Abstract
Objective
To compare the pattern of intraocular pressure (IOP) reduction following selective laser trabeculoplasty (SLT) versus argon laser trabeculoplasty (ALT) in open-angle glaucoma (OAG) patients, and to investigate the ability of initial IOP reduction to predict mid-term success.
Methods
A prospective, nonrandomized, interventional case series was carried out. Consecutive uncontrolled OAG glaucoma patients underwent SLT or ALT; the same preoperative medical regimen was maintained during follow-up. Data collected included age, type of OAG, pre- and postoperative IOP, number of glaucoma medications, and surgical complications. Post-treatment assessments were scheduled at day 1 and 7 and months 1, 3, and 6.
Results
A total of 45 patients (45 eyes) were enrolled [SLT group (n = 25); ALT group (n = 20)]. Groups were similar for age, baseline IOP, and number of glaucoma medications (P ≥ 0.12). We found no significant differences in mean IOP reduction between SLT (5.1 ± 2.5 mmHg; 26.6%) and ALT (4.4 ± 2.8 mmHg; 22.8%) groups at month 6 (P = 0.38). Success rates (IOP ≤ 16 mmHg and IOP reduction ≥25%) at last follow-up visit were similar for SLT (72%) and ALT (65%) groups (P = 0.36). Comparing the pattern of IOP reduction (% of IOP reduction at each visit) between groups, we found a greater effect following SLT compared with ALT at day 7 (23.7% ± 13.7% vs 8.1% ± 9.5%; P < 0.001). No significant differences were observed at other time points (P ≥ 0.32). Additionally, the percentage of IOP reduction at day 7 and at month 6 were significantly correlated in the SLT group (R2 = 0.36; P < 0.01), but not in the ALT group (P = 0.89). Early postoperative success predicted late success in most SLT cases (82%). No serious complications were observed.
Conclusion
Although mid-term results suggest SLT and ALT as effective and equivalent alternatives, a greater initial IOP reduction was observed following SLT. In addition, the initial IOP reduction was a good predictor of mid-term success in patients undergoing SLT, but not ALT.
Introduction
Laser trabeculoplasty has become an important tool in the treatment of open-angle glaucoma (OAG). This procedure reduces intraocular pressure (IOP) by improving the facility of outflow. In 1979, Wise and WiterCitation1 demonstrated that argon laser trabeculoplasty (ALT) was able to reduce IOP.Citation1,Citation2 They postulated that thermal energy produced by pigment absorption of laser light caused shrinkage of collagen in the trabecular lamellae and believed that the subsequent shortening of treated trabecular meshwork (TM) might enlarge existing spaces between 2 treatment sites or expand Schlemm’s canal by pulling the meshwork centrally. Traditionally, ALT has been performed using the blue-green, bichromatic wavelength spectrum (454.5 to 528.7 nm). As a main side effect, thermal damage induced by argon laser can lead to synechiae formation in the anterior chamber angle.Citation3
More recently (1995), a frequency-doubled q-switched neodymium:yttrium–aluminum–garnet (Nd:Yag) laser was developed to lower IOP in patients with glaucoma by selectively targeting the pigmented cells in the TM without causing thermal or collateral damage to nonpigmented cells or adjacent structures.Citation4–Citation7 Selective laser trabeculoplasty (SLT) delivers 80 to 100 times less energy than ALT, preserving the TM architecture in animal models, and it is potentially repeatable.Citation8,Citation9
Several studies have compare ALT with SLT, in terms of IOP reduction and medical dependency, showing equivalent short-term success.Citation10–Citation14 In this study, we sought to compare the pattern of IOP reduction (% of IOP reduction at each time point) following SLT versus ALT in treated OAG patients. In addition, we evaluated the ability of initial IOP reduction to predict mid-term success.
Methods
This prospective, nonrandomized, interventional study followed the tenets of the Declaration of Helsinki and was approved by the institutional review board. Written informed consent was obtained from all patients.
Patients
Patients included in this study were enrolled from 3 different centers: the Glaucoma Unit of the Federal University of São Paulo, Hospital Medicina dos Olhos and CERPO. All patients had OAG with uncontrolled IOP (individualized for each patient, based on the level of glaucomatous damage) on maximal tolerated medical treatment and age >18 years.
Exclusion criteria were visual field defect within 10° of fixation, previous laser or incisional glaucoma surgery, corneal disease, history of steroid use, and any patient who required more than 25% of IOP reduction to reach target IOP.
Procedures
Data collected included age, type of OAG, preoperative and postoperative IOP, number of glaucoma medications, gonioscopy appearance, surgical complications, and any subsequent related events.
