Abstract
Purpose
To assess the safety, efficacy, and refractive predictability of half-fluence accelerated corneal collagen crosslinking (CXL) applied concurrently with photorefractive keratectomy (PRK), and compare the results to standard PRK.
Setting
Refractive Services, The Eye Foundation, Coimbatore, India.
Design
Interventional comparative case series.
Methods
Patients seeking refractive correction for myopia or myopic astigmatism were included in the study. Photorefractive keratectomy with concurrent half-fluence crosslinking (PRK Xtra) was performed in eyes with borderline suspicious tomography (not amounting to forme fruste keratoconus) or low pachymetry between 450 and 474 µm with an otherwise unremarkable corneal tomography. Eyes with normal corneal tomography and thickness between 475 and 500 µm underwent standard PRK. The minimum follow-up period was 1 year.
Results
In total, 109 eyes underwent PRK Xtra (Group A) and 118 eyes underwent PRK alone (Group B). The preoperative MRSE was −3.64 D and −3.38 D in Groups A and B, respectively (P=0.28). Group A had a significantly higher number of eyes with thinner corneas (P<0.01) and corneal tomographic abnormalities (P=0.02). At 1 year follow-up, 96.3% of eyes in group A as against 99.1% of eyes in group B achieved a best corrected distance visual acuity (CDVA) of 20/20 or better. No iatrogenic ectasia or hyperopic shift secondary to progressive flattening was noted in the PRK Xtra group. No significant difference in incidence of haze was noted.
Conclusion
PRK Xtra showed comparable safety, efficacy, and stability to PRK in eyes with thinner pachymetry and tomographic abnormalities. Combining crosslinking with PRK in suspicious tomographies augurs for safe and predictable outcomes.
Introduction
Iatrogenic keratectasia and myopic regression are well recognized complications following keratoablative procedures, both of which occur in part due to biomechanical weakening of the cornea.Citation1 Corneal ectasia presents as increasing myopia and astigmatism, due to progressive corneal steepening that occurs centrally or inferiorly.Citation2 A younger age group, lower residual corneal thickness, and high refractive errors are recognized as risk factors. Corneal collagen crosslinking (CXL) enhances corneal rigidity and reduces the possibility of long term myopic shift.Citation3 Prophylactic CXL has been applied concurrently with laser in situ keratomileusis (LASIK) to reduce the incidence of regression and possible ectasia.Citation4–Citation6
This study aims to investigate the potential differences in safety, efficacy, and refractive predictability of Photorefractive keratectomy (PRK) alone versus PRK with concurrent half fluence CXL in eyes with borderline corneal pachymetry or tomography.
Patients and methods
The study was an interventional comparative case series conducted on patients who presented to Refractive Services between January 2013 and August 2015. The study adhered to the tenets of the Declaration of Helsinki, and an approval was obtained from the Ethics Committee of our hospital (Ethics Committee of The Eye Foundation, Coimbatore). A written informed consent was obtained from all the patients enrolled in this study.
Patients seeking refractive correction for myopia or myopic astigmatism were included in the study. Primary inclusion criteria were age greater than 18 years, a stable refractive error (change in spherical equivalent of not more than 0.25 D) for at least 1 year, and discontinuation of contact lenses for a minimum duration of 2 weeks. Patients with a corrected distance visual acuity (CDVA) of 20/25 or better and a spherical equivalent refraction of up to −6.0 D were included in the study. Exclusion criteria included post ablation corneal thickness of less than 400 µm, topographic evidence of corneal ectasia, previous ocular surgery, history of herpetic eye disease, corneal scarring, collagen vascular disease, pregnancy, and lactation.
