Abstract
Purpose
The aim of this study was to determine whether a significant correlation exists between the scotopic and photopic components of electroretinograms (ERGs) and the degree of circulation disturbances caused by a central retinal artery occlusion (CRAO).
Design
Observational clinical study.
Participants
Sixteen patients with a CRAO (16 eyes).
Methods
The circulatory disturbance in eyes with CRAO was graded as mild (group 1) when the arm-to-retina transmission time was <30 sec and severe (group 2) when the arm-to-retina transmission time was ≥30 sec. Scotopic and photopic ERG components in eyes with CRAO were compared with those in healthy fellow eyes with respect to the degree of circulation disturbance.
Results
The scotopic and photopic b-waves were significantly reduced only in group 2, whereas the amplitudes of the photopic negative response (PhNR) of the photopic cone ERGs were significantly reduced in both groups. The amplitudes of each ERG component, except for the a-wave of the mixed rod-cone ERG, were significantly smaller in group 2 than in group 1.
Conclusions
The PhNR was reduced even in group 1 with minimal circulatory disturbance and thus may be a good functional indicator.
Introduction
A central retinal artery occlusion (CRAO) is one of the most serious vascular obstructive disorders of the eye. Several types of treatments have been considered for the acute phase of CRAO.Citation1 The European Assessment Group for Lysis in the Eye (EAGLE) study was a multicenter, randomized trial that evaluated the efficacy and adverse effects of treating a CRAO by conventional isovolemic hemodilution or by local intra-arterial fibrinolysis.Citation2 The authors reported that the improvement of visual acuity was similar in both groups and concluded that because of the similar outcomes and higher rate of adverse reactions associated with intra-arterial fibrinolysis, they could not recommend intra-arterial fibrinolysis.
The electroretinographic (ERG) findings in eyes with CRAO are characterized by a decrease of the b-wave because of the inner layer retinal ischemia.Citation3–Citation5 However, Miyake clearly showed that the visual field defects and the alterations of the ERGs were often inconsistent in eyes with CRAO. For example, the visual fields may be extremely constricted and the visual acuity may be severely reduced, but the ERGs can be well preserved.Citation6
Although the function of the retinal layers that give rise to the ERGs can recover to a certain extent following a return of the retinal circulation, the retinal ganglion cells (RGCs) usually suffer irreversible damage soon after the occlusion because they are more vulnerable to ischemia. The histopathological changes associated with a CRAO include the death of the RGCs by apoptosis.Citation7 Machida et al reported that the photopic negative response (PhNR) of the ERG can be used to assess the retinal function following retinal vascular disorders.Citation8 Moreover, they showed a selective attenuation of the PhNR amplitude in eyes with a CRAO, but the relationship to other clinical findings was not presented.
At present, the effects of CRAO are assessed by visual acuity, fundus appearance, and fundus fluorescein angiography (FA), but a correlation between the different components of the ERG and the degree of circulation disturbances has not been determined. Recently, we reported that the PhNR reflects the severity of ocular circulatory damage in CRAO in the same patients used in this study.Citation9 In the earlier study, we focused on the photopic ERG components and especially the PhNR. In this study, the scotopic and photopic components of the ERGs recorded according to the recommendations of the International Society for Clinical Electrophysiology of Vision (ISCEV) were analyzed.Citation10
The aims of this study were to correlate the scotopic and photopic components of the ERGs recorded according to the recommendation of the ISCEVCitation11 with the degree of circulation disturbances and to investigate whether these findings can be indicators of the severity of the retinal alterations in CRAO patients.
Patients and methods
The medical records of 16 eyes of 16 consecutive patients with a CRAO who were examined at the Oita University Hospital, Oita, Japan, from 2003 to 2007 were analyzed. The procedures used conformed to the tenets of the Declaration of Helsinki, and an informed consent was obtained from all patients after the nature of the study had been fully explained.
A complete ophthalmological examination was performed on each patient. The diagnosis of CRAO was made by the findings obtained by indirect ophthalmoscopy and FA. Because the aim of the study was to determine which ERG components were significantly correlated with the retinal circulatory disturbance, the arm-to-retina time was chosen instead of visual acuity or visual field as the functional parameter. To determine the arm-to-retina circulatory time, 5 mL of 10% fluorescein sodium was injected into the cubital vein, and the time between the injection of the dye and its first appearance in the retinal artery was measured as the arm-to-retina circulation time.
