Abstract
Background:
Uniform postresidency systems to train medical specialists have not been developed in most European countries. Before developing a framework for such a system, we established the learning and professional profiles of Spanish ophthalmologists dedicated to medical retina and vitreoretina subspecialties.
Methods:
After identification of presumed subspecialists by experts from different autonomous regions, a self-administered questionnaire was mailed in 2006. A reminder was sent three weeks later. Postal mail was used. Nonresponder bias was determined.
Results:
Of 492 possible retina subspecialists, 261 replied to the questionnaires. While about 86% received specific retinal training, standardized fellowship programs were uncommon for both medical retina and vitreoretina (around 10%). Of the responders, 24.5% performed only medical retina, 11.8% vitreoretina, and 63.6% both. Most (60.5%) practiced anterior segment surgery, and 78.7% declared skills in vitrectomy.
Conclusion:
We have developed a database of Spanish ophthalmologists dedicated to retinal pathologies and identified some characteristics of their professional profile. Although most of them have received specific retinal training, standardized mastership programs are still uncommon. These data will be useful in creating a standardized Retina Mastership, an important goal of the European Higher Education Area.
Introduction
While fellowships in ophthalmology were created in the US during the 1970s, similar educational postresidency systems have not been developed or recognized in most Europeans countries. Now, in accordance with the Bologna Declaration (http://ec.europa.eu/education), all member countries of the European Union must institute so-called superior education programs that codify the standards by which advanced postdoctoral or postgraduate training is provided. These standards should fit within the framework of the European Higher Education Area. This program establishes the adoption of a common framework of readable and comparable degrees, the introduction of common standards for undergraduate and postgraduate levels in all countries, and the introduction of a learning credit system, known as the European credit transfer system, covering lifelong learning activities. Of similar importance for the near future is the linkage of the European credit transfer system with the European Research Area (http://ec.europa.eu/research), which encompasses a set of common standards and expectations for research conducted by members of the European Union. These actions open new possibilities for the standardization and enhancement of professional teaching programs. The goal of these changes is to attain complete educational and employment mobility of European citizens across the Union. These attempts of standardization should be in accordance with similar ones developed in North America.Citation1
Spain established the National Residency System in 1980 with a standardized admission examination for medical specialty programs. It also developed national guidelines for all medical specialties, including ophthalmology. Thus, a standardized system with common minimum requirements exists for teaching general ophthalmologists throughout the country. However, the way in which ophthalmologists are trained in the different subspecialties is neither standardized nor officially recognized by the Spanish National Health System. Nevertheless, Spanish ophthalmology has moved forward, and several ophthalmic subspecialty societies have been created. One is the Vitreo-Retina Society, founded in 1996.
This study is part of the Retina 2 Project, which started in 2005 with the aim of assessing the current management of retinal detachment in Spain.Citation2–Citation4 The first approach revealed a lack of information related to the profile of ophthalmologists dedicated to retinal diseases in Spain. The absence of a regulated training system to achieve the subspecialty was also evident. Therefore, we performed a national survey to identify ophthalmologists who specialize in retinal disease, to find out how they obtained their specific training in retina, and to learn the characteristics of their professional profile. This information is necessary to define the contents of a future fellowship training program in retina.
Methods and materials
The project was approved by the Research Committee of the University Institute of Applied Ophthalmobiology (IOBA) at the University of Valladolid in Spain. Under the auspices and with the approval of the Spanish Vitreo-Retina Society and the Spanish Ophthalmological Society, lists of the members of both societies were assembled. Experienced ophthalmologists at the University Institute of Applied Ophthalmology identified three very well-known and experienced ophthalmologists dedicated to the retina for each of the 17 autonomous regions of Spain, to whom the lists were sent. These leading ophthalmologists were asked to identify other regional ophthalmologists who dedicated a significant part of his/her practice to treating retinal diseases. For the purposes of this study, those ophthalmologists who were dedicated preferentially to treating diseases of the retina were defined as retinologists.
