Abstract
Sarcoidosis is a multi-system disease characterized by the presence of non-caseating epithelioid granulomas in affected tissues and the most frequent cause of noninfectious uveitis in Japan. Ocular manifestations of sarcoid uveitis vary enormously and commonly characterized by granulomatous anterior uveitis, intermediate uveitis, and posterior uveitis such as retinal periphlebitis, choroiditis, optic nerve granuloma and papillitis. However, case reports of multiple granuloma formation related to sarcoid uveitis is uncommon. This report describes the use of optical coherence tomography angiography to visualize changes occurring in granuloma formation in deeper retinal plexus before and after systemic corticosteroid treatment.
Introduction
Sarcoidosis is an inflammatory disorder of unknown etiology that commonly involves the lungs, lymph nodes, skin, and eyes. It is characterized histologically by the presence of noncaseating granulomas. On standard ophthalmic examinations and fluorescein angiography, intraocular manifestations vary enormously and commonly include granulomatous anterior uveitis, intermediate uveitis, “snow balls” and “string of pearls” vitreous opacities, retinal periphlebitis, choroiditis, papillitis, and optic nerve granuloma.Citation1,Citation2 Fluorescein angiography, the gold standard for visualizing retinal vasculature, has limited depth resolution.Citation3 Use of optical coherence tomography (OCT) angiography provides noninvasive high-resolution, depth-resolved en face images of the retinal capillary microvasculature at different levels of the retina, allowing simultaneous visualization of blood flow and structure.Citation4 However, OCT angiography imaging of retinal granulomas in the setting of sarcoidosis has not been reported previously. To our knowledge, this report describes for the first time the localization of granuloma-like formation in deeper retinal plexus, but not superficial plexus, of a patient with ocular sarcoidosis.
Case report
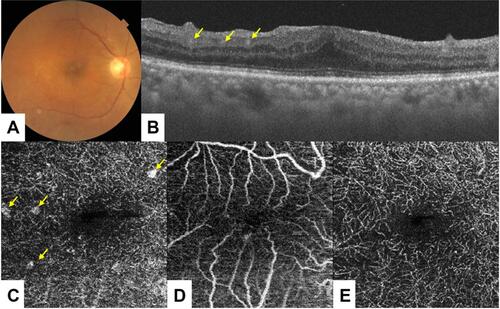
A-74-year-old female with recently diagnosed biopsy-supported systemic sarcoidosis involving the lungs presented with decreased vision and metamorphopsia in the right eye over a 6-month period. Best corrected visual acuity (BCVA) was 10/20 in the right eye and 20/20 in the left eye. Fundus examination of the right eye was unremarkable (). En face OCT angiography demonstrated small round areas of hyperreflectivity in the deeper capillary plexus of the right eye, likely to be granuloma lesions ( and ). However, the superficial capillary plexus appeared to be within normal limits (). OCT angiography of the affected right eye at 2 months follow-up after systemic corticosteroid treatment demonstrated resolution of these lesions (), and BCVA was 20/20 in the right eye. The patient has provided written informed consent for publication of the case details. This case report did not require Institutional Review Board/Ethics Committee approval.
Figure 1 A 74-year-old woman presented with a six-month history of ocular sarcoidosis. Fundus examination of the right eye was unremarkable (A). On spectral-domain OCT and 3×3 mm macular cube OCT angiography conducted in the right eye, however, granulomatous-like lesions were evident in the deeper retinal plexus (B, C: yellow arrow), but not in the superficial plexus (D). After systemic corticosteroid treatment, these lesions were resolved completely (E).
Conclusion
OCT angiography is useful for demonstrating the morphologic characteristics of granulomas and evaluating treatment response.
Acknowledgment
This study was supported by a Grants-in-Aid for Scientific Research (C) 16K11330 from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Disclosure
None of the authors has any financial/conflicting interests to disclose in this work.
References
- Herbort CP, Rao NA, Mochizuki M, et al. International criteria for the diagnosis of ocular sarcoidosis: results of the first international workshop on ocular sarcoidosis (IWOS). Ocul Immunol Inflamm. 2009;17:160–169. doi:10.1080/09273940902818861
- Pasadhika S, Rosenbaum JT. Ocular sarcoidosis. Clin Chest Med. 2015;36:669–683. doi:10.1016/j.ccm.2015.08.009
- Weinhaus RS, Burke JM, Delori FC, Snodderly DM. Comparison of fluorescein angiography with microvascular anatomy of macaque retinas. Exp Eye Res. 1995;61:1–16.
- Nagiel A, Sadda SR, Sarraf D. A promising future for optical coherence tomography angiography. JAMA Ophthalmol. 2015;133:629–630. doi:10.1001/jamaophthalmol.2015.0668
