Abstract
Purpose:
To determine how culture results are associated with clinical presentations and outcomes in delayed-onset bleb-associated endophthalmitis (BAE).
Methods:
Retrospective consecutive case series of BAE at Bascom Palmer Eye Institute between January 1, 1996 and December 31, 2009. All patients had prior glaucoma filtering surgery. BAE was defined as intraocular infection with vitreous involvement receiving treatment with intravitreal antibiotics. Visual acuity (VA) outcomes and other clinical data were grouped by culture result and compared using the 2-sided Student’s t-test.
Main outcome measure:
Mean logMAR change at 3 months after treatment (3-month logMARΔ).
Results:
Eighty-six eyes of 85 patients were identified. Two eyes were primarily eviscerated. Fifty-three (63%) eyes were culture-positive with the following organisms: Streptococcus, 21 (25%); coagulase-negative Staphylococcus, 9 (11%); Enterococcus, 6 (7%); Gram-negative, 15 (18%); Moraxella, 8 (10%); Pseudomonas, 3 (4%); and Serratia, 3 (4%). Presenting logMAR VA: culture-positive worse than culture-negative cases (2.45 vs 2.19, P = 0.05). Presenting intraocular pressure (IOP): culture-positive higher than culture-negative cases (24 mmHg vs 14 mmHg, P = 0.002). Poor presenting view of the fundus: Streptococcus worse than coagulase-negative Staphylococcus cases (90% vs 44%, P = 0.006), Pseudomonas and Serratia worse than Moraxella cases (100% vs 50%, P = 0.04). Three month logMARΔ: culture-positive worse than culture-negative cases (1.03 vs 0.43, P = 0.02), Streptococcus worse than coagulase-negative Staphylococcus cases (1.44 vs 0.31, P = 0.004), Pseudomonas and Serratia worse than coagulase-negative Staphylococcus cases (2.41 vs 0.31, P = 0.001), Pseudomonas and Serratia worse than Moraxella cases (2.41 vs 0.04, P = 0.001). A culture result of Streptococcus or Serratia was present in 6 of 7 eyes that received an additional treatment of enucleation or evisceration (P = 0.01).
Conclusion:
Culture-positive cases were associated with worse presenting VA, higher presenting IOP, and worse VA outcomes than culture-negative cases. Streptococcus, Pseudomonas, and Serratia cases were associated with poor presenting view of the fundus and worse VA outcomes than coagulase-negative Staphylococcus and Moraxella cases.
Introduction
Visual acuity (VA) outcomes after treatment of delayed-onset bleb-associated endophthalmitis (BAE) are poor.Citation1–Citation10 Only 22%–67% of eyes with BAE achieve a VA outcome of 20/400 or better. The most frequent causative organisms isolated include Streptococcus sp. and Gram-negative organisms in 31%–57% and 15%–32% of cases, respectively.Citation1–Citation6
The association between culture results and VA outcomes has been addressed in small case series.Citation1–Citation6 In one study there was no significant difference between VA outcomes of eyes with Streptococcus sp., non-Streptococcus Gram-positive organisms, and Gram-negative organisms.Citation2 Another study showed no significant difference between VA outcomes of eyes with Streptococcus and Staphylococcus sp.Citation3 Others reported VA outcomes for eyes with Streptococcus sp. and non-Streptococcus organisms but did not perform a comparative analysis.Citation4–Citation6 The inability to identify a significant association between VA outcomes and culture result may be due to the relatively small number of reported BAE cases and the pre-existing ocular disease in these patients.
It is also unclear if the clinical presentation of BAE differs by culture result. Presently no studies have reported presenting clinical information (eg, intraocular pressure, presence of hypopyon, view of the fundus) by culture result. The purpose of the current study is to determine how culture results are associated with clinical presentations and outcomes in BAE by performing a comparative analysis within a large case series.
