Abstract
Purpose
There are multiple reports of the role of corneal hysteresis (CH) as an independent risk factor for the diagnosis and risk of progression of normal-tension glaucoma (NTG). Our study measured CH with the Ocular Response Analyzer (ORA) in patients with intraocular pressure (IOP) <21 mmHg to investigate if a low CH would identify NTG in this Asian-based practice.
Methods
This was a prospective cross-sectional study of patients who underwent routine eye examination during 2016 in a private practice in Honolulu, Hawaii, where most patients are Asian. Inclusion criteria are: 1) ≥65 years 2) IOP <21 (compensated IOP by ORA), and 3) CH values <10 using ORA as measured by a single experienced technician. Exclusion criteria are: 1) sight-limiting ocular or corneal disease that would preclude accurate measurements for the purposes of the study. 2) Any patient who had difficulty in being tested with the ORA. 3) Patients who had any history of any type of glaucoma. All patients that met the inclusion criteria underwent fundus photography to measure cup-to-disc ratio and cup-to-disc asymmetry and also had central corneal thickness measured. Thickness of the retina nerve fiber layer was measured by ocular coherence tomography. The eyes with an average retina nerve fiber layer thickness less than 80 μm were classified as possible NTG and were scheduled for a visual field test. The field examination was considered valid only if the fixation, false positives, and false negatives were within the acceptable range. Patient demographics and data on preexisting diseases were collected including age, sex, coexisting medical conditions, and previous intraocular surgery. Those with thinning of retina nerve fiber layer on optical coherence tomography had a Humphrey visual field test to confirm the diagnosis of glaucoma.
Results
Seventy-six eyes of 46 patients that met the eligibility criteria were included in the study. Twenty-one previously undiagnosed eyes were confirmed as having NTG, which corresponds to an incidence of 27.6%.
Conclusion
CH measurement is a valuable test to assist in early diagnosis of NTG, especially in the elderly Asian population. With an established diagnosis, aggressive early treatments medically or surgically to further lower IOP can prevent irreversible blindness, which can severely impact the patient’s family and socioeconomic status.
Introduction
Glaucoma is a silent and sight-threatening disease caused by slowly progressive damage to the optic nerve. In patients over the age of 60, glaucoma is the leading cause of blindness.Citation1 The estimated prevalence of glaucoma in the USA is 3 million, and up to one half of these cases are undiagnosed.Citation1 Glaucoma affects more than 70 million people worldwide, 10% of whom are bilaterally blind, and 50%–90% are undiagnosed.Citation2,Citation3 This prevalence is expected to increase in parallel with the increasing life expectancies to 111.8 million in the year 2040.Citation3 Despite its significance, the underlying pathogenesis of glaucoma remains largely mysterious. Moreover, its diagnosis is often delayed as a majority of patients remain asymptomatic until the late stages and since awareness among the general population is relatively low.Citation4–Citation7
Early detection of glaucoma is the key for prevention of progressive visual loss with the treatment of aggressively lowering intraocular pressure (IOP). Normal-tension glaucoma (NTG) is particularly hard to detect given that the IOP is within normal limits, especially in the Japanese population. It is often overlooked until a late stage, which leads to irreversible visual impairment. In a recent review of population-based glaucoma prevalence, the calculated mean proportion of NTG was larger in Asian (76.3%) than in a white population (33.7%).Citation8
To date, the highest NTG proportion reported was 92.0%, from the Tajimi StudyCitation6 conducted in Japan, and the lowest was 30%, from the Italian Egna-Neumarkt Study.Citation9
Use of a fundus ophthalmoscope together with fundus camera photography is a good way to detect abnormalities in the disc such as irregularity, paleness, large cup size, hemorrhage, or loss of rim to diagnose low-tension glaucoma. However, hazy media from coexisting cataract or other eye pathologies prohibit a good examination, in addition to possible poor cooperation for detailed examination by patients.
One of the reasons that IOP is always lower than true pressure is the weakness of cornea biomechanics from aging or various corneal diseases and gives the reading of normal intraocular pressure from various tonometry, hence delay the treatment for years until irreversible vision loss occur and then bring patients to see eye professionals.
Corneal biomechanical properties are correlated and associated with the progression of visual field damage in NTG patients as indicated in many previous studies (). Corneal hysteresis (CH) is a mechanical property of the cornea that can affect the accuracy of IOP measurement. Several recent studies suggest that low CH is a risk factor for the development of glaucoma.Citation10 These findings also suggest that CH () can be used as one of the diagnostic and prognostic factors for progression of NTG that is independent of corneal thickness or IOP.
Figure 1 What is hysteresis and CH?
Abbreviation: CH, corneal hysteresis.
