Abstract
Background:
The purpose of this study was to evaluate the applicability and variability of echographic imaging using 10 mHz and high-resolution 20 mHz B scanning for measurement of intraocular tumors.
Methods:
This prospective consecutive study comprises 27 eyes in 27 patients with uveal melanoma. Each patient was examined by three experienced examiners independently on three occasions within a two-week time frame in a blinded manner. The height of the lesion was measured by all examiners using the 10 mHz B, 20 mHz B, and 8 mHz A scan probes. Additionally, basal diameter was examined using the 10 and 20 mHz B scan.
Results:
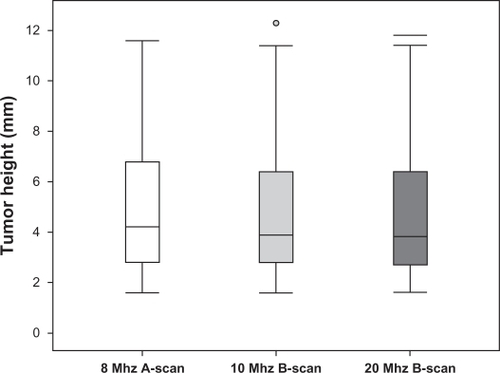
Tumor height measurements for all examiners using the standardized A scan tended to be higher than for both B scan measurements. Statistical analysis revealed significant differences in tumor height between B and A scan measurements. No difference in tumor height was found between the two B scan techniques (P = 0.239). Basal tumor diameter measurements revealed significant differences between 10 mHz and 20 mHz B scans (P < 0.001 and P = 0.001, respectively). For the 10 mHz B scan, basal diameter results tended to be larger than for the 20 mHz B scan. No difference was found for interobserver variation in all A scan and B scan examinations. The mean standard deviation of the difference in tumor height measurements between the examiners was ±0.24 mm for the 8 mHz A scan, ±0.46 mm for the 10 mHz B scan, and ±0.42 mm for the 20 mHz B scan. Both the 10 mHz and more precise 20 mHz B scan evaluations underestimated tumor height.
Conclusion:
The 20 mHz ultrasound probe, despite its theoretically higher resolution, is not able to replace A scan measurements of tumor height.
Introduction
Ophthalmic ultrasound plays a pivotal role in the diagnosis and follow-up of intraocular tumors. Basal tumor diameter, tumor height, and tumor volume are considered to be important prognostic indicators, especially in choroidal melanoma, the most common primary intraocular malignancy in adults.Citation1–Citation3
Standardized echography is a common and inexpensive technique for biometry and measuring intraocular tumors. This technique was introduced by Ossoinig in the 1960s. Standardized echography refers to a special examination technique which combines the use of a standardized A scan instrument developed for tissue differentiation and a real-time contact B scan. The standardized A scan is characterized by both internal (special signal processing through defined parameters) and external (ascertainment of the tissue sensitivity setting by the examiner) standardization, as well as a predefined A scan and B scan examination of the globe.Citation4 In standardized echography, an 8 mHz A scan probe is used for measuring tumor height and a 10 mHz B scan probe is used for the tumor base and topographic and morphological evaluation.
Since its inception, B scan ophthalmic ultrasound has employed frequencies near 10 mHz, providing good general-purpose imaging of the vitreous, posterior coats, and the anterior orbit. In the 1990s, instruments utilizing higher frequencies were implemented for imaging of the anterior segment and posterior pole of the eye.Citation5,Citation6 Recently, the new technical development of sensitive broadband 20 mHz transducers has allowed higher frequencies to be used for imaging the posterior globe. The 75 μm wavelength of ultrasound at 20 mHz is half the wavelength of a 10 mHz transducer, and therefore is theoretically capable of providing a two-fold improvement in resolution. Because the 20 mHz transducer has now become more popular, the aim of our study was to investigate the precision and interobserver variability of the 20 mHz scan compared with the conventional 10 mHz B scan and 8 mHz A scan transducer in measuring the dimensions of intraocular choroidal melanoma tumors by standardized echography.
