Abstract
Purpose
This study was performed to observe changes prospectively in exophthalmos and orbital fat in patients with inactive thyroid-associated ophthalmopathy (TAO) treated with bimatoprost.
Methods
In this 12-month single-treatment pilot observational study, 13 patients with inactive-phase TAO were administered bimatoprost to treat exophthalmos due to TAO. Exophthalmos values and orbital tissue volumes were measured on MRI by technicians in a masked fashion.
Results
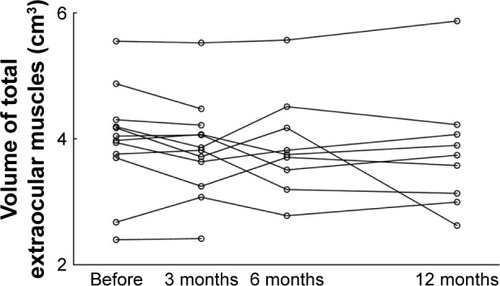
Nine orbits of nine patients (eight women, one man) were treated with bimatoprost for 12 months. Mean exophthalmos values before and after treatment were 21.7±2.2 and 21.7±2.0 mm, respectively. The mean value after 12 months of treatment was not significantly different from before treatment (P=0.82). Mean orbital fat volume before and after 12 months of treatment was 17.2±2.5 and 17.0±3.0 cm3, respectively. The corresponding total extraocular muscle volume was 4.0±0.7 and 3.8±0.9 cm3, respectively. Mean volume in each tissue type after 12 months of treatment was not significantly different from before treatment (orbital fat, P=0.70; extraocular muscles, P=0.32).
Conclusion
Topical bimatoprost treatment did not reduce exophthalmos or orbital fat in this cohort of patients with inactive TAO.
Introduction
Thyroid-associated ophthalmopathy (TAO) is an autoimmune inflammatory disease in the orbit that causes inflammation of extraocular muscle and orbital fat.Citation1–Citation5 Patients present with clinical symptoms and signs that may include exophthalmos, ocular movement disorder, upper-eyelid retraction, and chemosis.Citation5–Citation9 The cause of exophthalmos, which decreases the quality of life of these patients, is mainly an increased amount of orbital fat and enlarged extraocular muscles.Citation10
Methylprednisolone pulse therapy has been reported to reduce the inflammation associated with TAO.Citation11–Citation14 We have reported exophthalmos values and orbital tissue volume in patients with acute-phase TAO before and after methylprednisolone pulse therapy.Citation15 Mean orbital fat volume did not change significantly, although extraocular muscle enlargement decreased significantly. As a result, the mean exophthalmos value was not significantly different after treatment, because the orbital fat volume, which is largest in the orbit, had not changed. Another study also showed that exophthalmos values did not significantly improve after methylprednisolone pulse therapy.Citation16 Therefore, decreasing the amount of orbital fat appears to be the most important factor in alleviating exophthalmos, and studies have shown that orbital fat-decompression surgery is effective for exophthalmos due to TAO.Citation17,Citation18 Another study showed that intravenous administration of teprotumumab, a human monoclonal antibody inhibitor of IGF1R, was effective for exophthalmos in patients with active TAO.Citation19 IGF1R was detected in patients with TAO. Therefore, teprotumumab may result in a reduction in the volume of orbital fat.
Prostaglandin F2α (PGF2α) analogues, such as bimatoprost, have been used in patients with glaucoma or hypertension.Citation20,Citation21 However, previous studies have shown that PGF2α analogues can cause PG-associated periorbitopathy (PAP) such as enophthalmos, periorbital fat atrophy, and deepening of the upper-eyelid sulcus.Citation22–Citation26 PAP has been reported more frequently after the use of bimatoprost than after the use of other PGF 27,28 2α analogues. Those studies reported the presence of enophthalmos and orbital fat atrophy in patients with glaucoma using bimatoprost.Citation28,Citation29 One study showed that PGF2α prevented adipocyte differentiation by activating MAPK and that this mechanism might cause fat atrophy.Citation29 To the best of our knowledge, however, changes in exophthalmos and orbital fat in patients with inactive TAO treated with bimatoprost have not been reported. Therefore, the purpose of this study was prospectively to observe changes in exophthalmos and orbital fat in patients with inactive TAO treated with bimatoprost.
