Abstract
Purpose
The purpose of this study was to determine the satisfaction levels of patients at least 2 years after cataract surgery implantation with bilateral accommodating or bilateral multifocal intraocular lenses (IOLs) and to determine the relative rate of spectacle independence and adverse symptoms in that same time frame.
Design
Patient questionnaire administered in a single-center private practice at least 2 years after cataract surgery with presbyopia-correcting IOL implantation.
Methods
Patients who had undergone uncomplicated cataract surgery with an accommodating or multifocal IOL implant were eligible for inclusion. Patients with visually significant non-IOL-related postoperative morbidity were excluded. Patients with astigmatism or residual refractive error were not excluded. The main outcome measure was patient satisfaction at least 2 years after IOL implantation.
Results
Sixty-eight patients who received accommodating lenses and 49 patients who received multifocal lenses completed the questionnaire. The mean age of all patients was 75.7 years at the time of survey; the mean number of years since cataract surgery was 5.4 years. Overall, there were no significant differences between the two groups or within each group between the different lenses used. About 90% of patients in each group were “very satisfied” or “somewhat satisfied” with their vision at least 2 years after the initial surgery. Conversely, only one in eleven patients found his vision to be worse than expected.
Conclusions
The majority of patients who received either accommodating or multifocal IOLs remain satisfied with their lens of choice more than 5 years after the original surgery. Glare and halos remain more noticeable in patients who received multifocal lenses.
Introduction
Presbyopia-correcting intraocular lenses (IOLs) have been available in Europe and the United States for more than a decade, offering the prospect of correcting both cataract and refractive error. Multiple studies have demonstrated a clear relationship between refractive accuracy and patient-reported satisfaction with both accommodating and multifocal lenses; one cannot be achieved without the other.Citation1–Citation8 However, most patient-reported outcomes and satisfaction studies have been conducted with <1 year of follow-up.Citation2–Citation4,Citation8
The patient-perceived value of any refractive solution is borne out over the long term. There are a multitude of reasons why initial patient satisfaction may wane over the years, including a return to spectacle dependence for near tasks, onset of maculopathy in an eye that was healthy at the time of surgery, or onset/progression of dry eye that can affect vision and daily functioning. There may also be reasons patients cite a diminished satisfaction level that are not related to the surgery. One potential reason for patient-reported dissatisfaction over the long term is a significant change in the efficacy of the lens itself.
The purpose of this study, therefore, was to determine if there is a clear difference in the long-term patient satisfaction of these types of lenses among patients who underwent presbyopia-correcting surgery and had healthy eyes at the time of the procedure. To the author’s knowledge, this is the only study to evaluate patient-reported outcomes and satisfaction an average of 5 years postoperatively. The primary outcome was the level of patient-reported satisfaction without regard to refractive outcomes. The secondary outcome was the length of time a patient reported dissatisfaction (if any) with the implant.
Methods
This was a prospective analysis of long-term patient-reported outcomes and satisfaction of post-cataract surgery with an accommodating or multifocal bilateral IOL implantation. All eyes were implanted with the Crystalens (Bausch + Lomb, Bedminster, NJ, USA), the AcrySof IQ ReSTOR (Alcon, Ft Worth, TX, USA), or the Tecnis Multifocal 4.0D (AMO, Abbott Park, IL, USA) IOL, with the surgeon using the most recent iteration/model number available at the time of cataract surgery. Patients who had undergone uncomplicated cataract surgery at least 2 years prior were identified through a database search and considered for enrollment in the patient-reported outcomes survey. In an attempt to identify 50 patients who could be enrolled in each group (multifocal and accommodating lenses), we searched data on all cataract surgeries performed from June 2005 to July 2013.