Methods
The study protocol was approved by the Institutional Review Board of the University of Miami Miller School of Medicine Subcommittee for the Protection of Human Subjects in Research. The medical records and microbiologic records of all patients treated for BAE at Bascom Palmer Eye Institute (BPEI) between January 1, 1996 and December 31, 2009 were reviewed. All patients had prior glaucoma filtering surgery. BAE was defined as intraocular infection with vitreous involvement receiving treatment with intravitreal antibiotics. Patients with tube shunts as the filtering mechanism, bleb infection only (no posterior inflammation), onset within 1 month of glaucoma surgery, and inadvertent filtering blebs after cataract surgery were excluded. Clinical history and presentation, treatment, intraocular culture data, VA outcomes, and factors affecting VA were recorded. The current study included clinical information from the series of 71 eyes treated at BPEI between January 1, 1996 and July 1, 2008, which has been reported previously.Citation1
Snellen VAs were converted to logMAR equivalents for statistical analysis; VAs of hand motion, light perception, and no light perception were assigned logMAR values of 2.6, 3, and 4 respectively. Change in VA was determined by comparing the last recorded VA before the onset of endophthalmitis with VA at 3 months. The mean logMAR change at 3 months after presentation (3-month logMARΔ) and other clinical data were grouped by culture result and compared using the 2-sided Student’s t-test. A P-value of ≤0.05 was considered statistically significant.
Results
Eighty-six eyes of 85 patients were identified. Two eyes were primarily eviscerated. Intraocular culture results were positive in 53 of 84 eyes, 63% Streptococcus sp. and Gram-negative organisms were the most frequent isolates, accounting for 25% and 18% of cases respectively. In five eyes, two organisms were isolated. All isolated organisms were sensitive to the intravitreal antibiotics clinically administered which included Vancomycin and Ceftazidime in 77 eyes, 92%, Vancomycin and Amikacin in two eyes, Vancomycin and Gentamicin in one eye, Vancomycin alone in two eyes, Ceftazidime and Amikacin in one eye, and Cefazolin and Gentamicin in one eye. Intravitreal Dexamethasone injections were given to 69 eyes, 82%. All eyes received topical antibiotics and steroids.
A comparison of culture-positive and culture-negative cases showed no significant difference in baseline demographics (). A greater number of culture-positive cases presented with a poor view of the fundus. The mean presenting intraocular pressure (IOP) was higher in culture-positive cases with no significant difference in final IOP. The mean pre-endophthalmitis VA showed no significant difference between groups, however mean presenting VA and 3-month logMARΔ were worse in culture-positive cases ( and ).
Figure 1 Photograph of right eye of 66-year-old male presenting with BAE from Streptococcus sp. Presenting VA: HM, IOP: 28 mmHg. Treatment: tap and injection. Final VA: HM, IOP: 12 mmHg. Culture-positive cases were associated with worse presenting VA and higher presenting IOP than culture-negative cases.
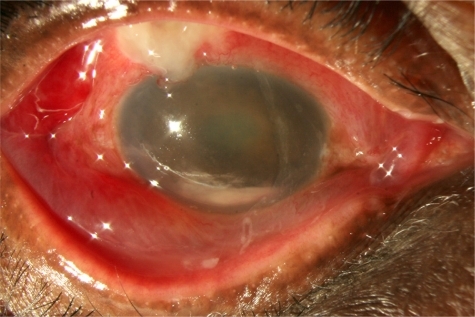
Figure 2 Photograph of left eye of 67-year-old male presenting with culture-negative BAE. Presenting VA: 20/200, IOP: 10 mmHg. Treatment: tap and injection. Final VA 20/200, IOP 16 mmHg. Culture-negative cases were associated with better VA outcomes than culture-positive cases.