Methods
Twenty-seven eyes in 27 consecutive patients of varying ages were included in this prospective blinded study. Measurements were performed within a six-month period. The study was approved by the local institutional review board. Informed consent was obtained from all persons in the study. Twenty of the patients had undergone radiation therapy in the past. Criteria for inclusion were uveal melanoma tumors not involving the iris or ciliary body. Each patient was examined independently three times by three experienced examiners within a two-week time frame. This protocol was chosen to avoid possible bias between the measurements of real tumor growth. The three examiners performed standardized echographic evaluations independent of each other. The data were stored in an Excel (Microsoft Excel, Microsoft, Seattle, CA) spread sheet by a fourth person, therefore no examiner was aware of previous results. In all cases, the same instrumentation was used for A scan and B scan examinations (Cine Scan S, Quantel Medical SA, Le Brezet, France). With regard to the standardized echographic technique, specific criteria described by Ossoinig were used to evaluate intraocular tumor dimensions.Citation4,Citation7,Citation8 All scans were performed with the patients placed in a supine position on a reclining chair. To avoid sound attenuation, particularly with the 20 mHz probe, the B scan probes were placed directly on the sclera, using a coupling gel (Methocel 2%, OmniVision GmbH, Puchheim, Germany). Each examination consisted of a preliminary topographic 10 mHz B scan evaluation.
During the first visit, the shape of the lesion and the measurement of both maximum transverse and longitudinal extension of the tumor base, as well as the tumor height with calipers, was performed employing the 10 mHz B scan probe. The direction of the patient’s gaze during measurement of diameter and tumor height was directly to the intraocular tumor, eg, if the tumor was peripherally at 12 o’clock, the patient was asked to look up and the B scan probe was positioned at 6 o’clock.
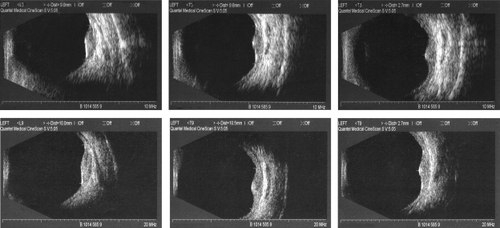
On the next visit, after new exploratory location of the tumor, the shape of the lesion, maximum transverse and longitudinal extensions of the tumor base, and tumor height were determined with calipers using the 20 mHz B scan probe. A relatively low gain setting was used in order to obtain the best measurement at both examinations. Measurements were taken of the inner sclera, which was identified as the first distinct line at the tumor base continuous with the surrounding fundus. Gain settings for B scan evaluation employing either 10 or 20 mHz were not specified. B scan tumor heights were measured by placing the inner caliper on the tumor surface spike once the tumor surface and the scleral spike were displayed in their maximum height during either transverse or longitudinal B scans. shows the tumor dimension measurements taken with the 10 mHz and 20 mHz probes. In the event of an existing retinal detachment, careful attention was paid to avoid setting the inner caliper on the surface spike of the tumor and not on the overlying retina.
Figure 1 Ultrasound images of small ocular melanoma (82-year-old female, no previous treatment). Images display measurements of longitudinal and transversal diameter and tumor height (from left to right). Upper images show measurements with the 10 mHz B scan ultrasound transducer, lower images show the corresponding measurements with the 20 mHz B scan transducer.
At the third and final visit, a standardized A scan instrument was first set at tissue sensitivity with the probe placed on the opposite site of the tumor. Careful attention was paid to a thorough perpendicular orientation of the sound beam with respect to the point of maximal tumor elevation and the inner sclera. Once the tumor surface spike and the scleral spike were displayed in their maximum height, the gain was lowered and the screen continuously monitored until the peaks were distinct and clear. Measurements were obtained by placing calipers on the peak of the surface spike and the inner scleral spike. In the presence of an existing retinal detachment, careful attention was paid to avoid setting the inner caliper on the surface spike of the tumor and not on the overlying retina. At least three high-quality images were taken, and the photograph representing the most accurate measurement was finally chosen by the examiner. The A scan tumor height was then documented.