At the time of cataract surgery, all patients had a potential visual acuity (VA) of 20/25 as ascertained by the cataract surgeon, with a refractive goal in the nondominant eye of -0.75 D for patients receiving the Crystalens and a refractive goal of plano/plano in the multifocal IOL patients. (“Potential VA” was defined as predicted best corrected VA, with or without spectacles.) Exclusion criterion was any patient who had developed visually significant non-IOL-related morbidities during the postoperative period. Patients who had undergone postoperative YAG laser capsulotomy or laser refractive enhancement procedures were not excluded from the study. For the purposes of this analysis, an examiner masked to the type of implant examined a table from a database query showing the recent findings (not including IOL type) and diagnoses of all patients who responded to the questionnaire. (See Figure S1 for the questionnaire.) If, at the time of the survey, the patient had severe dry eye, maculopathy, posterior capsule opacification, or previous refractive surgery, the patient was excluded from analysis. Neither astigmatism nor residual refractive error were exclusion factors, as the author believes either of those conditions may affect patient-reported satisfaction.
The survey was administered in a single-center private practice setting by a technician masked to the type of IOL implant. Initially 224 patients were identified who could participate in the study; of those, 117 patients met both the inclusion/exclusion criteria and responded to the questionnaire and, therefore, had analyzable data. Of those, 68 patients received accommodating IOLs and 49 patients received multifocal IOLs.
Aspire IRB (Santee, CA, USA) approved the study protocol, and all participating patients provided a written informed consent, consistent with the Declaration of Helsinki.
Results
Demographics
Overall, the mean age of all patients was 75.7 years at the time of the survey (range, 56–93 years), and the mean number of years since cataract surgery was 5.4 years (range, 2–10 years). Those who received an accommodating lens (group 1; n=68) had a mean age of 75.8 years (range, 56–91 years) at the time of the survey, and the mean number of years since cataract surgery was 6.1 years (range, 2–10 years). Those who received a multifocal lens (group 2; n=49) had a mean age of 75.6 years (range, 63–93 years) at the time of the survey, and the mean number of years since cataract surgery was 4.5 years (range, 2–8 years). YAG capsulotomies had been performed since surgery in 29 (43%) patients in group 1 and 19 (39%) in group 2. Refractive enhancement surgery had been performed following cataract surgery in five patients (7%) in group 1 and four patients (8%) in group 2. These differences were not statistically significant. No patient underwent a lens exchange after the initial cataract surgery in either group.
Patient-reported outcomes and satisfaction
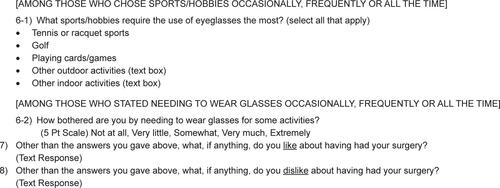
Overall, for patient-reported satisfaction, there were no significant differences between groups 1 and 2 or within each group between the different lenses used. In group 1, 67 of 68 (97%) of patients and in group 2, 44 of 49 (90%) patients were either “very satisfied” or “somewhat satisfied” with their vision at least 2 years after the initial cataract surgery (). Conversely, only one in eleven patients found their vision to be worse than expected postoperatively ().
Figure 1 Patient satisfaction levels at least 2 years after presbyopia-correcting intraocular lens implantation.
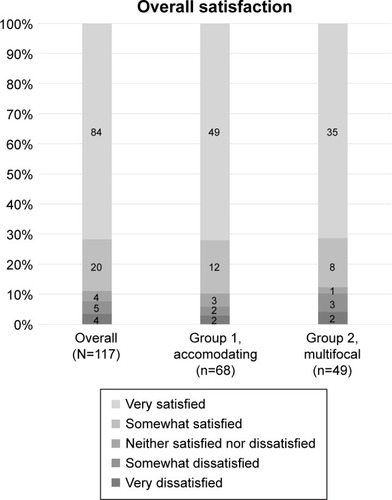
Figure 2 Patient expectations with vision at least 2 years after presbyopia-correcting intraocular lens implantation.
In group 1, 81% were “very likely” to refer friends/family and 9% were “likely” to refer friends/family. In this group, 26% considered vision “much better” than expected and only 1% considered vision “much worse” than expected (P<0.54). In Group 2, 73% were “very likely” to refer friends/family and 16% were “likely” to refer friends/family. In this group, 35% considered vision “much better” than expected and only 4% considered vision “much worse” than expected. The between-group differences were not statistically significant.
Both the groups wanted daylight driving and reading newspaper print without glasses as their top two desired activities postoperatively; 65% of group 2 and 54% of group 1 (P<0.67) wanted nighttime driving to be spectacle-free.