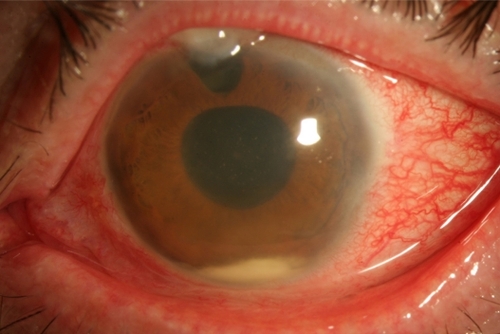
Table 1 Culture-positive and culture-negative cases
Comparing Streptococcus cases with non-Streptococcus Gram-positive and coagulase-negative Staphylococcus cases showed no significant difference in baseline demographics (). The Streptococcus cases presented with a higher mean IOP and greater number of cases with a poor view of the fundus. A higher number of coagulase-negative Staphylococcus cases received tap and injection as the initial treatment. There was no significant difference in mean pre-endophthalmitis VA or presenting VA, however 3-month logMARΔ was significantly worse in Streptococcus cases ().
Figure 3 Photograph of left eye of 79-year-old female presenting with BAE from Streptococcus sp. Presenting VA: LP, IOP: 40 mmHg. Treatment: pars plana vitrectomy. Final VA: LP, IOP: 0 mmHg. Only 45% of Streptococcus cases had VA outcomes ≥ 20/400.
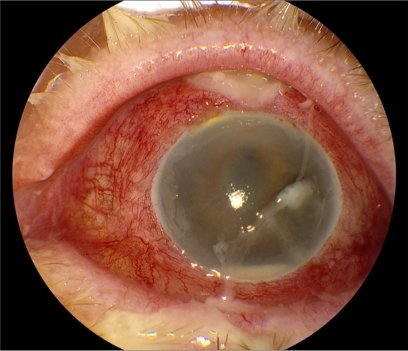
Table 2 Gram-positive cases
A comparison of Gram-negative cases with coagulase-negative Staphylococcus cases showed that fewer Gram-negative cases achieved VA ≥20/400 at 3 months (). Pseudomonas and Serratia cases were associated with a poor view of the fundus, higher mean presenting IOP, and a worse 3-month logMARΔ compared with coagulase-negative Staphylococcus cases. Pseudomonas and Serratia cases were also associated with a poor view of the fundus and worse 3-month logMARΔ compared to Moraxella cases ().
Figure 4 Photograph of left eye of 72-year-old female with BAE from Moraxella sp. Presenting VA: 1/200, IOP: 35 mmHg. Treatment: tap and injection. Final VA: 20/25, IOP: 11 mmHg. Moraxella cases were associated with a better presenting view of the fundus and better VA outcomes than Pseudomonas and Serratia cases.

Table 3 Gram-negative cases
Streptococcus and Serratia cases were associated with enucleation or evisceration (). Six of seven eyes that received an additional treatment of enucleation or evisceration had a culture result of Streptococcus or Serratia sp.
Table 4 Enucleation or evisceration in nine eyes (10%)
Discussion
The current study reports associations between culture results and clinical presentations and outcomes not clearly demonstrated in previous BAE series. The inability to detect these associations in past studies may have been due to the limited power inherent in smaller case series and the manner in which VA outcomes were analyzed. Previous BAE studies reported the percentage of eyes ≥20/400 or the loss of ≥5 Snellen lines.Citation1–Citation6 While this information is clinically descriptive, it may be limited for comparative purposes by the poor baseline VA of many glaucomatous eyes. Mean logMARΔ more precisely measures VA outcomes in low vision eyes.
The broad groups of causative organisms used in past BAE case series may also have limited the ability to detect associations with VA outcomes. A previous BAE case series used the classification of non-Streptococcus Gram-positive organisms.Citation2 Non-Streptococcus Gram-positive organisms include a wide range of organisms such as Staphylococcus aureus, Enterococcus, and coagulase-negative Staphylococcus cases that have varying VA outcomes. The current study narrowed the analysis to individual causative organisms, strengthening associations with VA outcomes.