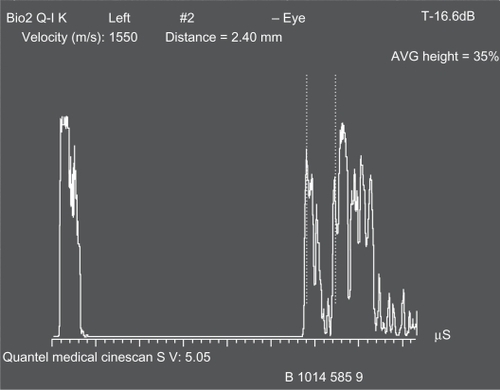
shows an image of an A scan tumor height measurement. Other documented parameters were shape, internal reflectivity, internal structure, vascularity, and location of the lesion. A minimum time span between examinations was set at two days and maximum time span over all three examinations at 14 days. The data were collected using an Excel spread sheet (Microsoft, Redmond, WA) and analyzed using SPSS 12 (SPSS Inc, Chicago, IL). Evaluations of measurements among the examiners were conducted using the Mann–Whitney U test, as well as the Wilcoxon test when comparing variations between the various techniques of measurement. P ≤ 0.05 was considered to be statistically significant.
Results
The average patient age was 64.1 (range 38–85) years. Twenty patients had undergone radiation therapy in the past at least six months earlier. Tumor heights measured with the A scan ranged from 1.6 to 11.6 mm, and mean tumor height for all patients was 4.2 mm. Three tumors were located close to the optic nerve, seven at the posterior pole, 14 between the vascular arcades and the equator, and three anterior to the equator but still distinguishable. In 10 cases, retinal detachment above the tumor was noted sonographically. Tumors had a dome-shaped configuration in 22 cases (with five tumors displaying an irregular surface contour) and a mushroom appearance in five cases. The main results of the measurements obtained are summarized in . Results of tumor height measurements with the standardized A scan by each examiner tended to be higher than for both B scan measurements (). Statistical analysis revealed significant differences with regard to tumor height between both B scan techniques (10 and 20 mHz) and the A scan measurements (P = 0.003 for A scan versus 10 mHz B scan and P < 0.001 for A scan versus 20 mHz B scan). No significant difference in tumor height was found between the two B scan techniques (P = 0.239, Wilcoxon test, ). In contrast, basal tumor diameter measurements, both transverse and longitudinal, revealed significant differences between 10 mHz and 20 mHz B scans (P < 0.001 and P = 0.001, respectively, Wilcoxon test, ). Basal diameter results for the 10 mHz B scan tended to be larger than in 20 mHz B scan. Evaluation of measurements of diameter and height by the three examiners revealed no significant differences for all A scan, 10 mHz and 20 mHz B scan techniques (P > 0.500 each, Mann–Whitney U test). The mean standard deviation of the difference in tumor height measurements between examiners was ±0.24 mm for the 8 mHz A scan, ±0.46 mm for 10 mHz B scan, and ±0.42 mm for 20 mHz B scan. For the10 mHz B scan, the standard deviation was ±1.0 mm for the transverse and ±1.2 mm for the longitudinal base diameter, and in the 20 mHz B scan was ±1.0 mm for the transverse and ±0.7 mm for the longitudinal base diameters.
Figure 4 Results of basal tumor diameter measurements, both transverse and longitudinal, with the 10 mHz and 20 mHz B scan.
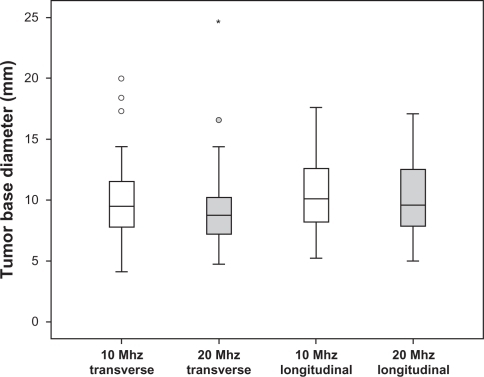
Table 1 Results of tumor height and diameter measurements of each examiner taken with the different ultrasound probes
To evaluate whether tumor size has any influence on precision of tumor height measurements, all lesions were categorized into three groups, ie, Group A, including tumors up to 3.0 mm, Group B, including tumors from 3.1 mm to 6.0 mm, and Group C, including tumors greater than 6.0 mm in height. Statistical analysis again did not reveal significant differences in height measurements in the 8 mHz A scan, or 10 and 20 mHz B scan, or in longitudinal and transverse basal diameter measurements on both B scans between the three examiners in all groups (P > 0.500 each, Mann–Whitney U test). Analogously, in Group A, statistical analysis again revealed no significant differences in height measurements between the 8 mHz A scan and both the 10 and 20 mHz B scans or between both B scan techniques (P ≥ 0.399 each, Wilcoxon test). Contrary to these findings, in Group B, 8 mHz A scan height measurements differed significantly as compared with both the 10 and 20 mHz B scans (P = 0.001 and P = 0.007, respectively, Wilcoxon test). No significant difference in tumor prominence was found between either B scan technique (P = 0.654, Wilcoxon test). Height measurements for tumors in Group C were found to be significantly larger in the 8 mHz A scan as compared with the 20 mHz B scan (P = 0.003, Wilcoxon test), but not compared with the 10 mHz B scan (P = 0.209, Wilcoxon test). Analogously, 10 mHz B scan measurements differed significantly from those with the 20 mHz B scan (P = 0.046, Wilcoxon test) in this group.