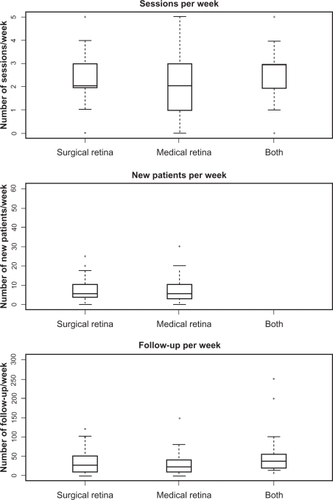
With this information, a database was created that included 492 probable retinologists from the total population of Spanish ophthalmologists, estimated at more than 4400. A self-administered questionnaire with 29 questions was created regarding the characteristics of their current work center, training process, length of subspecialization, clinical activity (including surgery), and involvement in research and continued medical education programs (). The questionnaire was evaluated by nine experienced retinologists and nonretinologists from the IOBA in a piloting phase. It was then posted to the 492 probable retinologists at the end of 2006 and beginning of 2007. Three weeks later, a reminder was sent to those who had not replied. Postal mail was always used.
Figure 1 Questionnaire sent to 492 ophthalmologists. In order to know the nonresponse bias, a new shorter questionnaire was sent to a new sample (only gray questions).
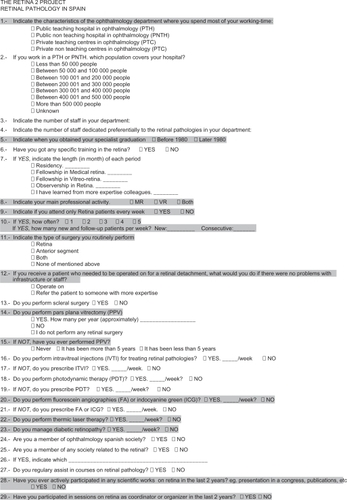
With a global response of 53.1% after two reminders, we determined the so-called “nonresponder bias”. Information from the primary responders’ answers was used to identify a reduced number of survey items. These “key items” were used to derive a new smaller questionnaire. This form was sent to nonresponders by using the commercial network of a vitreoretinal instruments company which has a national coverage. Those who responded to this second questionnaire were termed “secondary responders”. From these selected clusters, bias was calculated by comparing data from the primary responders with those from the secondary responders.Citation5,Citation6
For ophthalmologists declared to be retinologists, we sought to determine their activity level in this subspecialty based upon the total number of sessions per week and the number of new and returning patients seen each week. Quantitative variables were summarized by means ± standard deviations. When the values were not equally distributed along the whole range of a variable, the median was used. Percentages were used with qualitative variables. The relationships between categorical variables were evaluated by bivariate crosstabulation. Statistical significance was estimated by the Chi-squared test. When the use of this test was not possible, the Fisher’s Exact test was employed. The Mann–Whitney U test was used to compare independent groups. When there were more than two groups, the Kruskal–Wallis test was used. Multiple comparisons were adjusted by Bonferroni correction. Categorical principal components, multiple correspondence, and factor analysis were used for data reduction to examine the underlying relationships among multiple variables. The statistical analysis was performed using SPSS version 15.0 for Windows (SPSS Inc, Chicago, IL). P values ≤ 0.05 were regarded as statistically significant.
Results
All primary responders (261 ophthalmologists) were identified as retinologists. The sample for estimating the nonresponse bias was made up of 132 ophthalmologists, comprising 96 primary responders and 36 secondary responders (). There were no differences between primary and secondary responders except for those performing fluorescein angiography. Secondary responders personally performed fluorescein angiography less frequently than did primary responders.
Figure 2 Samples and methods used for creation of a database and evaluation of nonresponse bias. Thirty-six nonresponders to the initial survey did respond to the second survey and were referred to as “secondary responders”.
The majority of the primary responders (83.5%) worked at hospitals in the National Health System, and only 16.5% worked in private institutions. Most of the hospitals (67.3%) were public teaching hospitals. Of those, 70% had coverage of greater than 300,000 inhabitants.
