Abstract
Purpose
To compare the agreement and efficiency of a swept source-optical coherence tomography biometer, IOLMaster 700 (IOLM700), and a low-coherence optical reflectometry biometer, LENSTAR LS 900 (LS900), when acquiring biometry measurements during cataract evaluation.
Methods
A retrospective chart review of biometry measurements that were performed in 64 eyes of 32 patients on the same day using the LS900 and the IOLM700. The total image acquisition time per subject was compared between the two machines using a Wilcoxon rank-sum test. Bland–Altman plots showing the mean difference and 95% limits of agreement were graphed. Intraclass correlation coefficients (ICCs) were calculated for the mean axial length (AL), anterior chamber depth (ACD), lens thickness (LT), and two keratometry mean values (K1 and K2) that were output from each device.
Results
The average time to complete biometry measurements in both eyes was significantly shorter for the IOLM700 compared with the LS900 (44.5±12.4 vs 168.8±67.2 seconds, P<0.001). The Bland–Altman analysis and ICCs showed high degrees of agreement for the mean biometry values (ICC: AL 0.9999, ACD 0.9993, LT 0.9571, K1 0.9922, K2 0.9926) generated by the two devices.
Conclusion
There was a high level of agreement between the mean biometry output measures for IOLM700 and LS900. However, it took ~73% less time on average to acquire the images when using the IOLM700 compared with the LS900. In a busy clinic setting, use of the IOLM700 for biometry measures may save time and prove more efficient.
Introduction
Biometry is an essential component of the cataract evaluation. Along with improved surgical techniques and fifth-generation intraocular lens (IOL) power calculation formulas, advances in biometric technology have allowed for unprecedented refractive outcomes.Citation1 Over the past few decades, ocular biometry has evolved rapidly away from the use of contact ultrasound probes to the implementation of noncontact imaging modalities. In 2000, the IOLMaster (Carl Zeiss Meditec AG, Jena, Germany) was released in the United States as the first noncontact automatic biometry device.Citation2 The initial IOLMaster employed partial coherence interferometry,Citation3 which utilizes a low-coherence light source to scan the eye while reflections are detected by a scanning mirror in order to produce optical A scans.Citation4 Ten years later, the IOLMaster 500 (IOLM500) was introduced and quickly gained popularity over the previous generation because it offered increased speed and dual-mode measurements that allowed for simultaneous axial length (AL) and keratometry calculations.Citation2
The LENSTAR LS 900 (LS900; Haag-Streit AG, Koeniz, Switzerland) has become one of the most commonly used biometry devices since its Food and Drug Administration approval in 2009.Citation5 It combines optical low-coherence tomography with a 32-point pattern dual zone keratometry,Citation6 which contributes to the excellent level of precision delivered by the machine.Citation7 Utilizing optical low-coherence tomography, optical A-scans are acquired, and AL and anterior chamber depth (ACD) are calculated in a manner similar to the IOLM500. Moreover, the LS900 biometric parameters were expanded to include central corneal thickness (CCT) and lens thickness (LT).Citation8
In 2015, the IOLMaster 700 (IOLM700) was released in the United States. This device has an integrated swept source-optical coherence tomography (SS-OCT) with a tunable laser of 1,055 nm as a light source, which generates optical B-scans allowing cross-sectional visualization of the eye. Because the narrow bandwidth light source reflections are projected to the eye one at a time, the SS-OCT has an improved signal-to-noise ratio.Citation4 This enhanced visualization has improved the accuracy of biometry measurements in eyes with posterior subcapsular cataracts and dense cataracts.Citation6,Citation9–Citation11 Also, the IOLM700 measures CCT and LT,Citation8 which was not possible with the IOLM500.Citation8 The IOLM700 also utilizes telecentric keratometry, which combines a 950 nm light source and a unique optical configuration to ensure spot size remains constant irrespective of device-to-eye distance.Citation6 This technology makes patient movements less disruptive to image acquisition.
Although newer generation biometry devices strive to improve upon earlier versions,Citation6 it is not clear which biometry device is optimal. Moreover, there are many factors to consider when comparing biometry devices, ranging from accuracy and reproducibility to efficiency and cost. Previous studies have shown excellent correlation and agreement between the biometry output of the LS900 and IOLM500Citation8,Citation12 and IOLM700.Citation8 However, to our knowledge, no study has yet compared the efficiency of the LS900 and IOLM700 in terms of the time they take to acquire images.
