Abstract
Objective:
The aim of this study was to compare the efficacy of augmenting trabeculectomy with subconjunctival mitomycin C (TMMC) versus 5-fluorouracil (T5-FU) in lowering intraocular pressure (IOP).
Methods:
Forty eyes from 40 patients referred to the Nikoukari Ophthalmology University Hospital, Tabriz University of Medical Sciences, Tabriz, Iran, were enrolled in a randomized clinical trial. Patients with high-risk open angle glaucoma were allocated to receive either subconjunctival TMMC or T5-FU.
Results:
Mean overall preoperative IOP was 30.8 mmHg. Mean preoperative IOPs in the TMMC and T5-FU groups were 31.2 ± 9.8 and 30.6 ± 9.9 mmHg, respectively. Postoperatively, mean IOPs were 11.4.3 ± 4.9 and 13.6 ± 3.9 mmHg, respectively for TMMC and T5-FU groups after 6 months. In spite of some existing descriptive differences in IOP between the groups, statistical tests showed no difference in mean and median IOP. Three cases of hypotonia (IOP < 6 mmHg) and 1 case of epithelial keratitis were detected.
Conclusion:
TMMC and T5-FU appeared to have similar efficacy in lowering IOP.
Introduction
Trabeculectomy aims to decrease intraocular pressure (IOP) by allowing the passage of aqueous humor from the anterior chamber to the subconjunctival space. The main reason for failure of filtering surgery is fibroblast proliferation and subsequent scar formation at the surgical site. Recent ongoing research has found some remedies to prevent this, and improve surgical success by inhibiting scar formation. Antimetabolites, including mitomycin C (MMC) and 5-fluorouracil (5-FU), were first used to modify the wound-healing response in the early 1980s. Although an optimum therapy with good efficacy and low complication rate is not yet available, MMC and 5-FU are currently used for this purpose. MMC is an antimetabolite used during the initial stages of a trabeculectomy to prevent excessive postoperative scarring and thus reduce the risk of failure.Citation1 Similarly 5-FU can be used for the same purpose.Citation2 MMC and 5-FU are typically used in eyes at high risk for bleb failure, and are used by researchers and clinicians as adjuncts to trabeculcetomy surgery (herein, TMMC and T5-FU), but using different protocols and dosages. Most of the evidence on efficacy of TMMC and T5-FU is based on studies conducted separately for these two protocols rather than comparative randomized trials of TMMC and T5-FU. In spite of large numbers of studies conducted in this area, very few randomized clinical trials have compared MMC and 5-FU in a parallel design, and those available did not compare subconjunctival forms of both drugs. The aim of this study was to compare the efficacy of TMMC with T5-FU in lowering IOP in high-risk glaucoma patients.
Methods
A randomized clinical trial study was conducted in the Nikoukari Ophthalmology University Hospital, Tabriz, Iran. Forty eyes from 40 patients were enrolled. Using simple randomization in a parallel trial design, 18 patients were randomly assigned to receive TMMC and 22 to receive T5-FU. In the TMMC group, MMC was injected subconjunctively at a dose of 0.02 mg via an 0.4 mm*20 mm needle 180 degrees from the operating site. Likewise, 5-FU was injected into subconjunctively at a dose of 5 mg. The inclusion criteria for this study were: 1) open angle glaucoma; 2) uncontrolled IOP; 3) optic nerve damage and visual field restriction. Patients were then followed up for measurement of IOP and development of possible complications. IOP was measured using the Goldmann applanation tonometer (Haag-Streit, Bern, Switzerland) on 5 occasions: at baseline, 2 weeks, 1 month, 3 months, and 6 months afterwards.
The primary endpoint of the study was successful augmented surgery, defined as a consistent IOP between 6 mmHg and 22 mmHg towards the end of the evaluation period.
Data were analyzed using STATA version 11 statistical software package. Trends in IOP and IOP distributions were compared descriptively over the 6-month study. The primary endpoint was compared between the trial groups. Relative risk of treatment success for TMMC compared with T5-FU was calculated along with 95% confidence intervals (CI). Mean and median tests were also used to compare IOP between groups. Kaplan–Meier curves and survival function tests were used to assess the effect of treatment on time to success. To control possible random disproportions in some background confounders, a Cox regression model was used. All the statistical tests were interpreted on a 2-tailed basis. The test results with a P-value < 0.05 were considered as statistically significant. The study protocol was approved by the ethics committee of Tabriz University of Medical Sciences.