Patient-reported dissatisfaction
In group 1, six of 68 patients (8.8%) considered vision worse than expected. In group 2, six of 49 patients (12%) considered vision worse than expected. More patients in group 2 than in group 1 complained of glare; more patients in group 1 than in group 2 complained of difficulty reading fine print spectacle-free. In group 1, the top two reasons for dissatisfaction were reading fine print more difficult than anticipated (n=5) and the need to wear glasses more than anticipated (n=4). In group 2, the top two reasons for dissatisfaction were being bothered by glare/halo (n=3) and reading fine print more difficult than anticipated (n=3).
Glare and halos
More patients in group 2 (56%) than group 1 (31%) were bothered by glare and halo; this was statistically significant (P<0.02). Conversely, 44% of patients in group 1 and 16% of patients in group 2 were “not at all” bothered by glare and halo (P<.001). In group 1, 12% of patients were “very much” or “extremely” bothered by glare and halo, whereas in group 2, 36% of patients were “very much” or “extremely” bothered by glare and halo (P<0.02).
Spectacle need
Patients reported generally small differences in spectacle independence between groups. For watching television, 76% of patients in group 1 and 73% of patients in group 2 reported they “never” wore spectacles. For driving during daylight, 70% in group 1 and 75% in group 2 reported they never wore glasses, and for driving at night, 62% in group 1 and 67% in group 2 similarly reported no need for spectacles. For near vision tasks, 54% of patients in group 1 and 63% in group 2 reported never needing spectacles to see the computer monitor. None of these differences were statistically significant. However, there were significant differences for reading newspaper-sized print, where 48% in group 1 and 63% in group 2 reported complete spectacle independence (P<0.03), and for reading fine print smaller than newsprint, 22% in group 1 and 46% in group 2 reported never needing spectacles (P<0.02).
When asked if the patients would choose a different lens that would increase the need for reading glasses, but reduce the glare side effect, the majority of patients in both the groups would not (group 1, 71%; group 2, 72%). Patients in both the groups were “somewhat bothered” by needing glasses for different activities. These differences were not statistically significant.
Subgroup analyses
As technology evolved, patients received the current design for the IOL brands at the time of implant. Subgroup analyses of the various models within each brand showed no trend toward different results for any subgroup.
Discussion
This study was designed to evaluate patient satisfaction levels more than 5 years after cataract surgery with either an accommodating or a multifocal lens implant. This is significant because the average patients undergoing cataract surgery in the US are aged 69 years,Citation9 and the average life expectancy in the US is 79 years.Citation10 Thus, this study evaluates patient-reported outcomes and satisfaction of the “average” patients after half their remaining lifespan has passed.
In this study there were high levels of patient-reported satisfaction and a generally high level of acceptance of visual disturbances, such as halo and glare. Even with these visual disturbances, patients were generally unwilling to trade reduced visual disturbances if the tradeoff meant increased spectacle correction.
Multifocal lenses are widely thought to be the lens of choice for spectacle independence across a wide range of distances post-cataract surgery/post-refractive lens exchange surgery.Citation11–Citation13 However, this study suggests that patient satisfaction is similar at least 5 years after cataract surgery between multifocal and accommodating lenses. Each type of lens has been designed to perform differently, although both attempt to provide better postoperative vision across multiple range of vision than a monofocal lens.
Multifocal IOLs are known for dysphotopsia (including glare and halo) that can negatively impact the quality of life.Citation14 Glare and halo have been found to be substantially more common in this type of lens than in standard monofocal lenses; one study cited the occurrence of glare and halo as 3.5 times more common than in monofocal lenses.Citation14,Citation15 The US Food and Drug Administration professional labeling of some multifocal IOLs also includes a warning about contrast sensitivity and advises patients to exercise caution when driving at night.Citation16 Pepose et al showed that multifocal IOL implantation (unilateral or bilateral) resulted in more night driving issues and low-contrast issues.Citation16 Advocates of this technology note that any dysphotopsia tends to diminish over time and attribute that dimunition to neuroadaptation. This study found that if neuroadaptation occurred, it had little effect on patients’ ability to notice or be bothered by these dysphotopsia.