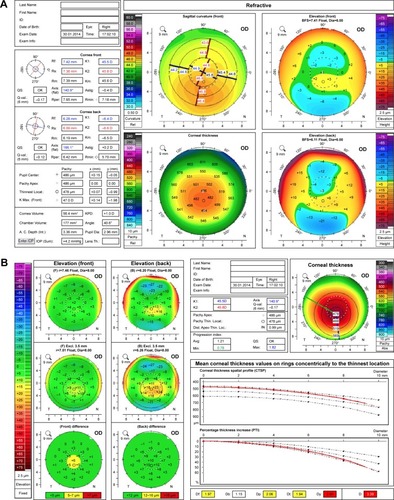
All patients underwent a detailed anterior and posterior segment evaluation to rule out ocular comorbidities. Corneal tomography was performed using the Oculus Pentacam Scheimpflug Imaging. Patients with a corneal pachymetry between 475 and 500 µm and normal corneal tomography were considered suitable candidates for PRK alone. Patients with corneal pachymetry between 450 and 474 µm and a normal tomography () or those exhibiting subtle tomographic abnormalities (mild inferior–superior asymmetry or overall D red) not amounting to forme-fruste or subclinical keratoconus () underwent PRK with concurrent half fluence CXL.
Figure 1 Preoperative corneal tomography of a patient seeking refractive correction for −2.50 D. Corneal tomography demonstrates a reduced pachymetry with no other abnormalities. The patient underwent PRK combined with CXL.
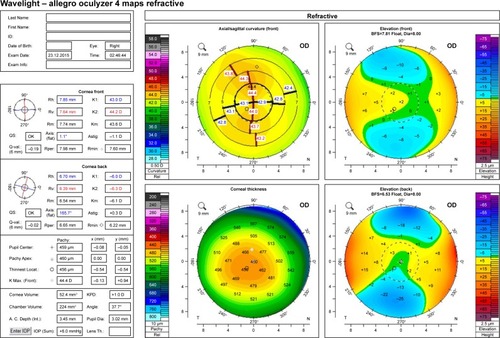
Figure 2 Preoperative corneal tomography of a patient seeking refractive correction; −3.50 D. Corneal tomography demonstrates an inferior superior asymmetry (A) with an overall D of red (B).
Surgical technique
Following instillation of proparacaine hydrochloride drops 1%, a wire lid speculum was placed. In all eyes, the excimer laser ablation was performed using the Wavelight Allegretto EX 500 system (Alcon Laboratories, Fort Worth, TX, USA). The epithelial removal was carried out using the phototherapeutic keratectomy mode at a pre-set depth of 50 µm. This was followed by myopic ablation treatment with a 6.00 mm treatment zone diameter and a transition zone of 1.25 mm. No adjustment in the excimer ablation nomogram was done for the PRK Xtra group.
Subsequent to the excimer laser treatment, mitomycin C (MMC) 0.02% was applied for 30 s in the PRK only group. The ocular surface was then washed thoroughly with normal saline solution, and a bandage contact lens was placed.
In patients undergoing concurrent CXL, 0.25% riboflavin drops (VibeX Xtra, Avedro, Waltham, MA, USA) were instilled over the exposed stroma and spread carefully over the stromal bed for the next 90 s. The riboflavin drops were applied immediately following ablation. Following the riboflavin soak, the excessive drops were irrigated and a half fluence UVA (ultraviolet A) irradiation at 30 mW/cm2 was applied for 90 s (energy dose of 2.7 J/cm2) using the KXL accelerated crosslinking device (Avedro Inc, Waltham, MA, USA). No further drops of riboflavin were administered during the UVA irradiation. A bandage contact lens was placed at the end of the procedure.
The postoperative protocol for both groups included loteprednol etabonate 0.5% topical suspension in tapering dose for 6 weeks, moxifloxacin hydrochloride eye drops 0.5% four times per day for a week, and polyethylene glycol and propylene glycol ophthalmic solution six times per day for 2 months.
Postoperative examination
Postoperative visits included postoperative day 1, day 5, 6 weeks, 3 months, 6 months, and 1 year. The bandage contact lens was removed on the fifth postoperative day following epithelium healing. Binocular and monocular uncorrected and best corrected visual acuity were recorded for both distance and near. Contrast sensitivity (Pelli-Robson contrast sensitivity test) was measured for both mesopic and photopic conditions. The secondary outcome measurements included incidence and resolution of corneal haze and incidence of residual error or regression.Citation7 Endothelial cell loss was measured using specular microscopy (Topcon SP). An anterior segment OCT (Avanti; Optovue Inc, Fremont, CA, USA) was used to measure the depth of the demarcation line in the PRK Xtra group at 1-month postoperative visit.