Discussion
The present study is the first to compare the 20 mHz B scan transducer with the conventional 10 mHz B scan and 8 mHz A scan transducers, including interobserver variability analysis in measuring the dimensions of uveal melanomas by standardized echography.
The goal of this study was to evaluate the accuracy of the B scan 10 mHz and 20 mHz examination techniques when compared with the top-rated A scan. In standardized echography, the A scan technique is commonly used for tumor height measurement, evaluation of internal structure, reflectivity, and signs of vascularization in the lesion.Citation8 This information can be obtained solely from amplitudes, shapes, and motions of A scan spikes. Because there is no specific gain setting for B scan evaluation, the B scan is primarily used for localizing the tumor and gross exploratory tumor height measurement. The B scan can be used to measure the diameter of a lesion with gradually sloping edges. However, its precision is limited because this measurement relies strongly on signal amplification during the examination, but it still does provide reproducible measurements for follow-up evaluation. The new 20 mHz B scan has advantages over the conventional 10 mHz B scan due to its higher resolution. This should improve the detection of lesion borders, thus improving the precision of measurements. We found statistically significant differences in tumor height evaluation between both B scan methods and the A scan. The 10 mHz and even more precise 20 mHz B scan evaluations underestimated tumor height. A subanalysis showed that this effect was especially associated with greater tumor height. This may be due to difficulties in detecting the lesion’s exact position and determination of the greatest diameter, particularly in 20 mHz B scans where only a small-diameter cross-section of the lesion can be seen on the screen. On the other hand, especially in tumors with subtle subretinal fluid, B scan measurements may not be as precise in positioning the measurement on the choroidal lesion. Our findings support the recommendation that B scan measurements should not be considered a reliable method to determine tumor growth or regression. However, the B scan is the only method other than ophthalmoscopy and fundus photography to evaluate the basal diameter of a choroidal tumor. In addition, it provides evidence of possible extrascleral extension of the lesion. The main domain of the A scan is the measurement of tumor height. Standardization of the A scan ultrasound technique in terms of a “tissue sensitivity setting” allows for easy reproduction of measurements in contrast with the nonstandardized B scan technique.Citation9 One of the main questions in the observation and initiation of appropriate therapy in choroidal melanoma patients is whether the tumor decreases in size (for example, after radiation treatment) or whether tumor growth is observed in smaller melanocytic lesions. Therefore, it is important to determine the accuracy of the examination technique in terms of interobserver and intraobserver variability of measurements. According to our data, a statistical consideration should be taken into account when deciding on tumor growth, ie, measurements falling outside a 95% confidence interval are usually considered as a statistically reasonable indication of true change. Given a normal distribution of the measurements, this means that the measurements have to fall outside plus or minus two standard deviations of the measured value. Therefore, our data from standard deviations between different measurements suggesting a difference in tumor prominence of more than 0.5 mm (two standard deviations) in A scan, may be considered a true change in tumor height, regardless of the absolute tumor height. Tumor shape or location did not influence the results of the measurements obtained in this study.