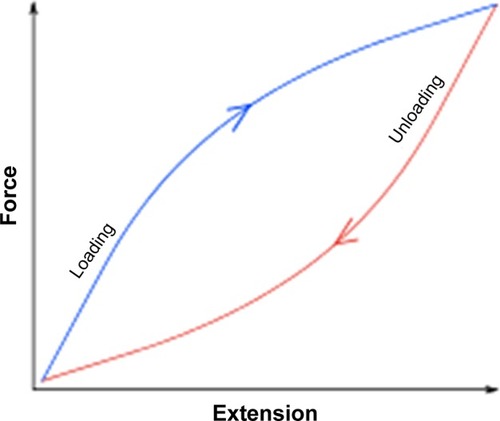
Table 1 Chronological list of studies correlating CH and glaucoma
We thus studied a series of cases to detect NTG by using Ocular Response Analyzer (ORA, Reichert instruments, Depew, NY, USA) to check CH () as one of the screening methods and to confirm the diagnosis with optical coherence tomography (OCT) and visual field test. CH below 10 mmHg was considered low for this study.
Methods
The study was conducted in this single general ophthalmologic practice where the ORA was available. Those patients without any history of glaucoma aged 65 years and older with IOP consistently below 21 mmHg and CH below 10 mmHg were included in the study (). Patients with severe corneal disease eye such as opacity and/or keratitis were excluded due to possible ORA reading errors. In order for reliable visual field and OCT exam, the patients included were educated to understand the visual field test.
Table 2 Characteristics of study subjects
Seventy-six eyes of 46 patients that met the eligibility criteria were included in the study. Comprehensive complete eye exams were performed that included CH measurement through ORA. Patients were selected according to the following criteria. Those with CH lower than 10 mmHg were scheduled for OCT to check retina nerve fiber layer (RNFL) thickness. Those eyes that had a value lower than 80 on RNFL exam and significant loss of nerve fiber on the OCT were then assessed with a visual field examination. Visual field exam results were carefully evaluated by the patients medical doctor (MD) specializing in Ophthalmology, for any valid abnormality.
This study has been approved by the institutional review committee of the University of Hawaii, # 2017-00386. All patients signed the inform consent to enter the study.
Results
Seventy-six eyes of 46 patients that met the eligibility criteria were included in the study. Twenty-one previously undiagnosed eyes were confirmed as having NTG, which corresponds to an incidence of 27.6% (). We found no statistically significant difference between normal eyes and NTG eyes in CH (P=0.19); however, the average RNFL between normal eyes and NTG eyes had a statistically significant difference (P<0.001) ().
Figure 2 The percentage of NTG after screening those with the low CH (below 10) by OCT and visual field.
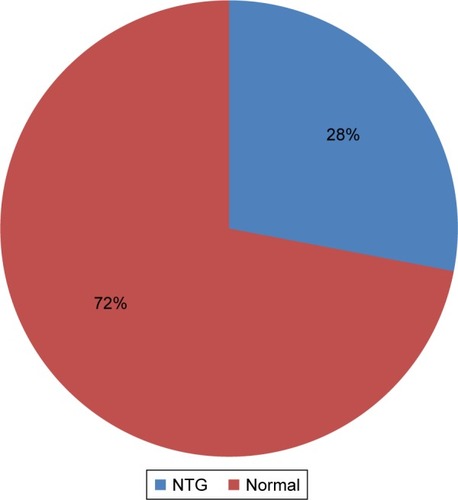
Table 3 Comparison between two groups with respect to CH and average thickness of RNFL
Discussion
As the lifespan of humans is increasing, the eyes of the elderly are also degenerating accordingly. The degeneration of cornea, optic nerve, and retina can affect visual ability and lifestyle of the elderly. Some of these patients were diagnosed as having NTG because they had vision loss with normal IOP. According to our study, patients who were Asian, older (above 75 years old), women, and having undergone cataract surgery made them more likely to have NTG.
Corneal degeneration causing low CH can give a normal reading for the measurement of IOP and delay the diagnosis of glaucoma. The IOP has a diurnal fluctuation varying throughout the 24 hours. Therefore some spiking of the IOP may never be detected. According to previous studies, the lowest IOP is usually seen after 2 pm, when some patients visit doctor for their IOP check. The highest is seen at 6 am or in the night, due to the supine position when most of the patients are still in bed.Citation26 Thus, a single office measurement of IOP does not adequately depict the degree of fluctuation in IOP. Some spiking of the IOP is never detected in this case. Even a minor increase in IOP in these elderly patients can cause serious optic nerve damage, especially if it has been going on for a period of time.
We still cannot treat aging and tissue degeneration, but we can aggressively treat these patients to lower IOP to prevent NTG and further loss of sight. Due to the visual field loss from NTG, safety for driving and even walking can be a big issue for these patients. The family or caregivers should be informed of the disability, which most patients may try to deny.
This study was conducted at a single office with a single calibrated ORA for accuracy. A single technician, who has done the test in over 20,000 cases in the past 2 years, performed the test in this study. Maintaining a correct posture and position in front of the machine were strict requirements for a reliable test result. The IOP readings were often compared with Goldmann applanation tonometry for consistency and agreement.
The majority of the participants (90%) of this study were Asian. A possible reason for this high incidence in this practice of seeing patients with undiagnosed NTG could be due to the high Asian population and less attention being paid to this disease. It was rare to see Polynesians in this study population, and most of the patients were pure Chinese, Japanese, Korean, and Philippine immigrants. It may be due to education, economic, or cultural reasons that this population tends to be poorly educated and ignores NTG until an irreversible late stage is reached.