Methods
Patients
Patients with inactive TAO who had developed exophthalmos were enrolled in this prospective interventional study at the Department of Ophthalmology, Shiga University of Medical Science Hospital from August 2015 to June 2018. The design was a 12-month single-treatment pilot observational study of bimatoprost in patients with inactive TAO. This study was approved by the institutional review board of Shiga University of Medical Science. It was conducted in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from each patient.
Exclusion criteria were the presence of TAO in the acute inflammatory phase, a history of treatment with PGF2α analogues, a history of other orbital disease, such as that due to trauma, and/or being at risk for an MRI examination. The study group comprised 13 patients with inactive-phase TAO (13 orbits), whose mean±SD exophthalmos value before treatment was 21.7±1.9 (16.6–24.8) mm.
MRI examinations were performed four times: before treatment and 3, 6, and 12 months after treatment. For each patient, if both orbits were treated with bimatoprost, only data for the right eye were used to avoid data duplication. The primary end point was change in exophthalmos values after 12 months of treatment. To meet the study objective, outcomes were measured not by clinical assessments, such as exophthalmometry, but entirely by MRI findings. Patients were treated for exophthalmos with bimatoprost ophthalmic solution 0.03% (Allergan, Irvine, CA, USA) once a day for 12 months. To avoid PAP-associated pigmentation, patients were instructed strictly to wipe off excess bimatoprost after eyedrop administration.
MRI acquisition
All images were acquired on a 3.0 Tesla MRI unit (Signa HDxt 3.0 T; GE Healthcare, Little Chalfont, UK) with a standard head coil. MR images were obtained using T2-weighted spin-echo MRI with a slice thickness of 1.5 mm. On axial images conditions were: repetition time 4,200 ms, echo time 85 ms, field of view 140 mm, and number of excitations two. Those on coronal and sagittal images were: repetition time 5,000 ms, echo time 85 ms, field of view 140 mm, and number of excitations two.
Exophthalmos measurement
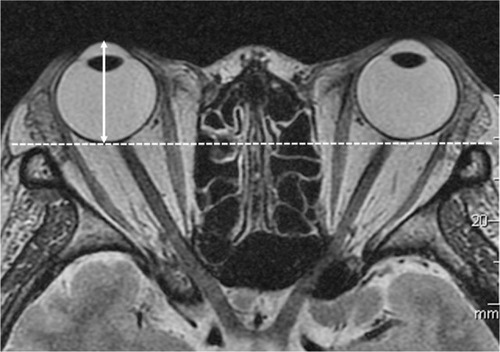
Exophthalmos was measured on axial images using a workstation (Aquarius Intuition software; TeraRecon, Foster City, CA, USA), which was similar to that used in previous studies.Citation15,Citation30 The exophthalmos value was defined as the perpendicular distance from the top point of the corneal surface to the line between the bilateral frontal processes of the zygomatic bone (). Exophthalmos was measured in a masked fashion by two technicians.
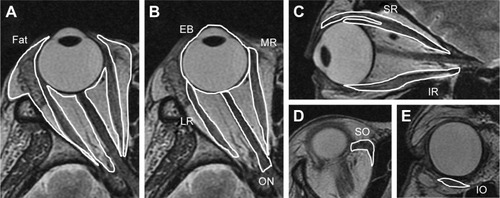
Volume measurement
The volume of each orbital tissue (ie, orbital fat, extraocular muscles, eyeball, optic nerve) were measured on MRI in a manner similar to that used in previous studies.Citation15,Citation31–Citation33 Regions of interest (ROIs) were drawn around the tissue samples on the MR images, and cross-sectional areas of the ROIs were measured using the workstation. Cross-sectional areas of orbital fat, lateral rectus, medial rectus, and superior oblique muscles, eyeball, and optic nerve were captured on axial images (). Areas of the superior rectus and inferior rectus muscles were evaluated on sagittal images. Coronal images were used to evaluate the inferior oblique muscle. ROIs of orbital fat included the lacrimal gland, vessels, and connective tissue, because these structures were difficult to separate. ROIs of the superior rectus muscle included the levator palpebrae muscle for the same reason. The volume of each tissue sample was calculated by multiplying the sum of the cross-sectional areas by the slice thickness (1.5 mm), and measured in a masked fashion by two technicians.