Statistical analysis
The type of refractive procedure (PRK Xtra vs PRK) was considered as the primary explanatory variable. Various visual outcome related parameters in the postoperative period were considered as outcome variables. Age, gender, and baseline visual parameters were considered as potential confounders.
All the quantitative variables were assessed for compliance with normal distribution within each treatment group by visual inspection of histograms, Normality Q–Q plots, and also by assessing the P-values of the Shapiro–Wilk test and Kolmogorov-Smirnov test.
All normally distributed quantitative variables were compared across the two groups by median and standard deviations using the Independent sample t-test to assess statistical significance. All the categorical variables were compared across the groups by crosstabulation and comparison of proportions using the chi-square test. P-value <0.05 was considered statistically significant.
Results
Patient demographics and characteristics are represented in . Of the 109 eyes belonging to group A (PRK Xtra), 52 patients underwent bilateral treatments and five were unilateral. The mean age in this group was 24.19±3.54 years. The preoperative mean refractive spherical equivalent (MRSE) was −3.64±1.44 D and the mean refractive error was −3.20±1.51 D sphere with −0.89±0.65 D cylinder.
Table 1 Demographics and patient characteristics
The second group (PRK alone) included 118 eyes. Of these, 56 patients underwent bilateral treatment and six were unilateral. The mean age was 25.92±4.91 years. The preoperative mean spherical refractive equivalent (MRSE) was −3.38±1.65 D and the mean refractive error was −3.09±1.44 D sphere with −1.05±0.94 D cylinder.
The mean preoperative central corneal thickness was 477.7±19.31 µm and 479.7±29.37 µm in Groups A and B, respectively (P=0.556). However, notably 58 eyes in the PRK Xtra group had a preoperative pachymetry between 450–474 µm as compared to none in the PRK group (P<0.01). Of the remaining 51 eyes in the PRK Xtra group, all of them had tomographic abnormalities with Overall D being yellow in 23 eyes and red in 28 eyes (P=0.02).
Postoperative uncorrected and best corrected visual acuity
Postoperatively an uncorrected visual acuity of 20/20 or better was achieved in 101 eyes (92.67%) in Group A and in 113 eyes (95.75%) in Group B. This difference was not statistically significant (P=0.14).
A best corrected visual acuity of 20/20 or better was achieved in 105 eyes (96.33%) and 117 eyes (99.1%) in groups A and B, respectively (P=0.23). Contrast sensitivity was measured both in photopic and mesopic conditions. Intra and intergroup comparison of preoperative and postoperative measurements did not reveal any significant difference between the two groups.
Refractive predictability and accuracy
A refractive predictability within 0.50 D was achieved in 95.4% and 97.4% of the eyes in groups A and B, respectively (P=0.8). Nine eyes in Group A had a residual error ranging from −0.25 D to −1.25 D, with a mean residual error of −0.59 D. Six eyes in group B had a residual error ranging from −0.25 D to −1.25 D, with a mean residual error of −0.60 D.s
Gain or loss of lines
The gain–loss data (preoperative CDVA versus postoperative CDVA) () indicates that, in group A, 90 eyes (82.56%) had unchanged CDVA, while one eye (0.91%) lost one line, 17 eyes (15.59%) gained one line, and one eye (0.91%) gained two lines in CDVA.
Figure 3 Change in corrected visual acuity, as number of eyes with gain/loss in Snellen lines of corrected distance visual acuity 1-year postoperatively.
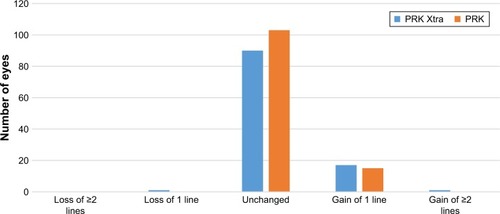
In group B, 103 eyes (87.29%) had no change, while 15 eyes (12.7%) gained one line in CDVA.