An analysis of Gram-negative cases by individual organism showed that Pseudomonas and Serratia cases had worse mean VA outcomes than Moraxella cases. The relatively good VA outcomes of Moraxella cases, 71% ≥ 20/400, confirms the previous report by Berrocal et al of favorable outcomes with Moraxella cases.Citation11
The current study also provides insight into the clinical presentation of causative organisms in BAE. Streptococcus, Pseudomonas, and Serratia cases were associated with a higher mean IOP and worse view of the fundus than coagulase-negative Staphylococcus cases. Similarly culture positive cases were associated with a worse presenting VA and higher presenting IOP than culture negative cases. The clinician can consider the increased likelihood of a more virulent organism and worse visual prognosis when the patient presents with poor VA, high IOP, and poor view of the fundus.
The VA outcome analysis provided in this study confirms what clinicians have suspected for decades. Worse VA outcomes in BAE are associated with the most frequent isolates, Streptococcus sp. and Gram-negative organisms such as Pseudomonas and Serratia sp. When discussing prognosis, clinicians may consider that eyes with Streptococcus sp. and Gram-negative organisms had VA outcomes ≥ 20/400 in only 45% and 46% of cases respectively while eyes with coagulase-negative Staphylococcus sp. Achieved ≥20/400 in 89% of cases.
Interestingly coagulase-negative Staphylococcus cases achieved better VA outcomes despite less aggressive treatment. Only 11% of the coagulase-negative Staphylococcus cases received pars plana vitrectomy compared with 57% of the Streptococcus cases. The higher mean IOP and worse view of the fundus in the Streptococcus cases likely compelled the treating clinician to more frequently favor pars plana vitrectomy. The role pars plana vitrectomy plays in BAE can only be determined by a sufficiently powered prospective randomized control trial. Unfortunately this may not be feasible due to the limited number of BAE cases.
The current study was not designed to determine the best management for BAE, but it does provide insight into the key role causative organisms play in the clinical presentation and prognosis of BAE. Culture-positive cases were associated with worse presenting VA, higher presenting IOP, and worse VA outcomes than culture-negative cases. Streptococcus, Pseudomonas, and Serratia cases were associated with poor presenting view of the fundus and worse VA outcomes than coagulase-negative Staphylococcus and Moraxella cases.
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- LengTMillerDFlynnHWJrJacobsDJGeddeSJDelayed-onset bleb-associated endophthalmitis (1996–2008): causative organisms and visual acuity outcomesRetina9102010 [Epub ahead of print]
- BusbeeBGRecchiaFMKaiserRNagraPRosenblattBPearlmanRBBleb-associated endophthalmitis: clinical characteristics and visual outcomesOphthalmology2004111814951503 discussion150315288977
- Ba’arahBTSmiddyWEBleb-related endophthalmitis: clinical presentation, isolates, treatment and visual outcome of culture-proven casesMiddle East Afr J Ophthalmol2009161202420142955
- KangasTAGreenfieldDSFlynnHWJrParrishRK2ndPalmbergPDelayed-onset endophthalmitis associated with conjunctival filtering blebsOphthalmology199710457467529160018
- MandelbaumSForsterRKGelenderHCulbertsonWLate onset endophthalmitis associated with filtering blebsOphthalmology19859279649723895104
- SongAScottIUFlynnHWJrBudenzDLDelayed-onset bleb-associated endophthalmitis: clinical features and visual acuity outcomesOphthalmology2002109598599111986108
- CiullaTABeckADToppingTMBakerASBlebitis, early endophthalmitis, and late endophthalmitis after glaucoma-filtering surgeryOphthalmology199710469869959186440
- CiullaTABakerASEndophthalmitis following glaucoma filtering surgeryInt Ophthalmol Clin199636387968989602
- PoulsenEJAllinghamRRCharacteristics and risk factors of infections after glaucoma filtering surgeryJ Glaucoma20009643844311131749
- SharanSTropeGEChipmanMBuysYMLate-onset bleb infections: prevalence and risk factorsCan J Ophthalmol200944327928319491982
- BerrocalAMScottIUMillerDFlynnHWJrEndophthalmitis caused by Moraxella speciesAm J Ophthalmol2001132578879011704047