As patient volume has risen over the past decade, clinic efficiency has emerged as an increasingly important metric that physicians and clinic administrators assess.Citation13,Citation14 The time that it takes to acquire images during patient evaluation impacts clinic flow, which ultimately can affect the patient experience. Our study sought to compare two modern biometry devices, the IOLM700 and LS900, not only in terms of their level of agreement on biometry measurements but also on the total time they took to acquire the images.
Methods
We conducted a retrospective review of adult subjects aged above 25 years who underwent evaluation for cataract surgery at a single academic center. This study was approved by the Institutional Review Board of Duke University Hospital and was conducted in accordance with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. A waiver of informed consent was granted due to the retrospective nature of this study. All data were de-identified for the purpose of statistical analysis.
All included subjects underwent a complete ophthalmic examination by a cornea specialist (PG). Eyes were excluded from the study if they had evidence of corneal or retinal pathology, prior refractive surgery, or abnormal structure, such as phacodonesis, white cataract, or corneal scar that would negatively impact the accuracy of biometry imaging. Subject eyes were imaged with both the IOLM700 and LS900 as part of their routine evaluation for cataract surgery. The order of the imaging test was random. Imaging technicians with extensive experience using both biometers recorded the start and stop time for total image acquisition for each subject by each machine as part of quality improvement.
The mean biometry values for AL, ACD, LT, and the flat (K1) and steep (K2) keratometry values were estimated by each machine (). To compare the agreement between the two devices, two-way mixed effects models were used to calculate the intraclass correlation coefficient (ICC) for each of the biometry values. Linear regression analysis comparing the biometry values of the two machines was performed with clustered standard errors to account for multiple eyes within subjects, and the fitted values were graphed. Agreement between the two devices was also evaluated for each biometry value using the method of Bland and Altman, by plotting the difference between the measurements on the y-axis against the average of the measurements on the x-axis.Citation15 The 95% limits of agreements (LoA) were defined as the mean ± 1.96 SD of the difference between the measurements of the two devices. Total image acquisition time per subject was also compared between the two machines using a nonparametric Wilcoxon signed-rank test. A P-value <0.05 was considered statistically significant.
Results
shows the demographic characteristics of the study subjects. A total of 64 eyes of 32 subjects were included in this study. The acquisition times for the IOLM700 and LS900 are compared in . The mean acquisition time waŝ73% less for the IOLM700 (44.5±12.4 seconds) compared with the LS900 (168.8±67.2 seconds, P<0.001).
Table 1 Demographics of the study subjects
Table 2 Mean acquisition times of the IOLMaster 700 and LENSTAR LS 900
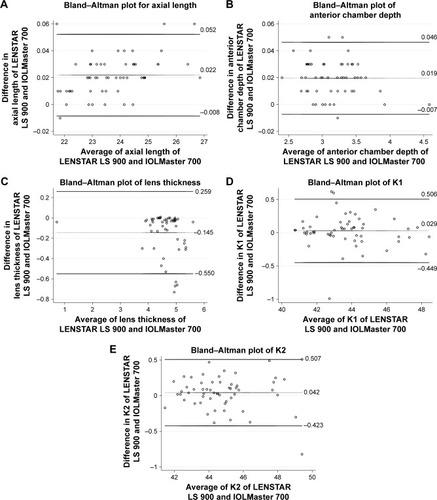
shows the mean biometry values for AL, ACD, LT, K1, and K2 as well as the ICC. An ICC of <0.50 signifies poor agreement between the two devices, while 0.50–0.75 signifies moderate agreement, 0.76–0.90 good agreement, and 0.91–1.00 excellent agreement.Citation16 For all mean biometry values, there was excellent agreement between the two devices with all values having an ICC >0.90. shows graphs of the predicted values of the biometry measurements from regression analysis. shows the Bland–Altman plots for each of the biometry values with the mean difference and the upper and lower 95% LoA graphed. There were relatively few outliers: ACD had three, AL had four, LT had four, K1 had three, and K2 had one outlier. No definite systematic bias was observed.
