Japanese patients with glaucoma: comparison with standard trabeculectomyClin Ophthalmol201591491149826316691
- SidotiPADunphyTRBaerveldtGExperience with the Baerveldt glaucoma implant in treating neovascular glaucomaOphthalmology19951027110711189121760
- ArimuraSTakiharaYMiyakeSRandomized clinical trial for early postoperative complications of Ex-PRESS implantation versus trabeculectomy: complications postoperatively of Ex-PRESS versus trabeculectomy study (CPETS)Sci Rep201662608027184606
- GeddeSJHerndonLWBrandtJDBudenzDLFeuerWJSchiffmanJCPostoperative complications in the tube versus trabeculectomy (TVT) study during five years of follow-upAm J Ophthalmol20121535804814.e122244522
- GeddeSJSchiffmanJCFeuerWJHerndonLWBrandtJDBudenzDLTreatment outcomes in the tube versus trabeculectomy (TVT) study after five years of follow-upAm J Ophthalmol20121535789803.e222245458
- KiuchiYSugimotoRNakaeKSaitoYItoSTrabeculectomy with mitomycin C for treatment of neovascular glaucoma in diabetic patientsOphthalmologica2006220638338817095884
- SaitoYHigashideTTakedaHOhkuboSSugiyamaKBeneficial effects of preoperative intravitreal bevacizumab on trabeculectomy outcomes in neovascular glaucomaActa Ophthalmol20108819610219775309
- BeutelJPetersSLukeMBevacizumab as adjuvant for neovascular glaucomaActa Ophthalmol201088110310918811641
- MikiAOshimaYOtoriYKameiMTanoYEfficacy of intravitreal bevacizumab as adjunctive treatment with pars plana vitrectomy, endo-laser photocoagulation, and trabeculectomy for neovascular glaucomaBr J Ophthalmol200892101431143318815428