Based on the FA and/or indocyanine green choroidal angiographic findings, eyes with CRAO were divided into two groups. Eyes with choroidal and retinal circulation disturbances were considered to have the most severe retinal changes and were excluded from the analysis.Citation12 The normal arm-to-retina transmission time is known to be not >15 sec.Citation12 Eyes with an arm-to-retina transmission time <30 sec were placed in the mild group (group 1), and eyes with an arm-to-retina transmission time ≥30 sec were placed in the severe group (group 2). For statistical analysis, each group was scored as 1 and 2, corresponding to the group number (circulation severity score).
The patients consisted of six men and seven women ranging in age from 44 to 81 years (mean 68.8 years). Patients with other retinal diseases were excluded. All emergency treatment procedures, eg, ocular massage, lowering of the intraocular pressure (IOP), and administration of thrombolytic agent, were performed before or on the same day as the ERG recordings. ERGs were recorded from the 13 eyes with CRAO and 12 of the normal fellow eyes as controls. The onset of the CRAO was determined by the patients’ subjective ocular symptoms. One patient had a branch retinal vein occlusion in the fellow eye.
The clinical findings of the cases with CRAO are presented in . The IOP was measured before each ERG recording by applanation tonometry, and none of the patients had an IOP >19 mm Hg.
Table 1 Demographics of the patients with CRAO
Electroretinography
The ERG recordings were performed on the same day or on the day after the treatment started. Scotopic mixed rod-cone ERGs and photopic-cone ERGs were elicited by stroboscopic stimuli, and the recordings were made according to the standards recommended by the ISCEV.Citation10 A customized 30 cm diameter Ganzfeld ColorDome stimulator was used to present the stimuli. The patients’ pupils were fully dilated with 0.5% tropicamide and 0.5% phenylephrine hydrochloride. The ERG responses were recorded with a corneal bipolar electrode (7819NFC-4; Mayo Corp, Inazawa, Japan) placed on the anesthetized cornea. The eyes were dark-adapted for 20 min before the scotopic recordings and light-adapted for 10 min before the photopic recordings. ERGs with poor signal-to-noise ratio were excluded.
The ERGs were elicited by flashes of white light from a white light-emitting diode. The rod ERG was elicited with white flashes at an intensity of 100 cd/m2. To elicit the standard combined rod-cone ERGs and bright-flash ERGs, 1000 cd/m2 and 8000 cd/m2, respectively, white flashes were delivered. The stimulation rate was 0.1 Hz in the dark-adapted state. The cone ERGs were elicited with the same white flashes at an intensity of 1000 cd/m2 on a white background of 25 cd/m2 with a frequency of 0.5 Hz. The 30 Hz flicker ERG was elicited with white pulses at 100 cd/m2 on a white background of 25 cd/m2. To improve the signal- to- noise ratio, four ERGs were averaged and analyzed. The ERG elicited by the first flash was excluded from the average.
The ERGs were amplified by a bioamplifier (Neuropack; Nihon Kohden, Tokyo, Japan), with the low- and high-bandpass filters set at 0.1 and 1000 Hz, respectively. The ERGs were digitalized with a 12 bit A/D board (AD 32/10HD; Contec, Osaka, Japan) and averaged online, and offline if necessary, using customized software (Multi Analyser EP; MTS, Tokyo, Japan).
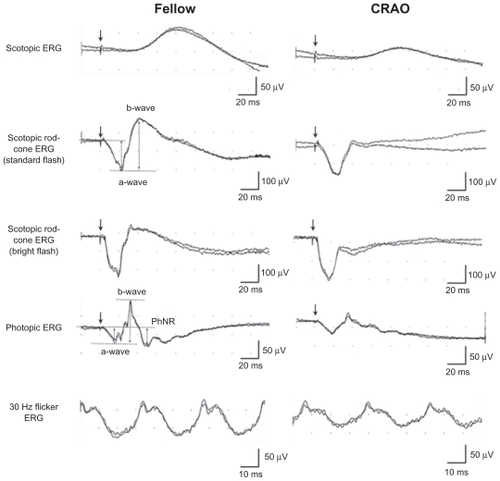
Representative scotopic and photopic ERGs are shown in . The amplitudes and peak implicit times of the scotopic and photopic ERGs were measured as shown in . The PhNR elicited by red stimuli on a blue backgroundCitation13–Citation15 was not available in this study. Therefore, the amplitude of the negative trough was analyzed following the cone ERG b-wave as the PhNR. One-factor analysis of variance followed by Scheffé’s F post hoc test was performed to evaluate the differences among the three groups, ie, two groups of eyes with a CRAO and a control group of healthy fellow eyes. A P value < 0.05 was considered to be statistically significant.