Results
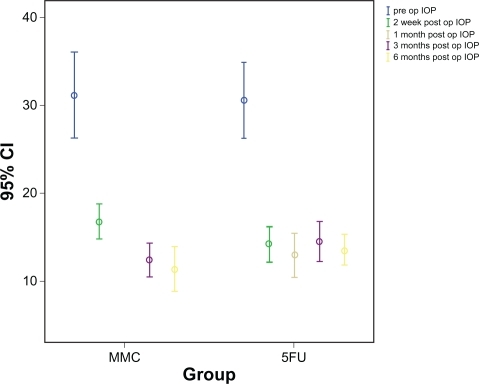
Men comprise 81% of the participants. Mean age was 67.5 years (standard deviation 10 years). The youngest subject was 48 years old and the oldest was 83 years old. Mean preoperative IOP was 30.85 mmHg. Mean preoperative IOPs in the TMMC and T5-FU groups were 31.2 ± 9.8 and 30.6 ± 9.9 mmHg, respectively. Postoperatively, mean IOPs were 11.4.3 ± 4.9 and 13.6 ± 3.9 mmHg, respectively, for TMMC and T5-FU after 6 months. shows that average IOP in both groups began to decrease sharply during the first 2 weeks, then leveled off in the T5-FU group but continued to decrease slowly in the TMMC group.
Figure 1 Error bar graph (95% confidence intervals of standard errors) comparing intraocular pressure (IOP) after trabeculectomy augmented with subconjunctival mitomycin C (TMMC) versus 5-fluorouracil (T5-FU).
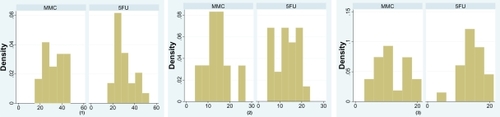
A similar pattern of steeper IOP improvement trend was also found for the TMMC group when quartiles instead of means were compared. The distribution of IOP in the TMMC group changed from left-skewed to nearly-normal after 6 months ().
Figure 2 Intraocular pressure (IOP) measured at baseline (1), 1 month (2), and 6 months (3) after surgery.
Abbreviations: TMMC, trabeculectomy augmented with subconjunctival mitomycin C; T5-FU, trabeculectomy augmented with 5-fluorouracil.
In spite of some existing descriptive differences in IOP between the groups, statistical tests showed no difference in mean and median IOP. For the primary endpoint (consistent IOP between 6 mmHg and 22 mmHg towards the end of the evaluation period), treatment was successful in 88.9% and 92.5% of subjects in TMMC and T5-FU groups, respectively. Two patients in the TMMC group and 1 patient in the T5-FU group did not have a successful outcome during the 6 months of follow-up: IOP in these 3 patients dropped to <6 mmHg, which was regarded unsuccessful. The relative risk of success for TMMC compared with T5-FU was 0.93 (95% CI: 0.8–1.1).
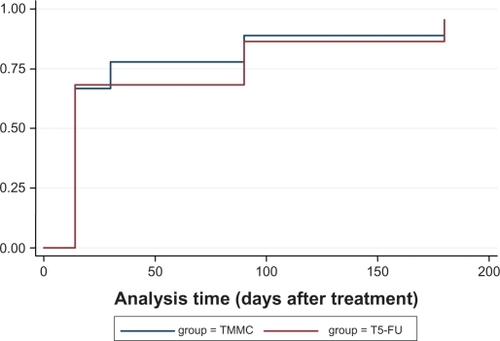
Testing the survival functions of successful treatment did not show any statistically significant differences between the groups ().
Figure 3 Kaplan–Meier curves comparing success rate of TMMC and T5-FU.
The Cox regression model did not help to detect possible differences in efficacy between groups. Three cases of hypotonia (IOP < 6 mmHg) and 1 case of epithelial keratitis were observed. No differences were detected between the groups.
Discussion
Most of the evidence on efficacy of TMMC and T5-FU is based on studies conducted separately for these two protocols rather than comparative randomized trials. A recent review enrolled 11 placebo-controlled studies for MMC and concluded that MMC appears to reduce the relative risk of failure of trabeculectomy both in eyes at high risk of failure (relative risk 0.32, 95% CI: 0.20–0.53) and those undergoing surgery for the first time (relative risk 0.29, 95% CI: 0.16–0.53).Citation1 Another systematic review partly by the same authors conducted earlier suggested that injection of low doses of 5-FU may not be effective.Citation2 The before–after assessment of the effect of TMMC or T5-FU was quite obvious in our study although was not an objective of the study.
It is clear from published results that treatment protocols for augmented trabeculectomy vary widely, for example, in form of drug application (ie, injection vs sponge), application-injection site, timing, frequency, and dosage. This variation is doubled when two drugs are compared in a clinical trial. Our study was a randomized clinical trial study comparing TMMC and T5-FU. We retrieved 10 articles that compared the two methods either in an observational study or in a parallel clinical trial design.Citation3–Citation12 compares the methodology of these studies.