Both ALT and SLT were performed under topical anesthesia. In the SLT group a frequency-doubled Q-switched Nd:YAG laser (Laserex Tango™ Nd:YAG, Ellex Medical, Australia) emitting at 532 nm with pulse duration of 3 nanoseconds and a spot size of 400 μm coupled to a slit- lamp delivery system. A Goldmann 3-mirror goniolens was placed on the eye with 1% methylcellulose. The aiming beam was focused onto the pigmented TM. The 400 μm spot size was large enough to irradiate the entire anteroposterior height of the TM. In all eyes, approximately 50 adjacent but nonoverlapping laser spots were placed over the inferior 180° of the TM. Initial energy level was set to 0.80 mJ and changed according to the level of TM pigmentation. The end point of each laser application was minibubble formation. In ALT group the patients were treated with a coherent argon laser with the blue-green (Ophthalas, Argon green laser™, Alcon, Fort Worth, TX) biochromatic wavelength spectrum (454.5 to 528.7 nm), with a 0.1-second pulse duration and a spot size of 50 μm coupled to a slitlamp delivery system. A Goldmann 3-mirror goniolens was placed on the eye with 1% methylcellulose. The aiming beam was focused onto the pigmented TM. Initial energy level was set to 400 mW and changed according to the level of TM pigmentation. The end point of each laser application was minibubble formation or focal tissue whitening. From 400 to 1000 mW of energy was delivered. For comparison, 1 Joule is equivalent to 1 Watt*second. Forty-five to 55 adjacent nonoverlapping spots were applied to the inferior 180° of the TM. Brimonidine 0.2% was instilled before and after the procedures, and 1% prednisolone acetate or 0.1% dexamethasone acetate was administrated 4 times a day for 5 days.
All the procedures were done by the same (experienced) surgeon. Patients were maintained on the same antiglaucoma drugs before and after laser treatment. Post-treatment assessments were scheduled at week 1 and months 1, 3, and 6. Visits occurred around the same time of day, whenever possible, to account for diurnal IOP fluctuation. Main outcomes were the pattern of IOP reduction (% of IOP reduction at each time point) following SLT versus ALT, and the ability of initial IOP reduction (day 7) to predict late success (month 6).
Statistical analysis
Independent samples t-test was used to compare the magnitude of IOP reduction between groups. Regression analysis was used to correlate initial and late IOP reduction in each group. Frequency data were analyzed using chi-square test.
Results
A total of 45 consecutive patients were enrolled, 25 patients in SLT group (25 eyes) and 20 patients in the ALT group (20 eyes). Most patients had primary OAG (86%). Groups were similar for age, gender, race, mean preoperative IOP, and number of glaucoma medications (P ≥ 0.09). Pretreatment demographic and clinical characteristics of study patients are provided in .
Table 1 Clinical characteristics of study patients
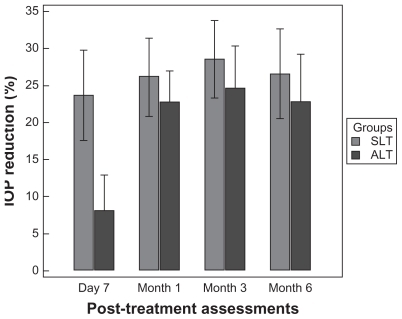
We found no significant difference in mean IOP reduction between SLT (5.1 ± 2.5 mmHg; 26.6%) and ALT (4.4 ± 2.8 mmHg; 22.8%) groups at 6 months (P = 0.38). Success rates (defined as IOP ≤ 16 mmHg and IOP reduction ≥25%) at last follow-up visit were also similar for SLT (72%) and ALT (65%) groups (P = 0.36). Comparing the IOP reduction pattern (% of IOP reduction at each time point; and ) between groups, we found a greater IOP reduction following SLT compared with ALT at day 7 (23.7% ± 13.7% vs 8.1% ± 9.5%; P < 0.001). No significant differences were observed at the other time points (P ≥ 0.32).
Figure 1 Intraocular pressure values (mmHg) at each time point. Comparison between argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT) groups.
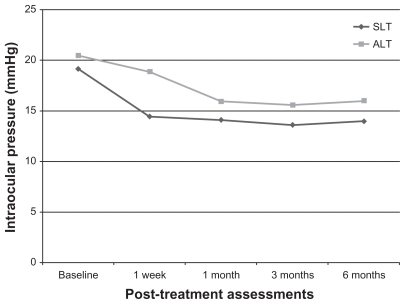
Figure 2 Percentage of intraocular pressure (IOP) reduction at each time point. Comparison between argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT) groups. Means and error bars (95% CI) are provided.
The percentage of initial IOP reduction at (day 7) correlated significantly with IOP reduction at month 6 in the SLT group (R2 = 0.36; P < 0.01), but not in the ALT group (P = 0.89). In addition, early postoperative success (at day 7) predicted late success (at month 6) in most cases treated with SLT (82%), but only in 29% of those treated with ALT.
Finally, 1 patient developed sustained IOP rise (≥10% IOP increase in 2 consecutive visits) in each group. The patient from the ALT group was relatively young and had significant visual field damage. Consequently, he was later submitted to a trabeculectomy with mitomycin-C. After the last follow-up visit, IOP values were close to baseline IOP in the patient from the SLT group. This patient is currently being followed. No cases of peripheral synechiae development or other serious complications were observed.
Discussion
Both ALT and SLT are procedures frequently used in OAG treatment. Most previously published studies focused primarily on the magnitude of IOP reduction, and reported similar results for the two treatment modalities. As far as we know, this is the first study to compare the pattern of IOP reduction between ALT and SLT, and to report on the ability of initial IOP reduction to predict mid-term success.