Refractive and keratometric stability
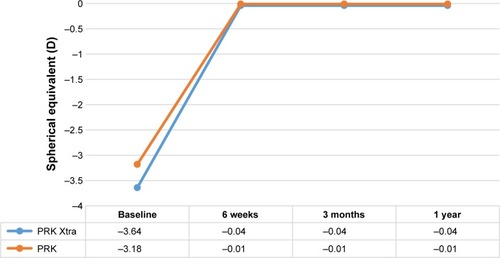
Refractive stability was demonstrated by the MRSE correction, as followed during the 6 weeks, 3 and 12 months’ postoperative visits (). The 1 year mean postoperative MRSE was −0.04±0.19 D and −0.01±0.10 D in groups A and B, respectively (P=0.153). None of the eyes in the PRK Xtra group noted overcorrection or hyperopic shift.
Figure 4 Refractive stability in both groups during 1 year follow-up.
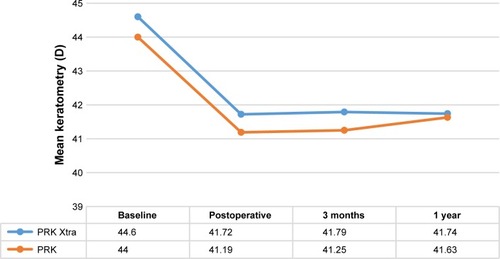
Keratometric changes in both groups were similar over a 1 year follow-up period (). A mean keratometric value of 41.74±2.17 D and 41.63±1.72 D at 1 year was seen in groups A and B, respectively (P=0.723). No progressive flattening or refractive shift was noted in either group.
Demarcation line
A patchy demarcation line was noted at a depth of 180.3±21.6 µm at 1-month postoperative visit in the PRK Xtra group.
Complications and adverse effects
No adverse effects like diffuse lamellar keratitis (DLK) or infections were reported in either groups. In the PRK Xtra group, nine eyes developed grade 1 superficial corneal haze, which resolved by the 6 month follow-up visit. It was of note that all these patients had a preoperative MRSE of greater than −3.0 D, with a mean of −4.4 D. Endothelial cell counts at preoperative and 1-month postoperative visit showed no statistically significant difference in both groups. No cases of postoperative ectasia were noted in either group, up to the last follow-up visit, with a mean follow-up of 28.4 months.
Discussion
Keratorefractive surgeries reduce the biomechanical strength of the cornea, both due to flap creation and stromal ablation.Citation1 The role of crosslinking to halt the progression of keratoconus by increasing the corneal rigidity has been well established.Citation3 The safety and efficacy of combining a partial surface ablation with crosslinking in keratoconic eyes has been described.Citation8–Citation10 Recently crosslinking has been combined with laser vision correction in eyes with high refractive errors, to reduce the incidence of regression.Citation4,Citation11,Citation12
In our study, patients with lower corneal pachymetry (between 450 and 474 µm) or those exhibiting subtle tomographic abnormalities (mild inferior–superior asymmetry or overall D red, not amounting to forme fruste or subclinical keratoconus) underwent PRK with half-fluence CXL. The concept behind applying concurrent CXL in these eyes was to compensate for the biomechanical weakness induced by the excimer ablation and to reduce the risk of ectasia and regression in these borderline corneas.
Progressive corneal flattening leading to overcorrection or visual loss following haze were some of the concerns behind combining CXL with laser vision correction. The advent of accelerated crosslinking methods enables us to achieve similar biomechanical stability as conventional treatment, without the induction of excessive corneal flattening.Citation13 In our study, we used accelerated crosslinking with a high irradiance of 30 mW/cm2 for a period of 90 s, delivering a total fluence of 2.7 J/cm2. This protocol has been used previously along with LASIK in eyes undergoing correction for high myopia and hyperopia.Citation4,Citation6 No correction or adjustment was made in the excimer laser algorithm for the PRK Xtra group. Similar studies combining laser in situ keratomileusis with CXL for myopic and hyperopic correction did not apply any corrections in the ablation algorithm.Citation4–Citation6 No overcorrection was noted in any of the eyes of the PRK Xtra group at 1 year follow-up. Hence, concurrent crosslinking in low dosage does not require undercorrection or adjustments in the excimer laser ablation nomogram.