Table 1 Comparison of methods in observational and clinical trial studies comparing TMMC with T5-FU
The drugs were administered intraoperatively in most of these studies using soaked sponges. A few also used subconjunctival injection of 5-FU. Dosage and timing also differed among these studies. Nevertheless, as in our study, nearly all of these studies failed to detect statistically significant differences in success or development of complications between TMMC and T5-FU. One study found borderline statistical significance for lower mean IOP in TMMC than T5-FU.Citation9 As in our study, some of these studies stated a descriptively higher success rate for TMMC. Our study results were consistent throughout different assessment methods such as comparing means, medians, quartiles, distribution patterns, and survival methods. Most of these studies tried to test the differences between groups in complications but found no difference. However, these studies’ power limits seem to be too low to enable differences in complication rates to be detected between groups. Register-based cohorts in high-income countries that have reliable patient registry databases could be a better way of answering this question. In addition case-control studies can also be a valuable way of investigating this issue in countries lacking reliable databases.
The IOP decrement pattern in our study seemed to be more transient for T5-FU than for TMMC. Khaw et al found similar results in an animal study.Citation13
Our survival analysis using Kaplan–Meier survival comparison and survival function tests did not show a significantly longer time for TMMC to achieve success. Among the studies discussed above, Palanca-Capistrano et al found similar results as ours when using the Kaplan–Meier and survival function tests to compare TMMC and T5-FU.Citation6 Several factors are known to affect IOP, among which are corneal parameters such as corneal curvature. It is obligatory in observational studies to measure and control these parameters. Considering the effect of randomization in clinical trials, the distribution of known and unknown confounders will be random; however, it is preferable to measure these parameters, even in randomized trials.
Based on our findings and available knowledge, it appears that TMMC and T5-FU have similar efficacy in augmenting trabeculectomy. However, considering the greater, but nonsignificant, efficacy of TMMC in some studies, including ours, future larger-scale clinical trials comparing the two methods may be able to detect a significant difference. Use of subconjunctival injections of MMC and 5-FU may be recommended also because of easier methodology and possibly less procedural variation.
Disclosure
The author discloses no conflicts of interest.
References
- WilkinsMIndarAWormaldRIntra-operative mitomycin C for glaucoma surgeryCochrane Database Syst Rev20054CD00289716235305
- WormaldRWilkinsMRBunceCPost-operative 5-fluorouracil for glaucoma surgeryCochrane Database Syst Rev20013CD00113211686977
- BadeebOTrabeculectomy with mitomycin C versus rabeculectomy with 5-fluorouracil for treatment of childhood glaucomaOman Journal of Ophthalmology200811712
- KimHYEgbertPRSinghKLong-term comparison of primary trabeculectomy with 5-fluorouracil versus mitomycin C in West AfricaJ Glaucoma200817757858318854737
- KitazawaYKawaseKMatsushitaHMinobeMTrabeculectomy with mitomycin. A comparative study with fluorouracilArch Ophthalmol199110912169316981841578
- Palanca-CapistranoAMHallJCantorLBMorganLHoopJWuDunnDLong-term outcomes of intraoperative 5-fluorouracil versus intraoperative mitomycin C in primary trabeculectomy surgeryOphthalmology2009116218519018930550
- Prata JuniorJAMincklerDSBaerveldtGLeePPLaBreeLHeuerDKTrabeculectomy in pseudophakic patients: postoperative 5-fluorouracil versus intraoperative mitomycin C antiproliferative therapyOphthalmic Surg199526173777746631
- PrataJAJrSeahSKMincklerDSBaerveldtGLeePPHeuerDKPostoperative complications and short-term outcome after 5-fluorouracil or mitomycin-C trabeculectomyJ Glaucoma199541253119920633
- SinghKEgbertPRByrdSBudenzDLWilliamsASDeckerJHTrabeculectomy with intraoperative 5-fluorouracil vs mitomycin CAm J Ophthalmol1997123148539186096
- SinghKMehtaKShaikhNMTsaiJCMosterMRBudenzDLTrabeculectomy with intraoperative mitomycin C versus 5-fluorouracil. Prospective randomized clinical trialOphthalmology2000107122305230911097613
- SmithMFDoyleJWNguyenQHSherwoodMBResults of intraoperative 5-fluorouracil or lower dose mitomycin-C administration on initial trabeculectomy surgeryJ Glaucoma1997621041109098818
- WuDunnDCantorLBPalanca-CapistranoAMHoopJAlviNPFinleyCA prospective randomized trial comparing intraoperative 5-fluorouracil vs mitomycin C in primary trabeculectomyAm J Ophthalmol2002134452152812383808
- KhawPTDoyleJWSherwoodMBSmithMFMcGorraySEffects of intraoperative 5-fluorouracil or mitomycin C on glaucoma filtration surgery in the rabbitOphthalmology199310033673728460007