Abstract
Background
The causes of persistent submacular detachment after successful rhegmatogenous retinal detachment (RRD) surgery remain unknown. Its presence is associated with poor postoperative visual acuity, but due to its spontaneous resolution no additional therapeutic or diagnostic procedure is recommended.
Case report
A case of central serous chorioretinopathy (CSC) that simulated persistent subfoveal fluid after RRD surgery is presented.
Conclusion
To the authors’ knowledge, no other case of visual impairment after successful retinal detachment surgery due to CSC has been reported in the PubMed database. In view of this report, CSC should be considered in the differential diagnosis of persistent subretinal fluid after successful retinal detachment surgery.
Introduction
Persistent submacular fluid after successful rhegmatogenous retinal detachment (RRD) surgery is associated with poor initial visual outcome.Citation1 Its spontaneous resolution may take several months and no additional procedure is recommended to accelerate its natural course as it does not seem to influence the final visual acuity.Citation2,Citation3 The causes of persistent foveal detachment are unclear; however, its incidence is more often significantly reduced after vitrectomy and gas surgery than after scleral buckle procedure.Citation1,Citation2
Central serous chorioretinopathy (CSC) is an idiopathic serous detachment of the macula related to increased adrenergic and steroidal stimulation state and has been reported secondary to different surgical procedures.Citation4–Citation6
A case of CSC misdiagnosed as persistent subretinal fluid after successful retinal detachment surgery, with no spontaneous improvement over an 18-month period, is reported here.
Case report
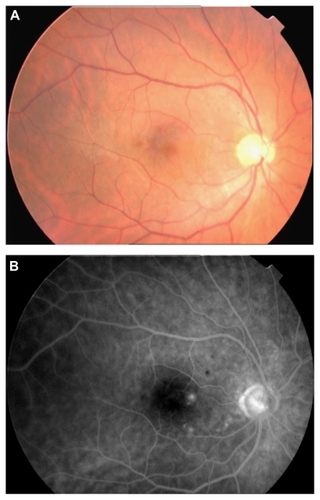
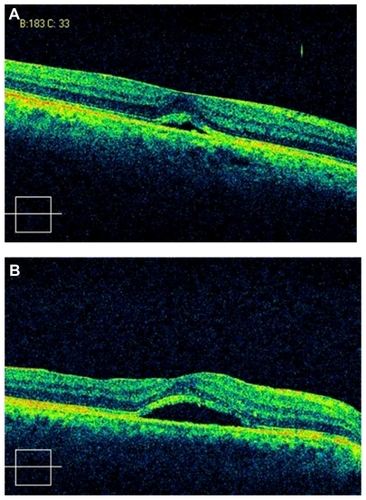
A 48-year-old phakic man underwent successful pars plana vitrectomy and encircling buckle for a 360° macula-off RRD in his right eye. Preoperative best corrected visual acuity was light perception. The patient was started postoperatively on prednisolone drops five times per day in a decreasing dosage for the following 5 weeks. At the 5-month visit, best corrected visual acuity was 0.4 in his right eye and persistent submacular fluid was identified on spectral-domain optical coherence tomography () with an increased epimacular signal that was believed to be a thickened internal limiting membrane. To relieve tangential macular tractions, which might have accounted for the persistent foveal detachment, the patient underwent a second vitrectomy with internal limiting membrane peeling and long-lasting gas. One month later, an increase in subretinal fluid was noted (). Fundus fluorescein angiography revealed two retinal pigment epithelium leaking points in the juxtafoveolar area, which led to the diagnosis of CSC ().
Figure 1 (A) Spectral-domain optical coherence tomography of the right eye of the patient 5 months after vitrectomy and buckle surgery for retinal detachment showing subretinal fluid in the foveal area with thickened inner limiting membrane; (B) inner limiting membrane subfoveal fluid accumulation persisted 2 weeks after peeling.
Discussion
The presence of submacular fluid after successful retinal detachment surgery is associated with poor postoperative visual acuity. No additional therapeutic procedure is recommended due to its spontaneous resolution, which can take up to 18 months and is accompanied by slow visual improvement. Optical coherence tomography is useful in detecting persistent subretinal fluid, which is otherwise difficult to identify on clinical examination.Citation2,Citation7
The causes of persistent submacular detachment after successful retinal detachment surgery remain unknown.Citation1–Citation3 Its incidence seems to be higher after scleral buckling surgery than after vitrectomy surgery (55% versus 15%).Citation1,Citation2 Complete drainage of subretinal fluid during pars plana vitrectomy plus the displacement of fluid by a large gas bubble have been proposed to explain such differences.Citation1 However, no definitive mechanism has been established.
In the patient discussed, CSC simulated persistent subfoveal fluid after RRD surgery. Fundus fluorescein angiography, which is not routinely performed in this setting, revealed retinal pigment epithelium leaking points underlying the detached fovea. It has been proposed that CSC is more likely in patients having type A personality and when its occurrence is preceded by a variety of stressful events in a patient’s life.Citation4–Citation6 CSC in the patient discussed here could have worsened after the second vitrectomy since subretinal fluid increased after internal limiting membrane peeling. Another explanation for the clinical course of this patient could be the persistence of subretinal fluid after RRD repair and the developing of CSC following macular surgery.
Conclusion
To the authors’ knowledge, no other case of visual impairment after successful retinal detachment surgery due to CSC has been reported in the PubMed database. In view of this report, CSC should be considered in the differential diagnosis of persistent subretinal fluid after successful retinal detachment surgery. This disease is associated with increased levels of catecholamines (stress) and glucocorticoids (steroidal medication), both related to ocular surgery for RRD.
Disclosure
The authors report no conflicts of interest in this work.
References
- BensonSESchlottmannPGBunceCXingWCharterisDGOptical coherence tomography analysis of the macula after vitrectomy surgery for retinal detachmentOphthalmology200611371179118316647127
- AbouzeidHBeckerKHolzFGWolfensbergerTJSubmacular fluid after encircling buckle surgery for inferior macula-off retinal detachment in young patientsActa Ophthalmol2009871969918537932
- SeoJHWooSJParkKHYuYSChungHInfluence of persistent submacular fluid on visual outcome after successful scleral buckle surgery for macula-off retinal detachmentAm J Ophthalmol2008145591592218329625
- FawziAACunninghamETJrCentral serous chorioretinopathy after bone marrow transplantationAm J Ophthalmol2001131680480511384585
- LimMCChanTKCentral serous chorioretinopathy following LASIK for hyperopiaJ Refract Surg200824665165218581795
- MondalLBasuSBaidyaKBhaduriGCentral serous chorioretinopathy after dacryocystorhinostomy operation on the same sideIndian J Ophthalmol2009571575819075414
- BensonSESchlottmannPGBunceCXingWCharterisDGOptical coherence tomography analysis of the macula after scleral buckle surgery for retinal detachmentOphthalmology2007114110811217095091