Number of ophthalmologists and retinologists by working center
In public hospitals, there were more ophthalmologists and retinologists in teaching hospitals than in nonteaching hospitals. The average number of ophthalmologists on staff at public teaching hospitals was 16.5 (). Of these, 4.5 were retinologists. For private teaching centers, there were 30.6 ophthalmologists and 5.0 retinologists, which was also greater than at private nonteaching centers (). For the teaching institutions, there were no differences between public and private centers regarding the number of ophthalmologists and retinologists.
Table 1 Number of estimated ophthalmologists and retinologists and types of working centers
Specialization and training periods
Among ophthalmologists who got their certificate before 1980, 67.5% participated in a specific training period for retinal diseases after their residency (). After 1980, only 36.3% took postresident training. In contrast, of the 82.4% who earned the ophthalmology certificate after 1980, when the National Residency System was implemented, almost 95% received specific training in retinal diseases (). Of that group, 87.3% were trained during their residency. Specific masterships in medical retina or in vitreoretina were less common among those ophthalmologists that attained the certificate after 1980. Around 70% of ophthalmologists, before and after 1980, were trained in retina by more experienced colleagues.
Table 2 Affirmative responses regarding specific training in retinal diseases
The length of the different training periods were variable. During residency, the median time dedicated to retina was 12 (range 1–60) months. Those who undertook masterships were trained for a median of 12 (0.5–24) months. Observership periods were not regulated and lasted a median of three (0.5–36) months. Training by more experienced colleagues lasted a median of 12 (1–120) months. All retinologists working in private centers had specific retinal training, while 91.3% of those working at public teaching hospitals and 94.6% at private nonteaching centers had this training. The differences between private and public facilities were not statistically significant.
Professional activity
Most retinologists (63.6%) provided both medical retina and vitreoretina services. The majority of responders (60.5%) also performed anterior segment surgery. Scleral surgery and pars plana vitrectomy were performed by 69.1% and 78.8% of retinologists, respectively, and only 18.4% referred patients who suffered from a retinal detachment to another surgeon. Almost 12% of retinologists declared that they did not currently perform pars plana vitrectomy, and 9.3% had never performed one. In addition to major surgery, most retinologists, even those dedicated exclusively to medical retina, performed various minor procedures, such as intravitreal injections, photodynamic therapy, fluorescein angiography, and laser ().
Table 3 Detailed characteristics of professional activity declared by retinologists
Differences among retinologists
While 24.5% of retinologists were dedicated mainly to medical retina, 11.9% were dedicated only to vitreoretina. All of the retinologists who did not perform any surgical procedures were dedicated to medical retina (). While 54.7% of medical retina retinologists performed anterior segment surgeries, none of the vitreoretina retinologists did so. Only 1.2% of the retinologists who specialized in both medical retina and vitreoretina did anterior segment surgeries ().
Most of the medical retina specialists (64.5%) preferentially referred retinal detachment patients to other retinologists. This was greater compared with vitreoretina specialists and those who dedicated to both practices (3.3% and 3.7%, respectively). Most medical retina specialists did not perform scleral surgery (55.0%), never performed a pars plana vitrectomy (33.9%), and only 22.6% currently perform pars plana vitrectomy ().
Level of patient activity
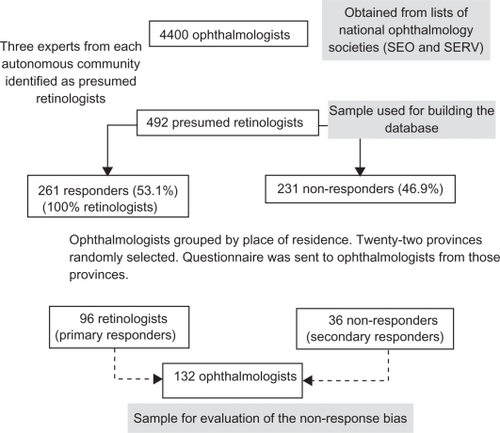
The level of patient activity was greater among retinologists who provided both medical retina and vitreoretina. They had more sessions per week and more new and follow-up patients (). Also, private centers had higher patient activity levels than public hospitals.
