Abstract
Optical coherence tomography (OCT) has emerged as a powerful diagnostic aid in disorders of the vitreoretinal juncture. The purpose of this study is to determine whether OCT can be used as an additional tool for evaluating an architecture including the thickened area, and the identifiable edge of a macular epiretinal membrane (ERM), and helping us to dissect the ERM from the retinal surface more easily and safely. In two cases with ERM, the edges of the membranes were detected by OCT, and the peeling of the membrane was started at the area easily. OCT guided ERM peeling might be useful for dissecting ERM membranes without any hesitation.
A macular epiretinal membrane usually develops after a partial or complete posterior vitreous detachment, and appears as a translucent membrane over the inner retinal surface in the macular area by ophthalmoscopy or biomicroscopy. Contraction of these membranes can result in various retinal pathologies, such as retinal distortion, increased thickness of the macula with or without increased permeability of retinal vessels, and cystoids macular edema.
Vision is decreased in eyes with macular epiretinal membranes for a variety of reasons: one or more full-thickness retinal folds, a trampoline-like sensory foveal elevation (tabletop-like traction), foveal ectopia created by an eccentric epiretinal membrane, retinal vascular leakage and macular edema, the presence of an opaque, dense membrane directly over the fovea, and traction-induced stasis of axoplasmic flow.Citation1
The goal of surgery is to relieve the traction caused by the macular epiretinal membrane. Frequently, the membrane can be directly visualized. If the membrane is difficult to identify, indocyanine green (ICG),Citation2 trypan blue,Citation3 and intravitreal triamcinolone crystalsCitation4 have been described to aid the surgeon in identifying the internal limiting membrane. If the membrane is thick and fibrotic, it may be possible to grasp the membrane directly with an intraocular end-grasping forceps and strip it away from the macular surface. In most cases, however, a barbed microvitreoretinal (MVR) blade or 25-gauge needle is employed to engage the membrane at its edge and elevate it from the retinal surface. The blade is then used to strip away connections to the retina on that side of the membrane where the dissection was initiated. During this initial maneuver, a “front” of elevated membranes is created, taking care not to fragment the membrane by pulling too hard or too long in any one direction. Once an entire side of the membrane has been elevated, fine-tipped intraocular forceps are used to continue the dissection. This dissection should be started over the thickest part of the membrane, or the identifiable edge of the membrane.
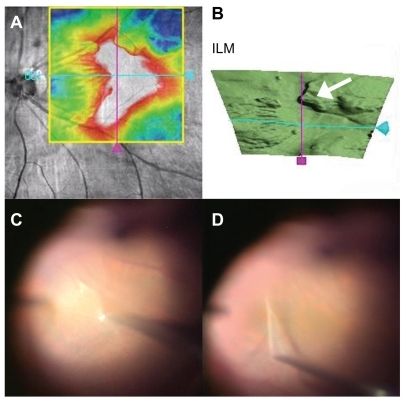
Optical coherence tomography (OCT) has emerged as a powerful diagnostic aid in disorders of the vitreoretinal juncture.Citation5 The use of OCT has allowed clinicians to evaluate the architecture and cross-sectional thickness of the neurosensory retina and its anatomic relationship to the retinal pigment epithelium and posterior hyaloids. In eyes with macular epiretinal membrane, the use of OCT may be helpful to determine the thickest part of the membrane, and the identifiable edge of the membrane. In , the arrow indicates the edge of the membrane (), and shows the thickest part of the membrane (). We can start the peeling of the macular epiretinal membrane more easily if we have had this information by OCT preoperatively. Here we show that we performed vitrectomy with epiretinal membrane peeling on the basis of the OCT findings obtained preoperatively in . We confirmed the area and thickness of the epiretinal membrane (), found the edge of the membrane (), and started the peeling at that point (). We might be able to perform a surgery without any hesitation if we received these details of epiretinal membranes preoperatively.
Figure 1 The right eye of a 71-year-old patient with idiopathic epiretinal membrane. All OCT images are obtained by spectral-domain OCT (Cirrus™ HD-OCT, Carl Zeiss Meditec, Jena, Germany). A) Horizontal image of optical coherence tomography (OCT) shows epiretinal membrane over the macula.. The arrow shows the identifiable edge of the membrane. B) Three dimensional retinal map images obtained by OCT. The arrows show the membrane that was elevated from the internal limiting membrane (ILM). C) Retinal map image obtained by OCT shows the range of epiretinal membrane. The arrow shows the thickest part of the membrane.
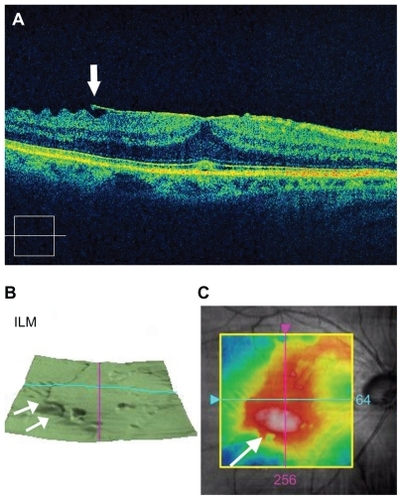
Figure 2 The right eye of a 75-year-old patient with idiopathic epiretinal membrane. A) Retinal map image obtained by optical coherence tomography (OCT) shows the range of epiretinal membrane. B) Three dimensional retinal map images obtained by OCT. The arrow shows the membrane that was elevated from the internal limiting membrane (ILM). C, D) Intraoperative photographs. C) 25-gauge micro-hooked needle was used to elevate the epiretinal membrane from the retinal surface. Because the membrane was elevated from the ILM (arrow) as shown by OCT (B) it was easy to pick up the edge of the membrane. D) One-piece membrane was removed by 25-gauge micro-hooked needle.
There are no complications in this OCT-guided epiretinal membrane (ERM) peeling because OCT provides only additional information to assist the conventional procedure of ERM peeling. When the peeling point is located between the fovea and the optic disc, surgeons should take extra care when peeling or choose another peeling point. OCT-guided ERM peeling is useful in cases in which edges of the membrane are apart from the retinal surface, but all cases are applicable and beneficial because ERMs usually have a thickened portion. Edges of epiretinal membranes were not always detected by OCT, but a thickened area could be usually determined. To start peeling off the membrane at the thickened area might prevent a macula from being injured by a blade or needle, which is used for membrane peeling. Furthermore, findings obtained by OCT simplifies the procedure because we do not have to find the area where we should start membrane peeling during surgery. OCT-guided ERM peeling might be useful for dissecting ERM membranes.
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- McDonaldRGAabergTMIdiopathic epiretinal membranesSemin Ophthalmol19861189195
- KwokAKYeungYSLeeVYICG-assisted peeling of the retinal ILMOphthalmology2002109104012045036
- FeronEJVeckeneerMParys-Van GinderdeurenRTrypan blue staining of epiretinal membranes in proliferative vitreoretinopathyArch Ophthalmol200212014114411831915
- FraserEACheemaRARobertsMATriamcinolone acetonide-assisted peeling of retinal internal limiting membrane for macular surgeryRetina20032388388414707850
- HuangDSwansonEALinCPOptical coherence tomographyScience1991254117811811957169