With respect to the great differences in B scan evaluation of a tumor ( and ), neither the 20 nor 10 mHz B scans should be used as nonstandardized techniques for the definition of tumor growth. Although the 20 mHz B scan provided a higher resolution than the 10 mHz B scan, the standard deviation between examiners was still higher than with the A scan measurements. However, the B scan is still suitable for morphological and topographic examinations. Our standard deviation of 0.24 mm for each examiner is in accordance with data reported by other authors. Nicholson et al reported that approximately 90% of independent measurements by two technicians made from photographic records of 53 previously performed scans were within a 0.4 mm difference, with a standard deviation of 0.22 mm.Citation10 A standard deviation of 0.20 mm for tumor height was also reported by Char et al in a prospective series of 26 patients.Citation11 However, this study focused only on intraobserver variability of echographic measurements, and confirmed ultrasound to be the most accurate method of measuring tumor height. Haritoglou et al reported a standard deviation of 0.18 mm in A scan tumor height measurements in a prospective series.Citation12
Interestingly, in all A scan and all B scan techniques, no statistically significant difference amongst the observers was found. This may be the result of the standardized approach in our institution. Furthermore, in a retrospective review of 32 uveal melanomas, Char et al reported a difference in ultrasound measurements of a thickness of 0.64 mm between two institutions (interobserver variability, range 0–2.2 mm, standard deviation 0.60 mm), both in small and large tumors.Citation13 The correlation between the two institutions was 0.89. According to Char et al, several factors affect these correlations, such as experience in ultrasound measurements, location of the tumor, and the instrumentation used.
However, because those two studies of interobserver variability were performed in a retrospective manner, they did not address the precision of independent measurements during separate dynamic echographic examinations as in our series, but relied on photographic evidence.Citation10,Citation13 In addition, the authors did not describe the intraobserver variability of echographic measurements that play an important part when a patient is seen by the same examiner on different occasions.
In summary, the novel 20 mHz ultrasound probe, despite its theoretically higher resolution, is unable to replace A scan measurement of tumor height. Underestimation of tumor height and the larger standard deviation of measurements lower the value of this technique in follow-up management of intraocular tumors.
Disclosure
The authors report no conflicts of interest in this work.
References
- HawkinsBSThe Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma: IV. Ten-year mortality findings and prognostic factors. COMS report number 24Am J Ophthalmol200413893695115629284
- SeddonJMAlbertDMLavinPTRobinsonNA prognostic factor study of disease-free interval and survival following enucleation for uveal melanomaArch Ophthalmol1983101189418996651594
- ShieldsCLShieldsJAKiratliHDe PotterPCaterJRRisk factors for growth and metastasis of small choroidal melanocytic lesionsOphthalmology1995102135113619097773
- OssoinigKCStandardized echography: Basic principles, clinical applications, and resultsInt Ophthalmol Clin197919127210395120
- PavlinCJHarasiewiczKSherarMDFosterFSClinical use of ultrasound biomicroscopyOphthalmology1991982872952023747
- TillPSolid tissue model for the standardization of the echoophthalmograph 7200 MA (Kretztechnik)Doc Ophthalmol1976412052401009816
- ColemanDJSilvermanRHChabiAHigh-resolution ultrasonic imaging of the posterior segmentOphthalmology20041111344135115234135
- OssoinigKCBigarFKaefringSLMalignant melanoma of the choroid and ciliary body. A differential diagnosis in clinical echographyBibl Ophthalmol19751411541131210
- PulidoJSByrneSFClarksonJGDi BernardoCLHoweCAEvaluation of eyes with advanced stages of retinopathy of prematurity using standardized echographyOphthalmology199198109911041891219
- NicholsonDHFrazier-ByrneSChiuMTSchiffmanJHughesJRNovinskiEKEchographic and histologic tumor height measurements in uveal melanomaAm J Ophthalmol19851004544573898853
- CharDHStoneRDIrvineARDiagnostic modalities in choroidal melanomaAm J Ophthalmol1980892232307355976
- HaritoglouCNeubauerASHerzumHFreemanWRMuellerAJInterobserver and intraobserver variability of measurements of uveal melanomas using standardized echographyBr J Ophthalmol2002861390139412446372
- CharDHKrollSStoneRDHarrieRKermanBUltrasonographic measurement of uveal melanoma thickness: Interobserver variabilityBr J Ophthalmol1990741831852182105