Other clinical characteristics
Ninety percent of the responders were members of the Spanish Ophthalmological Society, and 52.8% belonged to at least one retina society. Of the responding retinologists, 91.2% periodically attended retinal courses, 66.8% participated in research and preparation of scientific papers on retinal diseases, and 57.1% never participated in teaching courses on this subject.
Discussion
There are some limitations in this work. First, there is no official registry of retinologists in Spain. The initial list of ophthalmologists for this study was obtained from two scientific societies. Not all ophthalmologists working in Spain are members of these societies, although probably more than 80% belong to the Spanish Ophthalmological Society, and it is very difficult to obtain data from nonmembers.
Another important limitation is that all retinologists were identified by other experienced colleagues. These reference retinologists were carefully selected among the most outstanding retina forum. All of them have a vast experience, continuously participate in teaching activities, and are recognized as second-opinion leaders. That could guarantee an adequate knowledge of his/her colleagues’ professional activities. On the other hand, all the autonomous regions of Spain are represented by at least three retinologists. Despite that, we are aware that some practicing retinologists may not have been recognized in this manner, and some who were included may have actually been dedicated to another specialty. However, none of responders were identified as not being dedicated to the retina. Finally, the number of estimated retinologists in Spain represents approximately 10% of ophthalmologists. This rate is similar to that in the US, where 10.5% of ophthalmologists declare themselves as specialized in the treatment of vitreoretina diseases.Citation7
The other limitation is the type of survey used. Typically, self-administered questionnaires have a low rate of response, that might overestimate the answers. This strategy was chosen, however, because of the kind of information required. In order to avoid misinterpretations, questions were mostly closed. The quality and reliability of the questions used were evaluated during the pilot phase. Also, the general data collected here regarding the profile of centers where retinologists perform their task verified the data obtained from the first questionnaire of the Retina 2 Project in 2005.Citation2,Citation3 This concordance of data reinforces the validity of information obtained from this questionnaire. Notwithstanding the limitations of this questionnaire, we consider that nonresponse and any recall bias do not invalidate our results.
A significant percentage of ophthalmologists in Spain are dedicated to the care of vitreoretina diseases, emphasizing the importance of this subspecialty. Most of the responses came from ophthalmologists who obtained their certificates after 1980. This means that they followed a regular and standardized residency program that mandated a specific training period on a retina unit. However, a small percentage of these ophthalmologists (7%) declared that they did not have a specific retinal rotation during their residency.
Implementation of the National Residency System in 1980 has had a definitive influence on the profile of retinologists. This probably explains why a specific postresidency training period in retina is more often found among those specialists who gained their certificate before 1980. Unfortunately, specific fellowships or masterships were not very common among ophthalmologists, and most received training from more experienced colleagues. These data contrast with the situation in other countries. In the US, 64% of residents in ophthalmology choose a subspecialty. Among these, retina (35.6%) and cornea and external diseases (25.2%) are the most frequently selected.Citation8 Similar data are available from Canada.Citation9 There are a variety of opinions on the necessity of certain degree fellowships after the residency period, that must be regulated and standardized.Citation1 This extraresidency training period seems crucial for those who want to orient their subspecialty towards retinal surgery.Citation10
The length of the specific training period was also highly variable. The complexity of diagnostic tools and treatments has increased in recent decades, necessitating longer periods of training. There are now many surgical approaches to treating the same disease. The retinal surgeon must develop skills with these different approaches and understand the nuances of each case so that he/she can choose the best surgery that will yield optimal results.Citation11 Clearly, the time, goals, requirements, and other issues, such as minimum number of new patients, number of surgeries, number of ancillary tests, number of minor nonsurgical treatments, number of grand rounds, scientific sessions, and equipment related to the training period should be regulated. Thus, the official recognition of a Spanish Mastership in Retina, with standardized minimum requirements, is one of the objectives of the Spanish Vitreo-Retina Society for the immediate future.