Figure 2 Volume measurement.
Statistical analysis
The Shapiro–Wilk test was used to test the normality of the numerical variables. Paired t-tests were used to compare the exophthalmos values and the orbital tissue volume before and after 12 months of treatment. All analyses were performed using SPSS 22 software (IBM, Armonk, NY, USA). Data are expressed as means±SD. P<0.05 was considered to indicate statistical significance.
Results
Patients
In the final analysis, we analyzed nine orbits of nine patients (eight women, one man; mean age 49.9±10.6 [35–68] years) who had been treated with bimatoprost for 12 months. The mean pretreatment exophthalmos value was 21.7±2.2 mm (16.6–24.8). Five of the nine patients were treated bilaterally with bimatoprost, and four were treated unilaterally. All patients had Graves’s disease, and four of the nine had a treatment history of methylprednisolone pulse therapy. No patients had a history of orbital surgery or orbital radiotherapy. Characteristics of the patients are listed in .
Table 1 Characteristics of patients with TAO
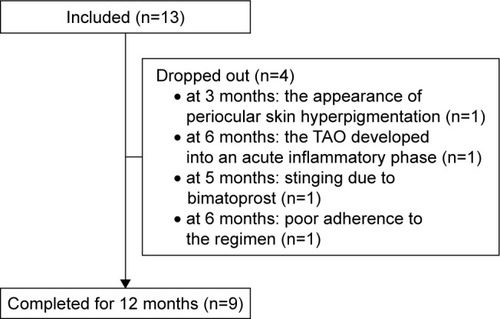
During the 12-month period, 4 of 13 patients dropped out of treatment (). One of the four dropped out at 3 months because of the appearance of periocular skin hyperpigmentation. The second patient dropped out at 6 months because the TAO developed into an acute inflammatory phase. The third patient dropped out at 5 months because of stinging due to bimatoprost. Finally, the fourth patient dropped out at 6 months because of poor adherence to the regimen.
Exophthalmos
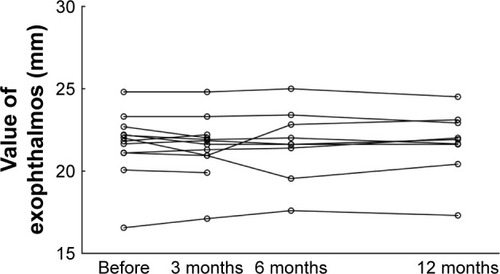
Mean exophthalmos values before and after 12 months of treatment are shown in . The mean value after 12 months was not significantly different from that before treatment ().
Table 2 Changes in exophthalmos values and orbital tissue volume from before to after treatment with bimatoprost
Volume of orbital fat and extraocular muscles
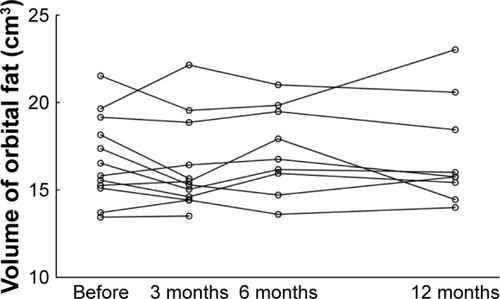
Mean volumes before and after 12 months of treatment are shown in . The mean volume of each tissue after 12 months of treatment was not significantly different from that before treatment ( and ).
Patient dropout
For patients who dropped out, orbital fat volume and exophthalmos values before treatment and at the last MRI examination are shown in and – (one patient was excluded from the table and figures because the TAO developed into an acute inflammatory phase and the extraocular muscles were swelling). Orbital fat volume and exophthalmos values for patients who dropped out were similar before treatment and at the last MRI examination.