Table 3 ICCs between the mean biometry values of the IOLMaster 700 and LENSTAR LS 900
Figure 2 Linear regression of the IOLMaster 700 vs the LENSTAR LS 900.
Abbreviation: K, keratometry.
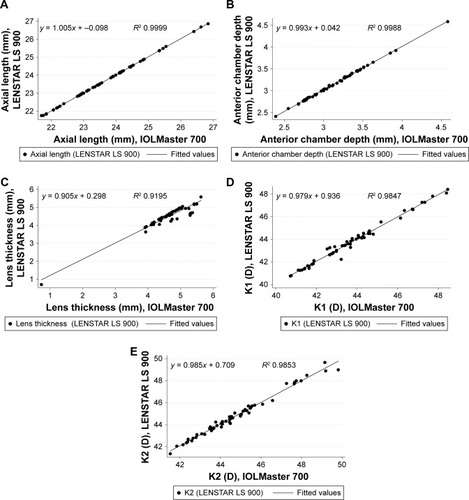
Figure 3 Bland–Altman plots showing the mean difference (dotted line) and 95% upper and lower limits of agreement (solid lines) for biometry measurements obtained by the IOLMaster 700 and LENSTAR LS 900.
Abbreviation: K, keratometry.
Discussion
Optical biometry is a key component of preoperative planning for cataract surgery. Accurate and reproducible biometry measurements are critical to obtain the highest refractive accuracy and minimize postoperative refractive surprise. However, the time it takes to obtain measurements also deserves attention as it has the potential to impact clinic flow and patient experience. Our study confirms that the biometry values estimated by the IOLM700 achieve a high level of agreement with the LS900. However, to our knowledge, we are the first to show that image acquisition takeŝ73% less time on average when utilizing the IOLM700 compared with the LS900. Our findings suggest that the IOLM700 may be more efficient than the LS900 for biometry measurement during routine cataract evaluation.
Several prior studies have sought to compare biometry devices in terms of their accuracy and their relative degree of agreement. Hui and Yi showed that the LS900 and IOLMaster V5.4 biometry values were highly correlated and that the IOL power calculations for the AcrySof SA60AT IOL were similar.Citation17 Both Rohrer et alCitation12 and Rasilber et alCitation18 have demonstrated very high to excellent correlation between the mean outputs of the IOLM500 and the LS900. In a 2017 meta-analysis by Huang et al that compared 18 studies involving 1,921 eyes, no difference was found in AL, ACD, and keratometry readings between the LS900 and IOLMaster.Citation19 In a more recent study of 120 eyes, Kunert et al demonstrated excellent agreement between the IOLM700, IOLM500, and LS900.Citation8 Similar studies by Kurian et al and Shammas et al comparing the IOLM700 and the LS900 have also shown both good reproducibility and agreement.Citation6,Citation20 Our study also demonstrates that the IOLM700 and LS900 show excellent agreement in terms of their biometry output, but we are the first to show that the IOLM700 requires significantly less time to acquire images.
The ability of the IOLM700 to obtain images more quickly may be attributable to its integration of both telecentric keratometry and SS-OCT technology.Citation4,Citation9 Specifically, the rapid cycle, tunable 1,055 nm laser source has been shown to give a better signal-to-noise ratio and has improved tissue penetration.Citation4,Citation9 Also, the LS900 may require better cooperation from subjects since all images are acquired in a single position with one release procedure. If it is difficult for a patient to remain still during image acquisition, then it is possible that the LS900 measurements may be more difficult to acquire, leading to longer total imaging time. By comparison, the IOLM700 acquires images via three different positions and release proceduresCitation17 and thus might require a shorter attention span by the subjects for each imaging position.
Limitations of our study include the retrospective nature of this study and the modest sample size. Also, we excluded eyes that had significant corneal or retinal pathology, which may limit the generalizability of these results. Finally, given the retrospective nature of the study, we did not directly evaluate whether the shorter time for image acquisition impacted clinic flow or patient experience. Future studies should aim to better elucidate whether the IOLM700 performs significantly better than the LS900 in terms of patient experience, clinic flow, and cost-effectiveness.
Conclusion
Our study confirms that there is a high level of agreement in the mean biometry values generated from images acquired by the IOLM700 and LS900. However, image acquisition by the IOLM700 takes approximately three-fourths less time than image acquisition by the LS900, making it substantially more efficient. When compared with biometry machines that use older technology, machines that incorporate SS-OCT technology may save time and have the potential to improve clinic flow and patient experience.