Pepose et al also showed bilateral implantation with an accommodating lens or a “mix and match” combination of an accommodating lens and a multifocal lens had statistically better visual outcomes than bilateral multifocal IOL implantation.Citation16 Those results were only 6 months after surgery; this study’s results were at least 2 years after surgery, but do reinforce the earlier bilateral same-lens findings.
Glare and halo by themselves are not an unusual phenomenon and can occur to some degree in almost any pseudophakic patient. The causes can range from minor posterior capsule opacification to minor residual refractive error to ocular surface disease. In this study, the percentage of patients affected by dysphotopsia in the accommodating lens group was similar to the percentages reported by patients receiving monofocal IOLs in other studies.Citation17–Citation19
In group 1, 37 of the patients received a Crystalens HD. Those implants had a 3.0 mm central zone with a different focal power than the lens periphery. Crystalens HD is prone to more dysphotopsia than previous generations of the lens.Citation20–Citation22 The newest lower add generation of accommodating lenses (Crystalens AO) has a uniform lens power across the optic, designed to reduce dysphotopsia.Citation21 Yet within group 1 in this study, there was no difference in the incidence of complaints about glare or halos among patients receiving Crystalens HD than among patients with more recent designs.
Similarly, patients in group 2 were implanted with the AcrySof ReSTOR 3.25 or the Tecnis Multifocal 4.0D, depending on patient choice and lens availability. Since these patients underwent their cataract surgeries, newer iterations of multifocal lenses have been introduced in the marketplace that add between 2.5 and 2.75 D to the “near” zone, shifting the traditional near zone to the intermediate zone. These newer lenses are sometimes referred to as “extended depth of focus.”Citation23,Citation24 By sacrificing uncorrected vision at the nearest working distances, these lenses also claim to reduce the amount of dysphotopsia. The author believes that this same patient questionnaire, if administered in the year 2020 to evaluate patient perceptions long-term with today’s multifocal and accommodating lenses, would yield similar results between the two groups on issues such as spectacle independence for near tasks.
Cataract refractive surgeons readily agree that patients with comorbidities such as dry eye, mild maculopathy, and corneal aberrations as a result of previous refractive surgery or that occur natively may not be candidates for a multi-focal lens because the visual limitations caused by these diseases may cause intolerance of a lens that also causes a loss of contrast sensitivity. Those same comorbidities have not been viewed as a contraindication for accommodating lenses.
Although this patient questionnaire did not address astigmatism, its correction has been shown to be another critical component to patient satisfaction.Citation25,Citation26 Toric IOLs are generally perceived by cataract surgeons as providing the most complete lens-based astigmatic correction offering both high efficacy and safety when compared to other procedures. Were this questionnaire re-administered in the year 2020, we would expect to include patients who received toric accommodating lenses and, based on the results from this patient-reported outcome survey, would predict their satisfaction level would be greater than those who received standard monofocal lenses or newer iterations of multifocal lenses.
Conclusion
Patient-reported outcomes indicate that the majority of patients who received either accommodating or multifocal IOLs remain satisfied with their lens of choice more than 5 years after the original surgery. Glare and halos remain more noticeable in patients who received multifocal lenses.
Acknowledgments
This study was supported by Bausch + Lomb. Partial results have been presented at the Royal Hawaiian Eye Meeting, 2016. Portions of this study were presented at the American Society of Cataract & Refractive Surgeons meeting in 2015.
Disclosure
Dr Hovanesian is a consultant to Alcon, Bausch + Lomb, and Johnson & Johnson Vision. The author reports no other conflicts of interest in this work.