In this study, comparing the IOP-lowering efficacy of ALT and SLT in treated OAG patients, we found no significant difference between groups after 6 months. Our results are in agreement with previously published data. Damji et al found similar results at 6 months evaluating a sample of 36 eyes.Citation12 A prospective study by Hollo,Citation15 in which patients underwent ALT in 1 eye and SLT in the fellow eye, found equivalent outcomes. Another prospective study by Martinez-de-la-Casa et alCitation9 treated consecutive patients with SLT (20 eyes) and ALT (20 eyes). After 6 months, a similar reduction in IOP was observed. Finally, in a larger series (176 eyes), Damji et alCitation16 reported equivalent success rates (IOP reduction ≥20%) between treatments after 6 months.
The main outcome measurement of our study was the analysis of the pattern of IOP reduction. There are no previously published data on this topic. Comparing the magnitude of IOP reduction at each time point following laser treatment, initial IOP reduction (day 7) was greater in the SLT group. In addition, this initial outcome was a significant predictor of mid-term success for these patients, but not for those treated with ALT. One could hypothesize that this difference could be related to the specific action of the selective laser in the pigmented cells of the TM. While SLT stimulates aqueous outflow without structural damage to the TM, ALT firstly requires structural damage and subsequent tissue healing to increase outflow facility, which may need a longer period to occur.Citation1,Citation7,Citation17 Our findings suggest that SLT seems to be a better option in patients requiring a faster IOP reduction following laser trabeculoplasty.
There are some specific characteristics of our study that should be considered while interpreting its findings. First, although prospective, it was not randomized. Second, its sample size was limited. A larger sample might have revealed different outcomes. Finally, a study with a longer follow-up is warranted in order to confirm the pattern of IOP reduction we found for each laser modality.
Conclusion
In summary, these mid-term results suggest SLT and ALT as safe, effective, and equivalent alternatives for IOP reduction in treated OAG patients. A greater initial (first week) IOP-lowering effect was observed following SLT. In addition, the initial IOP reduction was a good predictor of mid-term success in patients undergoing SLT, but not ALT. These findings add to our previous knowledge on laser treatment, and should be considered while indicating and following patients undergoing laser trabeculoplasty.
Disclosure
None of the authors have any commercial interest regarding the present study.
References
- WiseJBWitterSLArgon laser therapy for open-angle glaucoma: a pilot studyArch Ophthalmol1979972319322575877
- The Glaucoma Laser Trial Research GroupThe Glaucoma Laser Trial (GLT) and Glaucoma Laser Trial Follow up study: 7. ResultsAm J Ophthamol19951206718731
- EguchiSYamashitaHYamamotoTShiratoSKitazawaYMethods of argon laser trabeculoplasty, complications and long-term follow-up of the resultsJpn J Ophthalmol19852921982114046228
- JuzychMSChopraVBanittMRComparison of long-term outcomes of selective laser trabeculoplasty versus argon laser trabeculoplasty in open-angle glaucomaOphthalmology2004111101853185915465546
- LatinaMAParkCSelective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactionsExp Eye Res19956043593717789416
- LatinaMASibayanSAShinDHNoeckerRJMarcellinoGQ-switched 532-nm Nd:YAG laser trabeculoplasty (Selective Laser Trabeculoplasty)Ophthalmology199810511208220909818610
- KramerTRNoeckerRJComparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyesOphthalmology2001108477377911297496
- AndersonRRParrishJASelective photothermolysis: precise microsurgery by selective absorption of pulsed radiationScience198322045965245276836297
- Martinez-de-la-CasaJGarcia-FeijooJCastilloASelective vs argon laser trabeculoplasty: hypotensive efficacy, anterior chamber inflammation, and postoperative painEye200418549850215131681
- DamjiKFShahKCRockWJBainsHSHodgeWGSelective laser trabeculoplasty v argon laser trabeculoplasty: a prospective randomised clinical trialBr J Ophthalmol199983671872210340983
- LanzettaPMenchiniUVirgiliGImmediate intraocular pressure response to selective laser trabeculoplastyBr J Ophthalmol1999831293210209430
- DamjiKFBovellAMHodgeWGSelective laser trabeculoplasty: a review and comparison to argon laser trabeculoplastyOphthalmic Pract2003215458
- MelamedSBen SimonGLevkovitch-VerbinHSelective laser trabeculoplasty as primary treatment for open-angle glaucoma: a prospective, non-randomised pilot studyArch Ophthalmol20031217956960
- CvenkelBOne-year follow-up of selective laser trabeculoplasty in open angle glaucomaOphthalmologica20042181202514688431
- HolloGArgon and low energy, pulsed Nd:YAG laser trabeculoplasty. A prospective, comparative clinical and morphological studyActa Ophthalmol Scand19967421261318739675
- DamjiKFBovellAMHodgeWGSelective laser trabeculoplasty versus argon laser trabeculoplasty: results from a 1-year randomized clinical trialBr J Ophthalmol200690121490149416899528
- NoeckerRJKramerTRComparison of the acute morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyesOphthalmology2001108477377911297496