Results
The time interval between the CRAO and the ERG recording ranged from 2 h to 30 days (7.4 ± 10.8 days; ). Two patients whose ERG was measured 30 days after onset of CRAO were excluded from the ERG analyses so that the time interval ranged from 2 h to 13 days (3.2 ± 4.3 days). Of the 11 eyes, four were placed in group 1 and seven in group 2. A partial internal carotid artery obstruction was found in three patients.
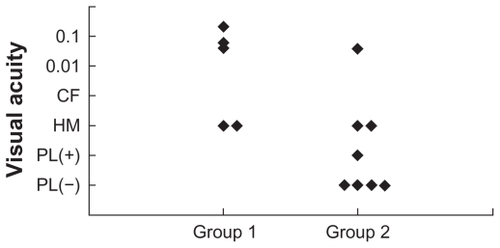
The distribution of the visual acuities is shown in . The visual acuity was significantly higher in group 1 than in group 2. The visual fields were available only on two eyes: cases 5 and 6 (). Case 5 showed a temporal defect with a central scotoma, and case 6 had a nasal defect with a central scotoma according to the classification of Hayreh and Zimmerman.Citation16
Figure 2 Distribution of the visual acuities at the initial visit in the two groups.
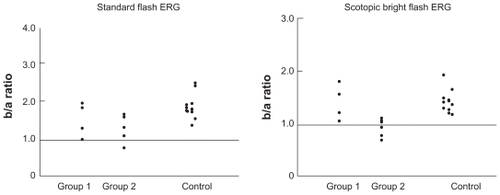
The b-wave/a-wave (b/a) ratios of the scotopic standard-flash ERG and the scotopic bright-flash ERG are plotted in . The mean b/a ratio was low in eyes with a CRAO, but only one eye showed the negative type for the scotopic standard-flash ERG, ie, a b/a ratio <1.0.
Figure 3 The b-wave/a-wave ratio of the ERGs in eyes with a CRAO and the fellow eyes elicited by standard flash (left) and by scotopic bright flash (right) recommended by the ISCEV. Only one eye with a CRAO had a b/a ratio <1.0 in the recordings with standard flash (left). The error bars represent the standard deviation.
The average amplitudes of the ERGs recorded under scotopic condition in the two groups and the control fellow eyes are shown in . The average b-wave amplitudes of the scotopic rod ERGs in both affected groups were significantly smaller than those in the control eyes. The average a-wave amplitudes of the mixed rod-cone ERGs in group 2 were reduced, but the decrease was not significant compared with the control eyes, whereas the average b-wave amplitudes of the mixed rod-cone ERGs in group 2 were significantly smaller than those in the control eyes.
Figure 4 Average amplitudes of the ERGs recorded under scotopic conditions in the two groups and the control fellow eyes. Left: the amplitudes of the b-wave of the scotopic rod ERG. Middle and right: the amplitudes of the a- and b-waves of the ERGs elicited by the standard flash, respectively. The amplitude of scotopic rod b-wave was significantly lower in groups 1 and 2 compared with control. In addition, the b-wave of the mixed rod-cone ERG was significantly smaller in group 2 than in the controls. Controls are the healthy fellow eyes of all the patients. The error bars represent the standard deviation.
Abbreviation: ERG, electroretinogram.
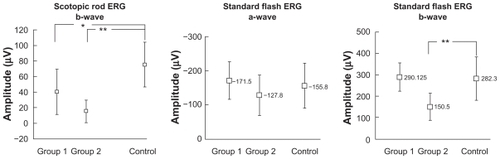
The ERGs recorded under photopic condition are shown in . The photopic a-wave amplitudes were decreased in group 2, but the decrease was not statistically significant compared with the control eyes. The photopic b-wave was significantly smaller in group 2, and the amplitude of the PhNR in the control fellow eye was significantly larger than the PhNR for both affected groups. The 30 Hz flicker ERG was significantly reduced in group 2.
Figure 5 Average amplitudes of ERGs recorded under photopic condition in the two groups and the control fellow eyes. Only the PhNR is significantly different in group 1 from the controls. The controls are the healthy fellow eyes of all the patients. The error bars represent the standard deviation.
Abbreviations: ERG, electroretinogram; PhNR, photopic negative response.

In summary, significant reductions in the scotopic rod b-wave and the PhNR were found only in the group 1 eyes.
Discussion
Results showed that the amplitudes of the b-wave of the scotopic and photopic ERGs were significantly smaller in an eye with a CRAO than in the fellow control eye. On the other hand, the amplitude of the a-wave was not significantly reduced. The b/a ratio was also smaller in eyes following a CRAO. These findings are in agreement with the known origins of the a- and b-waves, ie, that the a-waves originate from the activity of postphotoreceptoral cells, including the off-bipolar cells and photoreceptors, and the b-waves from the activity of the inner retina but not the RGCs.