Table 3 Exophthalmos values and orbital tissue volume from before treatment to last MRI examination in patients who dropped out
Discussion
Our results indicate that neither the mean exophthalmos value nor mean orbital fat volume decreased significantly after 12 months of treatment with bimatoprost. Previous studies of patients with TAO showed a close relationship between exophthalmos values and volume of orbital fat.Citation30,Citation34 Based on these findings, a decrease in orbital fat is needed to alleviate exophthalmos. Other studies have revealed the effectiveness of surgery (eg, orbital fat decompression) to accomplish this difference.Citation17,Citation18 Richter et alCitation17 reported the effectiveness of transpalpebral decompression. Their mean resected volume of orbital fat was 6.3 cm3, and their mean exophthalmos value decreased by 5.9 mm (from 24.3 mm preoperatively to 18.4 mm postoperatively). It decreased according to the decrease in the orbital fat volume postoperatively. In the current study, we performed a new treatment using noninvasive bimatoprost. Unfortunately, exophthalmos values were not lower after treatment, because orbital fat volume had not decreased.
Although a previous study showed orbital fat atrophy in patients with glaucoma after using bimatoprost,Citation28,Citation29 we did not have the same experience in our patients with TAO. The most important regulators of fat-cell lipolysis are hormones and paracrine factors, such as prostaglandins.Citation35 PGF2α-receptor agonists are potent inhibitors of adipocyte differentiation.Citation36–Citation38 Taketani et alCitation39 reported that PGF2α analogues have the potential to inhibit adipogenesis in vitro through PGF2α-receptor stimulation. The orbital fat atrophy reported in the patients with glaucoma treated with bimatoprost might have occurred by that mechanism. In the current study, however, the volume of orbital fat had not decreased after treatment. Although the reason is unclear, we speculate that the pathophysiology associated with TAO might be different from that associated with glaucoma.
Four of 13 patients dropped out of this study. The reasons were adverse effects and intolerance of bimatoprost because of the development of periocular skin hyperpigmentation and bimatoprost-induced stinging. PAP has been reported more frequently after using bimatoprost than after use of other PGF2α analogues,Citation34,Citation35 hence the dropouts.
The present study has some limitations. First, the sample was small. Although only nine orbits were included in this study, the results showed a similar tendency in all patients, and exophthalmos values and orbital fat volume after 12 months of treatment were not remarkably different from those before treatment. Second, only bimatoprost was used. Other PGF2α analogues, such as latanoprost, were not evaluated in this study. However, it is expected that other PGF2α analogues will be ineffective in reducing exophthalmos in patients with TAO, because the incidence of PAP caused by bimatoprost is higher than that caused by other PGF2α analogues.Citation27,Citation28 Third, we used eyedrops as the method of administration in this study, because previous studies have shown that bimatoprost eyedrops cause enophthalmos in patients with glaucoma.Citation28,Citation29 Actually, bimatoprost eyedrops were ineffective for TAO-induced exophthalmos in the present study. Therefore, because the cause of ineffectiveness in this study might have been eyedrops as the method of administration, it cannot be denied that other methods of bimatoprost administration could be effective. Fourth, cytokines stimulate orbital fibroblasts to produce high levels of PGE2 in patients with TAO, enlarging the volume of orbital fat and extraocular muscle.Citation11,Citation40–Citation42 This mechanism, which differs from that in normal individuals and patients with glaucoma, may be related to that in the present study of bimatoprost (ie, prostaglandin analogues).
In conclusion, mean exophthalmos values and orbital fat volume were not significantly lower after treatment with bimatoprost. Therefore, topical bimatoprost treatment did not reduce exophthalmos or orbital fat in this cohort of patients with inactive TAO.
Author contributions
TH contributed to conception, design, data acquisition, analysis, and interpretation; drafted the article and revised it critically for important intellectual content; provided final approval of the version to be published; and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of the work are appropriately investigated and resolved. MO contributed to the conception and design of the study and the analysis and interpretation of data; revised it critically for important intellectual content; provided final approval of the version to be published; and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of the work are appropriately investigated and resolved.
Acknowledgments
We thank Ms Fumiko Kimura and Ms Yasuyo Hongo for measurements of volume and exophthalmos in this study. This work was supported by JSPS Kakenhi grant JP17K16966. We thank Nancy Schatken, BS, MT (ASCP) and Angela Morben, DVM, ELS from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Disclosure
TH reports grants from JSPS Kakenhi during the conduct of the study, personal fees from Senju Pharmaceutical and Pfizer Japan, grants from Alcon Japan, and grants from Novartis Pharmaceuticals outside the submitted work. MO reports grants and personal fees from Alcon Japan, Novartis Pharmaceuticals, Santen Pharmaceutical, Otsuka Pharmaceutical, Pfizer Japan, Hoya, and Senju Pharmaceutical, and personal fees from Allergan Japan, Bayer, Kowa Pharmaceutical Company, Chuo Sangio, Topcon, RE Medical, and Carl Zeiss Japan outside the submitted work. The authors report no other conflicts of interest in this work.