The results of this study confirm multiple other studies that showed that as many as 30%–50% of individuals in the general population who have glaucomatous optic neuropathy and visual field loss have initial screening IOPs below 22 mmHg. As glaucomatous optic neuropathy examination and visual field test can be challenging for elderly patients with NTG, CH can be an add-on diagnostic tool for NTG.
This study suggests considering measuring CH as a screening tool for NTG, especially in patients with risk factors.
Conclusion
CH measurement is a valuable test to assist in early diagnosis of NTG, especially in an elderly Asian population. Once the diagnosis of NTG is made, aggressive medical or surgical treatments to further lower IOP can prevent irreversible blindness, which can severely impact on the patients and their family.
Disclosure
The authors report no conflicts of interest in this work.
References
- BoydKWhat is glaucoma?Am Acad Ophthalmol Epub4282016
- QuigleyHABromanATThe number of people with glaucoma worldwide in 2010 and 2020Br J Ophthalmol20069026226716488940
- WeinrebRNAungTMedeirosFAThe pathophysiology and treatment of glaucoma: a reviewJAMA20143111901191124825645
- TopouzisFColemanALHarrisAFactors associated with undiagnosed open-angle glaucoma: the Thessaloniki Eye StudyAm J Ophthalmol200814532733518045565
- ChuaJBaskaranMOngPGPrevalence, risk factors, and visual features of undiagnosed glaucoma: the Singapore Epidemiology of Eye Diseases StudyJAMA Ophthalmol201513393894626043441
- IwaseASuzukiYAraieMThe prevalence of primary open-angle glaucoma in Japanese: the Tajimi StudyOphthalmology20041111641164815350316
- RamakrishnanRNirmalanPKKrishnadasRGlaucoma in a rural population of southern India: the Aravind comprehensive eye surveyOphthalmology200311081484149012917161
- ChoHKKeeCPopulation-based glaucoma prevalence studies in AsiansSurv Ophthalmol20145943444724837853
- BonomiLMarchiniGMarraffaMPrevalence of glaucoma and Intraocular pressure distribution in a defined population. The Egna-Neumarkt StudyOphthalmology19981052092159479277
- MedeirosFMeira-FreitasDLisboaRCorneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal studyOphthalmology201312081533154023642371
- CongdonNGBromanATBandeen-RocheKCentral corneal thickness and corneal hysteresis associated with glaucoma damageAm J Ophthalmol200614186887516527231
- BochmannFAngGSAzuara-BlancoALower corneal hysteresis in glaucoma patients with acquired pit of the optic nerve (APON)Graefes Arch Clin Exp Ophthalmol200824673573818193259
- Sullivan-MeeMBillingsleySCPatelADOcular response analyzer in subjects with and without glaucomaOptom Vis Sci20088546347018521025
- WellsAPGarway-HeathDFPoostchiACorneal hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patientsInvest Ophthalmol Vis Sci2008493262326818316697
- AbitbolOBoudenJDoanSCorneal hysteresis measured with the ocular response analyzer in normal and glaucomatous eyesActa Ophthalmol20108811611919891669
- AnandADe MoraesCGTengCCCorneal hysteresis and visual field asymmetry in open angle glaucomaInvest Ophthalmol Vis Sci2010516514651820574009
- HirneissCNeubauerASYuACorneal biomechanics measured with the ocular response analyser in patients with unilateral open-angle glaucomaActa Ophthalmol201189e189e19221288308
- NarayanaswamyASuDHBaskaranMComparison of ocular response analyzer parameters in Chinese subjects with primary angle-closure and primary open-angle glaucomaArch Ophthalmol201112942943421482869
- Grise-DulacASaadAAbitbolOAssessment of corneal bio-mechanical properties in normal tension glaucoma and comparison with open-angle glaucoma, ocular hypertension, and normal eyesJ Glaucoma201121486489
- MoritaTShojiNKamiyaKCorneal biomechanical properties in normal-tension glaucomaActa Ophthalmol201190e48e5321914145
- MansouriKLeiteMTWeinrebRNAssociation between corneal biomechanical properties and glaucoma severityAm J Ophthalmol201215341942722018707
- De MoraesCVHillVTelloCLower corneal hysteresis is associated with more rapid glaucomatous visual field progressionJ Glaucoma20122120921321654511
- KaushikSPandavSSBangerARelationship between corneal biomechanical properties, central corneal thickness, and intraocular pressure across the spectrum of glaucomaAm J Ophthalmol201215384084922310080
- PrataTSLimaVCGuedesLMAssociation between corneal bio-mechanical properties and optic nerve head morphology in newly diagnosed glaucoma patientsClin Exp Ophthalmol20124068268822429725
- VuDMSilvaFQHaseltineSJRelationship between corneal hysteresis and optic nerve parameters measured with spectral domain optical coherence tomographyGraefes Arch Clin Exp Ophthalmol20132511777178323519885
- AsraniSZeimerRWilenskyJGieserDVitaleSLindenmuthKLarge diurnal fluctuation in intraocular pressure are an independent risk factor in patients with glaucomaJ Glaucoma20009213414210782622