The new finding in this study was the high correlation between the degree of reduction of the scotopic b-wave and degree of ocular circulation disturbances, and between the degree of reduction of the PhNR and degree of ocular circulation disturbances.
In a physiological study of a primate model of transient CRAO, the ERGs and visual-evoked responses were found to tolerate 94–100 min of ischemia, but the retinal damage was more severe, extensive, and irreversible following longer periods of ischemia.Citation17,Citation18 However, because only a minority of patients have a complete obstruction of the retinal blood flow and most have a partial or transient obstruction, the results of the primate model of CRAO may not reflect the pathophysiology of CRAO in these patients. As reported, a recovery of visual function can be obtained even in cases who were treated >18 h after the onset of the CRAO,Citation19 suggesting that retinas can tolerate a transient obstruction.
The a-wave of the scotopic ERG was generally unaffected, but the scotopic b-wave amplitude was reduced. However, a negative-type ERG was observed in only one case of CRAO in the ERGs elicited by the ISCEV standard-flash stimuli. Because the severity of the retinal ischemia differed widely among these patients, with most of the cases having a partial and/or transient obstruction of the central retinal artery, variations in the amplitudes of the ERG components would be expected. In an experimental study of the retinal survival time, Hayreh et al reported that the b/a ratio of the combined rod-cone responses were significantly different between those with shorter and longer periods of CRAO.Citation18 A previous study on animals showed that the correlation between the ERG parameters and the histological changes with any of the residual retinal circulation variables was not significant.Citation18
In this study, 1000 cd/m2 and 8000 cd/m2 white flashes were used to elicit the standard combined ERG and bright- flash ERG, respectively. In the V-log I curve,Citation20 where the amplitudes of the a- and b-waves are plotted against the logarithm of stimulus intensity, the b-wave amplitude reached the plateau, whereas the a-wave amplitude was still in the ascending part with 1000 cd/m2. Therefore, a b/a ratio <1.0 was not often observed in this series, and with an intensity of 8000 cd/m2, which was used to elicit bright-flash ERGs, the b-wave amplitude was on the plateau and the a-wave amplitude was still growing. Therefore, the incidence of the eye with a b/a ratio <1.0 was higher under these conditions. It was reported that the negative-type waveform was more frequently detected when 1 log unit higher stimulus intensity was used to elicit the ERGs in eyes with congenital stationary night blindness and x-linked retinoschisis.Citation21,Citation22
This study had several limitations, eg, small sample number, lack of widely accepted quantitative indicators for retinal circulation disturbances, large range in the time from CRAO onset to recording the ERG, and different treatments for CRAO because of the retrospective nature of the study. It would be interesting to use other parameters of retinal circulation, such as those obtained by a laser flowmeter or ocular fundus blood pressure measurements. In addition, the PhNR was not elicited by the most effective stimuli.Citation13–Citation15 Instead, the PhNR corresponding component of the cone ERG elicited by the ISCEV standard was analyzed, considering that it would contain the majority of the original PhNR. Further investigations on the pure PhNR and its correlation to the clinical parameters in CRAO patients should be carried out. The results obtained in this study should be carefully interpreted, but this study still provides clinically useful evidence that the b-wave and a-wave would be good indicators of the severity of retinal ischemia in CRAO patients.
The PhNR corresponding component was reduced even in group 1 with minimal severity of circulatory disturbances and where a- and b-waves of the scotopic and photopic ERG showed almost no alteration compared with those in control eyes. These findings suggest that PhNR corresponding component is the most affected and possibly the more sensitive component of the ERG following retinal circulation injuries. This is in good accordance with previous studies reporting that the PhNR of the photopic ERG originated from the inner retina and reflected the activity of the RGCs.Citation13,Citation14,Citation23 In addition, Machida et al have shown that the PhNR was the most affected wave in seven cases of CRAO.Citation8 Together with the previous evidence, these results show the high correlation of the ERG parameters, especially PhNR, with the severity of CRAO. A useful ERG parameter to determine the prognosis of retinal vessel occlusion is needed. Recently, the implicit time of the 30 Hz flicker ERG has been reported to be a good indicator for the development of ocular neovascularization after a central retinal vein occlusion.Citation24 Further investigations to determine the ERG parameters that are significantly correlated with the visual prognosis in CRAO patients are needed.