With regard to continuing education after their specific training in retinology, a high percentage of retinologists (91.2%) regularly attended courses on retinal diseases. Of these, only almost half were members of any scientific society related to the retina. Perhaps many retinologists do not realize that, among the benefits of society membership, is the opportunity for continued education in their specialty.
Other data obtained from this questionnaire are interesting. With regard to the clinical activity profile, most retinologists were dedicated simultaneously to medical retina and vitreoretina diseases. While only 11.9% of the retinologists fully concentrated on managing vitreoretina patients, most practices included anterior segment surgery. Most retinologists (64.5%) dedicated to medical retina alone would refer a patient with a retinal detachment, a practice documented in only 4% of the retinologists dedicated to both medical retina and vitreoretina. It is also very interesting that even while practicing pars plana vitrectomy, almost 23% of retinologists described themselves as dedicated to medical retina. This is consistent with almost 30% of medical retina practitioners who do not refer retinal detachment patients. Surprisingly, there are no data available on the profile of activity of retinologists elsewhere, including in the UK or US.
Almost 80% of retinologists operated on retinal detachments, and a similar percentage performed pars plana vitrectomy. Data for intravitreal injection and photodynamic therapy probably do not reflect the current situation for these treatments, because the questionnaire was completed by the beginning of 2007. Soon afterwards, new antiangiogenic factors became available on the Spanish market. Thus, there is likely to have been a decrease in photodynamic therapy procedures and an increase in the number of intravitreal injections performed since the time of this survey.
In conclusion, we have identified a relevant group of retinologists working in Spain. We also have a clearer idea about the training process of these ophthalmologists and their clinical and surgical activity. All these data are relevant for attempting to create a standardized Retina Mastership, an important goal for the Spanish Vitreo-Retina Society, that will be proposed in accordance with the European Higher Education Area. These results will be presented at the National Ministry of Health of Spain, the Spanish Vitre-Retina Society, and the Euretina Society.
Acknowledgements
The Spanish Ophthalmological Society, Spanish Vitreo-Retina Society, and Bausch and Lomb, Spain, supported this work.
Disclosure
The authors report no conflicts of interest in this work.
References
- KeltnerJLFineSLAbramsGWMondinoBSubspecialty fellowships: Standardizing and enhancing the educational experienceOphthalmology20071144628.e1e317320965
- FernándezIRojasJPastorJCGómezUlla FPiñeroANational enquiry on vítreo-retinal surgery and management of rhegmatogenous retinal detachments in Spain. Retina 2 projectArch Soc Esp Oftalmol20068111635640 Spanish.17136636
- RojasJFernándezIPastorJCGómezUlla FPiñeroAManagement of the urgent rhegmatogenous retinal detachments by the National Health System of Spain. Retina 2 projectArch Soc Esp Oftalmol2007825279284 Spanish.17516264
- PastorJCFernándezIBarragánSTraining and clinical activity of Spanish retinologists: A preliminary approach. Retina 2 project. Descriptive analysisArch Soc Esp Oftalmol20098427583 Spanish.19253177
- RidoutMSDemetrioCGFirthDEstimating intraclass correlation for binary dataBiometrics199955113714811318148
- UkoumunneOCA comparison of confidence interval methods for the intraclass correlation coefficient in cluster randomized trialsStat Med200221243757377412483765
- KoGJBrownMMBrownGCThe macroeconomics of vitreoretinal diseasesCurr Opin Ophthalmol200516318419015870577
- GeddeSJBudenzDLHaftPTielschJMLeeYQuigleyHAFactors influencing career choices among graduating ophthalmology residentsOphthalmology200511271247125415921748
- NobleJSchendelSDanielSBaerlocherMOMotivation and future trends: A survey of Canadian ophthalmology residentsCan J Ophthalmol200742682182517985002
- ParkeDWShould postresidency fellowship mandatory?Arch Ophthalmol1990108137392297330
- Rodríguez de la RúaEPastorJCFernandezINon-complicated retinal detachment management: Variations in 4 years. Retina 1 project; report 1Br J Ophthalmol200892452352518211938