Disclosure
Dr Gupta is a consultant to Aurea, Allergan, Alcon, BioTis-sue, Johnson and Johnson Vision, Kala, Novabay, Novartis, Ocular Science, Shire, Tear Lab, Tear Science, and Zeiss. Dr Thompson is a recipient of the Heed Fellowship. All authors have no other conflicts of interest in this work.
References
- KaneJXvan HeerdenAAtikAPetsoglouCIntraocular lens power formula accuracy: comparison of 7 formulasJ Cataract Refract Surg201642101490150027839605
- Carl Zeiss Meditec Receives FDA Clearance for the IOLMaster 500 Biometer2010118 Available from: http://www.marketwired.com/printer_friendly?id=1348694Accessed May 5, 2018
- Optical Biometry Explained Available from: https://cataract-community.zeiss.com/optical-biometry-explainedAccessed May 5, 2018
- SrivannaboonSChirapapaisanCChonpimaiPLoketSClinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometerJ Cataract Refract Surg201541102224223226703299
- GoldmanDADee StephensonPWhich device do surgeons prefer for optical biometry?2015825 Available from: https://www.healio.com/ophthalmology/cataract-surgery/news/print/ocular-surgery-news/%7B4edddbf9-9621-41ef-84e6-046cbb8c98e1%7D/which-device-do-surgeons-prefer-for-optical-biometryAccessed May 25, 2018
- KurianMNegalurNDasSBiometry with a new swept-source optical coherence tomography biometer: repeatability and agreement with an optical low-coherence reflectometry deviceJ Cataract Refract Surg201642457758127113881
- LENSTAR LS 900 Improving outcomes – Haag-Streit Diagnostics20168 Available from: https://www.haag-streit.com/fileadmin/Haag-Streit_USA/Lenstar/Landing/papers/Brochure_Lenstar_eng.pdfAccessed May 25, 2018
- KunertKSPeterMBlumMRepeatability and agreement in optical biometry of a new swept-source optical coherence tomography-based biometer versus partial coherence interferometry and optical low-coherence reflectometryJ Cataract Refract Surg2016421768326948781
- ShajariMCremoneseCPetermannKSinghPMüllerMKohnenTComparison of axial length, corneal curvature, and anterior chamber depth measurements of 2 recently introduced devices to a known biometerAm J Ophthalmol2017178586428263734
- HirnschallNVarsitsRDoellerBFindlOEnhanced penetration for axial length measurement of eyes with dense cataracts using swept source optical coherence tomography: a consecutive observational studyOphthalmol Ther20187111912429498015
- AkmanAAsenaLGüngörSGEvaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500Br J Ophthalmol201610091201120526674777
- RohrerKFruehBEWältiRClemetsonIATappeinerCGoldblumDComparison and evaluation of ocular biometry using a new noncontact optical low-coherence reflectometerOphthalmology2009116112087209219744720
- BohmanBDyrbyeLSinskyCPhysician well-being: the reciprocity of practice efficiency, culture of wellness, and personal resilienceNEJM Catalyst2017 Available from: https://catalyst.nejm.org/physician-well-being-efficiency-wellness-resilience/Accessed May 25, 2018
- MilsteinALeeTHComparing physicians on efficiencyN Engl J Med2007357262649265218160682
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet1986184763073102868172
- KooTKLiMYA guideline of selecting and reporting intraclass correlation coefficients for reliability researchJ Chiropr Med201615215516327330520
- HuiSYiLComparison of two optical biometers in intraocular lens power calculationIndian J Ophthalmol201462993193425370395
- RabsilberTMJepsenCAuffarthGUHolzerMPIntraocular lens power calculation: clinical comparison of 2 optical biometry devicesJ Cataract Refract Surg201036223023420152602
- HuangJMcAlindenCHuangYMeta-analysis of optical low-coherence reflectometry versus partial coherence interferometry biometrySci Rep201774341428233846
- ShammasHJOrtizSShammasMCKimSHChongCBiometry measurements using a new large-coherence-length swept-source optical coherence tomographerJ Cataract Refract Surg2016421506126948778