References
- AbdelghanyAAAlioJLSurgical options for correction of refractive error following cataract surgeryEye Vis201412
- Yıldırım KarabağRGünençÜAydınRArıkanGAslankaraHVisual Results Following Implantation of a Refractive Multifocal Intraocular Lens in One Eye and a Diffractive in the Contralateral EyeTurk J Ophthalmol201848161429576891
- McneelyRNPazoESpenceAVisual outcomes and patient satisfaction 3 and 12 months after implantation of a refractive rotationally asymmetric multifocal intraocular lensJ Cataract Refract Surg201743563363828602324
- ChangJSNgJCLauSYVisual outcomes and patient satisfaction after presbyopic lens exchange with a diffractive multifocal intraocular lensJ Refract Surg201228746847522716033
- ChangJSNgJCChanVKLawAKVisual outcomes and patient satisfaction after refractive lens exchange with a single-piece diffractive multifocal intraocular lensJ Ophthalmol20142014458296825505974
- Braga-MeleRChangDDeweySMultifocal intraocular lenses: relative indications and contraindications for implantationJ Cataract Refract Surg201440231332224461503
- GundersenKGMakariSOstenstadSPotvinRRetreatments after multifocal intraocular lens implantation: an analysisClin Ophthalmol20161036537127041983
- ShimodaTShimodaGHidaWTVisual outcomes after implantation of a novel refractive toric multifocal intraocular lensArq Bras Oftalmol2014772717525076467
- ScheinODCassardSDTielschJMGowerEWCataract surgery among Medicare beneficiariesOphthalmic Epidemiol201219525726422978526
- Centers for Disease Control and PreventionLife expectancy2017 Available from: https://www.cdc.gov/nchs/fastats/life-expectancy.htmAccessed June 19, 2017
- HawkerMJMadgeSNBaddeleyPAPerrySRRefractive expectations of patients having cataract surgeryJ Cataract Refract Surg200531101970197516338569
- PagerCKExpectations and outcomes in cataract surgery: a prospective test of 2 models of satisfactionArch Ophthalmol2004122121788179215596581
- MuñozGAlbarrán-DiegoCFerrer-BlascoTSaklaHFGarcía-LázaroSVisual function after bilateral implantation of a new zonal refractive aspheric multifocal intraocular lensJ Cataract Refract Surg201137112043205222018366
- SheppardALShahSBhattUBhogalGWolffsohnJSVisual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lensJ Cataract Refract Surg201339334334923332118
- LeylandMZinicolaEMultifocal versus monofocal intraocular lenses in cataract surgery: a systematic reviewOphthalmology200311091789179813129879
- PeposeJSQaziMADaviesJVisual performance of patients with bilateral vs combination Crystalens, ReZoom, and ReSTOR intraocular lens implantsAm J Ophthalmol2007144334735717651679
- AllenRHo-YenGOBeckingsaleABFitzkeFWSciscioAGSalehGMPost-capsulotomy dysphotopsia in monofocal versus multifocal lensesClin Exp Optom200992210410919054013
- WilkinsMRAllanBDRubinGSRandomized trial of multifocal intraocular lenses versus monovision after bilateral cataract surgeryOphthalmology2013120122449245524070808
- Martínez PalmerAGómez FaiñaPEspaña AlbeldaAComas SerranoMNahra SaadDCastilla CéspedesMVisual function with bilateral implantation of monofocal and multifocal intraocular lenses: a prospective, randomized, controlled clinical trialJ Refract Surg200824325726418416260
- DevganULindstromRLSingerJAWhitmanJFirst Impressions of the Crystalens HD. Cataract & Refractive Surgery TodayBryn Mawr, PABMC Publications2008
- KezirianGMChuYRFeinermanGCrystalens AO: Surgical Experience. Cataract & Refractive Surgery TodayBryn Mawr, PABMC Publications2010
- SladeSGStrategies for Success with Five Refractive IOLs. Cataract & Refractive Surgery TodayBryn Mawr, PABMC Publications2009
- CalogeroDNew Categories of IOLs for Improved Near and Intermediate PerformanceWashington, DCUnited States Food and Drug Administration2014
- GallegoAABaráSJaroszewiczZKolodziejczykAVisual Strehl performance of IOL designs with extended depth of focusOptom Vis Sci201289121702170723190714
- GyöngyössyBJirakPSchönherrURotational stability and patient satisfaction after implantation of a new toric IOLEur J Ophthalmol201626432132726541110
- FarooquiJHKoulADuttaRShroffNMManagement of moderate and severe corneal astigmatism with AcrySof® toric intraocular lens implantation – Our experienceSaudi J Ophthalmol201529426426926586976