References
- HattonMPRubinPAThe pathophysiology of thyroid-associated ophthalmopathyOphthalmol Clin North Am200215111311912064074
- El-KaissiSFraumanAGWallJRThyroid-associated ophthalmopathy: a practical guide to classification, natural history and managementIntern Med J200434848249115317547
- SteinJDChildersDGuptaSRisk factors for developing thyroid-associated ophthalmopathy among individuals with Graves diseaseJAMA Ophthalmol2015133329029625502604
- HigashiyamaTNishidaYMorinoKUse of MRI signal intensity of extraocular muscles to evaluate methylprednisolone pulse therapy in thyroid-associated ophthalmopathyJpn J Ophthalmol201559212413025448468
- HigashiyamaTIwasaMOhjiMQuantitative analysis of inflammation in orbital fat of thyroid-associated ophthalmopathy using MRI signal intensitySci Rep2017711687429203853
- MurakamiYKanamotoTTuboiTMaedaTInoueYEvaluation of extraocular muscle enlargement in dysthyroid ophthalmopathyJpn J Ophthalmol200145662262711754905
- PrummelMFBakkerAWiersingaWMMulti-center study on the characteristics and treatment strategies of patients with Graves’ orbitopathy: the first European Group on Graves’ Orbitopathy experienceEur J Endocrinol2003148549149512720530
- BahnRSGraves’ ophthalmopathyN Engl J Med2010362872673820181974
- HiromatsuYEguchiHTaniJKasaokaMTeshimaYGraves’ ophthalmopathy: epidemiology and natural historyIntern Med201453535336024583420
- LehmannGMFeldonSESmithTJPhippsRPImmune mechanisms in thyroid eye diseaseThyroid200818995996518752427
- BartalenaLBaldeschiLDickinsonAConsensus statement of the European Group on Graves’ Orbitopathy (EUGOGO) on management of GOEur J Endocrinol2008158327328518299459
- TortoraFPrudenteMCirilloMDiagnostic accuracy of short-time inversion recovery sequence in graves’ ophthalmopathy before and after prednisone treatmentNeuroradiology201456535336124573324
- HigashiyamaTNishidaYOhjiMRelationship between magnetic resonance imaging signal intensity and volume of extraocular muscles in thyroid-associated ophthalmopathy with methylprednisolone pulse therapyClin Ophthalmol20161072172927143850
- BartalenaLBaldeschiLBoboridisKThe 2016 European thyroid association/european group on graves’ orbitopathy guidelines for the management of graves’ orbitopathyEur Thyroid J20165192627099835
- HigashiyamaTNishidaYOhjiMChanges of orbital tissue volumes and proptosis in patients with thyroid extraocular muscle swelling after methylprednisolone pulse therapyJpn J Ophthalmol201559643043526321629
- OhtsukaKSatoAKawaguchiSHashimotoMSuzukiYEffect of high-dose intravenous steroid pulse therapy followed by 3-month oral steroid therapy for graves’ ophthalmopathyJpn J Ophthalmol200246556356712457917
- RichterDFStoffAOlivariNTranspalpebral decompression of endocrine ophthalmopathy by intraorbital fat removal (Olivari technique): experience and progression after more than 3000 operations over 20 yearsPlast Reconstr Surg2007120110912317572552
- PratMCBraunsteinALDagi GlassLRKazimMOrbital fat decompression for thyroid eye disease: retrospective case review and criteria for optimal case selectionOphthalmic Plast Reconstr Surg201531321521825198394
- SmithTJKahalyGJEzraDGTeprotumumab for thyroid-associated ophthalmopathyN Engl J Med2017376181748176128467880
- WangKXuLYuanZIntraocular pressure-lowering efficacy and safety of bimatoprost 0.03% therapy for primary open-angle glaucoma and ocular hypertension patients in ChinaBMC Ophthalmol2014142124568617
- LiTLindsleyKRouseBComparative effectiveness of first-line medications for primary open-angle glaucoma: a systematic review and network meta-analysisOphthalmology2016123112914026526633