Acknowledgments
This study was supported by Research on Sensory and Communicative Disorders from the Ministry of Health, Labor, and Welfare and from the Ministry of Education, Culture, Sports, Science and Technology, Japan. No author has a financial or proprietary interest in any material or method mentioned.
Disclosure
The authors report no conflicts of interest in this work.
References
- FraserSSiriwardenaDInterventions for acute non-arteritic central retinal artery occlusionCochrane Database Syst Rev20021CD00198911869617
- SchumacherMSchmidtDJurkliesBCentral retinal artery occlusion: local intra-arterial fibrinolysis versus conservative treatment, a multicenter randomized trialOphthalmology2010117713671375e120609991
- CarrRESiegelIMElectrophysiologic aspects of several retinal diseasesAm J Ophthalmol1964589510714177989
- HamasakiDIKrollAJExperimental central retinal artery occlusion. An electrophysiological studyArch Ophthalmol19688022432484969419
- JohnsonMADisease of the middle retina: venous and arterial occlusionsHeckenlivelyJRArdenGBPrinciples and Practice of Clinical Electrophysiology of VisionCambridge (MA)MIT Press2006675681
- MiyakeYCentral reinal artery occlusionMiyakeYElectrodiagnosis of Retinal DiseasesTokyoSpringer-Verlag2006181182
- ZhangYChoCHAtchaneeyasakulLOMcFarlandTAppukuttanBStoutJTActivation of the mitochondrial apoptotic pathway in a rat model of central retinal artery occlusionInvest Ophthalmol Vis Sci20054662133213915914634
- MachidaSGotohYTanakaMTazawaYPredominant loss of the photopic negative response in central retinal artery occlusionAm J Ophthalmol2004137593894015126164
- MatsumotoCSShinodaKYamadaKNakatsukaKPhotopic negative response reflects severity of ocular circulatory damage after central retinal artery occlusionOphthalmologica2009223636236919590251
- MarmorMFHolderGESeeligerMWYamamotoSInternational Society for Clinical Electrophysiology of VisionStandard for clinical electroretinography (2004 update)Doc Ophthalmol2004108210711415455793
- RizzoJFIIINeuroophthalmologic disease of the retinaAlbertDMJakobiecFAPrinciples and Practice of Ophthalmology2nd edPhiladelphia (PA)WB Saunders Company200040834108
- JohnsonRNMcDonaldHRAiEJumperJMFuADFluorescein angiography: basic principles and interpretationRyanSJRetinaPhiladelphia, PAMosby2006873915
- ViswanathanSFrishmanLJRobsonJGHarwerthRSSmithEL3rdThe photopic negative response of the macaque electroretinogram: reduction by experimental glaucomaInvest Ophthalmol Vis Sci19994061124113610235545
- ViswanathanSFrishmanLJRobsonJGWaltersJWThe photopic negative response of the flash electroretinogram in primary open angle glaucomaInvest Ophthalmol Vis Sci200142251452211157891
- RangaswamyNVFrishmanLJDorotheoEUSchiffmanJSBahraniHMTangRAPhotopic ERGs in patients with optic neuropathies: comparison with primate ERGs after pharmacologic blockade of inner retinaInvest Ophthalmol Vis Sci200445103827383715452095
- HayrehSSZimmermanMBCentral retinal artery occlusion: visual outcomeAm J Ophthalmol2005140337639116138997
- HayrehSSKolderHEWeingeistTACentral retinal artery occlusion and retinal tolerance timeOphthalmology198087175786769079
- HayrehSSZimmermanMBKimuraASanonACentral retinal artery occlusion. Retinal survival timeExp Eye Res200478372373615106952
- MatsumotoHMatsumotoSSNagataMFurushimaMNakatsukaKEmergency treatment of simultaneous occlusion of central retinal artery and vein [in Japanese]Jpn J Clin Ophthalmol2005596923927
- LamBLFull-field electroretinogramLamBLElectrophysiology of Vision: Clinical Testing and ApplicationsBoca Raton, FLTaylor & Francis Group2005164
- MiyakeYKey points of clinical ERG recordings and data analysis. ISCEV protocol and controversial points [in Japanese]Folia Ophthalmol Jpn199344519524
- MiyakeYYagasakiKHoriguchiMKawaseYKandaTCongenital stationary night blindness with negative electroretinogram. A new classificationArch Ophthalmol19861047101310203488053
- ChenHWuDHuangSYanHThe photopic negative response of the flash electroretinogram in retinal vein occlusionDoc Ophthalmol20061131535916944088
- KjekaOBredrupCKrohnJPhotopic 30 Hz flicker electroretinography predicts ocular neovascularization in central retinal vein occlusionActa Ophthalmol Scand200785664064317403019