MMC was not applied following laser ablation in the PRK Xtra group. A lower incidence of haze was expected due to crosslinking induced keratocyte apoptosis in the anterior corneal stroma. Nine eyes, however, developed postoperative grade 1 haze as against no eyes in the PRK only group. The haze, however, subsided within the first 6 months, and all eyes achieved a CDVA of 20/20. It is noteworthy that all patients presenting with haze received a refractive correction of greater than −3.0 D. Although the minimal haze did not affect the visual outcome in our series, we recommend the use of 0.02% MMC. Even when the laser correction is being combined with crosslinking in this accelerated half fluence mode, it is likely that the amount of apoptosis caused by this form of crosslinking may not be sufficient to prevent haze formation.
Conclusion
Our study was able to establish the safety and refractive efficacy of combining crosslinking with standard PRK in eyes with borderline corneal pachymetry and in eyes with subtle abnormalities on corneal tomography. Concurrent cross-linking in such corneas could help maintain biomechanical stability following excimer ablation. Long-term results are awaited to establish the superiority of this protocol.
What was known
Iatrogenic keratectasia and myopic regression are well recognized complications of keratoablative pro cedures, and CXL, when combined with LASIK, enhances corneal rigidity and reduces the possibility of long-term myopic shift.
What this paper adds
Combining half fluence crosslinking with standard surface ablation augurs for excellent refractive results in thin corneas and borderline corneal tomography, and no progressive flattening or hyperopic shift is seen, thereby maintaining the safety and efficacy of the refractive procedure.
Disclosure
The authors report no conflicts of interest in this work.
References
- RandlemanJBPost-laser in-situ keratomileusis ectasia: current understanding and future directionsCurr Opin Ophthalmol20061740641216900036
- BinderPSAnalysis of ectasia after laser in situ keratomileusis: risk factorsJ Cataract Refract Surg2007331530153817720066
- RandlemanJBKhandelwalSHafeziFCorneal cross-linkingSurv Ophthalmol20156050952325980780
- TamayoGEPredictable visual outcomes with accelerated corneal cross-linking concurrent with laser in situ keratomileusisJ Cataract Refract Surg2012381222062208
- AslanidesIMMukherjeeANAdjuvant corneal crosslinking to prevent hyperopic LASIK regressionClin Ophthalmol2013763764123576861
- CelikHUAlagözNYildirimYAccelerated corneal crosslinking concurrent with laser in situ keratomileusisJ Cataract Refract Surg20123881424143122814049
- NakamuraKKurosakaDBissen-MiyajimaHTsubotaKIntact corneal epithelium is essential for the prevention of stromal haze after laser assisted in situ keratomileusisBr J Ophthalmol20018520921311159488
- KanellopoulosAJAsimellisGKeratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens protocol)J Refract Surg201430889324763473
- KymionisGDKontadakisGAKounisGASimultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconusJ Refract Surg200925S807S81119772256
- KanellopoulosAJComparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconusJ Refract Surg200925S812S81819772257
- TomitaMYoshidaYYamamotoYMitaMWaringGIn vivo confocal laser microscopy of morphologic changes after simultaneous LASIK and accelerated collagen crosslinking for myopia: one-year resultsJ Cataract Refract Surg20144098199024857441
- KanellopoulosAJAsimellisGKarabatsasCComparison of prophylactic higher fluence corneal cross-linking to control in myopic LASIK: one year resultsClin Ophthalmol201482373238125473264
- ShettyRPahujaNNuijtsRMCurrent protocols of corneal collagen cross-linking: visual, refractive, and tomographic outcomesAm J Ophthalmol2015160224324926008626