- YangHKParkKHKimTWKimDMDeepening of eyelid superior sulcus during topical travoprost treatmentJpn J Ophthalmol200953217617919333704
- YoshinoTFukuchiTToganoTEyelid and eyelash changes due to prostaglandin analog therapy in unilateral treatment casesJpn J Ophthalmol201357217217823208023
- SakataRShiratoSMiyataKAiharaMIncidence of deepening of the upper eyelid sulcus on treatment with a tafluprost ophthalmic solutionJpn J Ophthalmol201458221221724390604
- NakakuraSYamamotoMTeraoEProstaglandin-associated periorbitopathy in latanoprost usersClin Ophthalmol20159515625565768
- RabinowitzMPKatzLJMosterMRUnilateral prostaglandin-associated periorbitopathy: a syndrome involving upper eyelid retraction distinguishable from the aging sunken eyelidOphthalmic Plast Reconstr Surg201531537337825393907
- InoueKShiokawaMWakakuraMTomitaGDeepening of the upper eyelid sulcus caused by 5 types of prostaglandin analogsJ Glaucoma201322862663122936280
- KucukevciliogluMBayerAUysalYAltinsoyHIProstaglandin associated periorbitopathy in patients using bimatoprost, latanoprost and travoprostClin Exp Ophthalmol201442212613123844550
- JayaprakasamAGhazi-NouriSPeriorbital fat atrophy – an unfamiliar side effect of prostaglandin analoguesOrbit201029635735921158579
- NishidaYTianSIsbergBSignificance of orbital fatty tissue for exophthalmos in thyroid-associated ophthalmopathyGraefes Arch Clin Exp Ophthalmol2002240751552012136278
- TianSNishidaYIsbergBLennerstrandGMRI measurements of normal extraocular muscles and other orbital structuresGraefes Arch Clin Exp Ophthalmol2000238539340410901470
- NishidaYTianSIsbergBTallstedtLLennerstrandGMRI measurements of orbital tissues in dysthyroid ophthalmopathyGraefes Arch Clin Exp Ophthalmol20012391182483111789862
- LennerstrandGTianSIsbergBMagnetic resonance imaging and ultrasound measurements of extraocular muscles in thyroid-associated ophthalmopathy at different stages of the diseaseActa Ophthalmol Scand200785219220117305734
- PeysterRGGinsbergFSilberJHAdlerLPExophthalmos caused by excessive fat: ct volumetric analysis and differential diagnosisAJR Am J Roentgenol198614634594643484861
- ArnerPHuman fat cell lipolysis: biochemistry, regulation and clinical roleBest Pract Res Clin Endocrinol Metab200519447148216311212
- MillerCWCasimirDANtambiJMThe mechanism of inhibition of 3T3-L1 preadipocyte differentiation by prostaglandin F2alphaEndocrinology199613712564156508940395
- SerreroGLepakNMProstaglandin F2alpha receptor (FP receptor) agonists are potent adipose differentiation inhibitors for primary culture of adipocyte precursors in defined mediumBiochem Biophys Res Commun199723312002029144422
- LiuLClipstoneNAProstaglandin F2alpha inhibits adipocyte differentiation via a G alpha q-calcium-calcineurin-dependent signaling pathwayJ Cell Biochem2007100116117316888802
- TaketaniYYamagishiRFujishiroTActivation of the prostanoid FP receptor inhibits adipogenesis leading to deepening of the upper eyelid sulcus in prostaglandin-associated periorbitopathyInvest Ophthalmol Vis Sci20145531269127624508785
- HanRTsuiSSmithTJUp-regulation of prostaglandin E2 synthesis by interleukin-1beta in human orbital fibroblasts involves coordinate induction of prostaglandin-endoperoxide H synthase-2 and glutathione-dependent prostaglandin E2 synthase expressionJ Biol Chem200227719163551636411847219
- KoumasLSmithTJPhippsRPFibroblast subsets in the human orbit: Thy-1+ and Thy-1– subpopulations exhibit distinct phenotypesEur J Immunol200232247748511813166
- FangSHuangYZhongSRegulation of orbital fibrosis and adipogenesis by pathogenic th17 cells in graves orbitopathyJ Clin Endocrinol Metab2017102114273428328938397