Abstract
Purpose:
To describe a case of choroidal osteoma with choroidal neovascularization (CNV) that was successfully treated with two intravitreal injections of bevacizumab (IVB).
Design and methods:
Case report on a 12-year-old Japanese girl who presented with a sudden decrease in vision in her left eye. At the first visit, 2 days after the onset of her symptoms, her visual acuity (VA) in her left eye was 0.2. Ophthalmoscopy showed a hemorrhage of 5 disc diameters under the retinal pigment epithelium and a serous retinal detachment at the posterior pole of the left eye. These findings were confirmed by optical coherence tomography. Fluorescein angiography (FA) and indocyanine green angiography (ICGA) showed several points of leakage around the fovea, which suggested a CNV. From these findings, the patient was diagnosed with choroidal osteoma with a CNV. The submacular hemorrhage was from the CNV associated with the choroidal osteoma. We treated her with two injections of 1.25 mg/0.05 mL IVB with a 4-month interval.
Results:
The patient’s VA in her left eye improved to 0.7, and this vision was maintained for 4 years. The CNV disappeared in the FA and ICGA images and no recurrence was observed after 4 years.
Conclusion:
Our findings indicate that IVB is effective in resolving CNV in eyes with an osteoma and prevents a decrease of vision in eyes with a choroidal osteoma with a CNV.
Keywords:
Introduction
A choroidal osteoma is a rare and benign choroidal tumor, and its clinical and histopathological features were first reported by Gass et al.Citation1 Choroidal osteomata are seen in the peripapillary and macular areas of young healthy girls. The striking features of a choroidal ostroma are: well defined mass; slightly elevated, white-to-cream or orange lesion as observed by ophthalmoscopy; and high tissue density due to calcification as observed by ultrasonography and computed tomography (CT).
Choroidal osteomata usually grow very slowly, but some patients have an acute decrease in vision. The main causes of this sudden decrease in vision are a serous macular detachment or a subretinal hemorrhage, with or without choroidal neovascularization (CNV). A definitive treatment for the CNV associated with a choroidal osteoma has not been established. Photocoagulation,Citation2,Citation3 surgical removal of the CNV,Citation4 photodynamic therapy (PDT),Citation5–Citation7 and transpupillary thermotherapy (TTT)Citation8,Citation9 have been tried, but long-term vision is usually not well preserved.
Intravitreal injections of vascular endothelial growth factor (VEGF) antibody (eg, bevacizumab) has been used to block the activity of VEGF in eyes with a CNV associated with age-related macular degeneration (AMD). This therapy has reduced the visual loss and improved visual acuity (VA). Bevacizumab is a full-length VEGF antibody that has been used for off-label treatment of CNVs associated with neovascular AMD.Citation10
Earlier studies have shown that intravitreal bevacizumab (IVB) was effective in resolving the CNV associated with a choroidal osteoma.Citation11–Citation13 But the follow-up periods in these reports were short; that is, from 4 to 10 months.
We report a case of choroidal osteoma with a CNV that was successfully treated with two injections of IVB, and good vision has been maintained for at least 4 years.
Case report
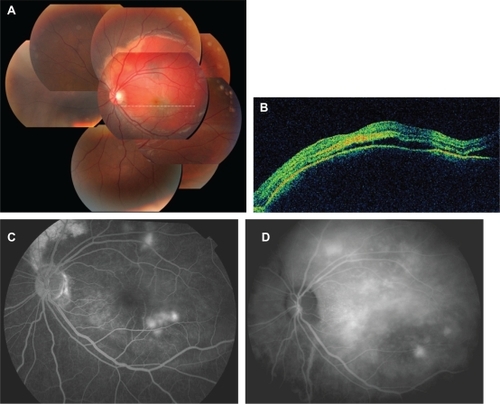
A 12-year-old Japanese girl presented with a sudden decrease of vision in her left eye on November 13, 2006. Her systemic and ophthalmological histories were not significant. At her first visit, 2 days after the onset, her VAs were 1.2 OD and 0.2 OS. The intraocular pressures were within the normal limits in both eyes. Slit-lamp biomicroscopy showed no remarkable changes, including the absence of inflammation of the anterior segments. Ophthalmoscopy showed a 5-disc diameter hemorrhage under the retinal pigment epithelium (RPE) and serous retinal detachment (SRD) at the posterior pole of the left eye (). These findings were confirmed by optic coherence tomography (OCT) (). Fluorescein angiography (FA) showed a mild pooling of dye associated with a pigment epithelium detachment and several points of leakage superior and inferior to the fovea (). Indocyanine green angiography (ICGA) showed leakage lateral and inferior to the fovea, which suggested a CNV (). The ophthalmoscopic, OCT, FA, and ICGA findings were normal in the right eye.
Figure 1 Patient with a choroidal osteoma and choroidal neovascularization before treatment. (A) Fundus photograph showing 5-disc-diameter hemorrhage under the retinal pigment epithelium. (B) Horizontal optical coherence tomographic image, showing pigment epithelial detachment and serous retinal detachment. (C, D) Angiography: fluorescein angiography (C) and indocyanine angiography (D) show several points of dye leakage around the fovea.
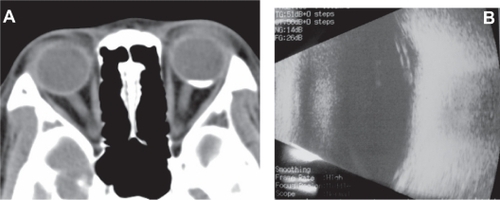
CT showed calcification and a bone-density mass in the posterior pole of the left eye (), but magnetic resonance imaging showed no unusual changes in the intra- and extraocular areas. Ultrasound echography (B-mode) showed a flat convex elevation in the posterior pole of the eye, which produced an acoustic shadow behind the sclera (). Microperimetry showed poor sensitivity with poor focus and fixation (). The serological examinations were negative.
Figure 2 (A) Computed tomographic images of patient with choroidal osteoma, showing calcification and bone-density mass in the posterior pole of the left eye. (B) Ultrasonic echography (B-mode) shows a convex elevation in the posterior pole of the eye, producing an acoustic shadow behind the sclera.
On the basis of these findings, the patient was diagnosed with choroidal osteoma and the submacular hemorrhage was from a CNV associated with the choroidal osteoma. We treated her with 1.25 mg/0.05 mL injection of IVB (Avastin®; Genentech, South San Francisco, CA) after obtaining approval from the Institutional Review Board of Chiba University. Approval was also obtained from the patient and her parents.
The subretinal fluid quickly disappeared 8 days after this treatment, and the elevation of the RPE disappeared. Two months later, her VA improved to 0.6 OS, and the size of the dye leakage was reduced, although not completely. We gave a second IVB injection 4 months after the first treatment, the CNV disappeared, and no recurrence has been observed ().
Figure 3 Patient with a choroidal osteoma and choroidal neovascularization 18 months after two intravitreal injections of bevacizumab. Fundus photograph (A), horizontal optical coherence tomographic scan (B), fluorescein angiography indocyanine angiography (C), and indocyanine angiography (D) all show absence of subretinal fluid and leakage points.
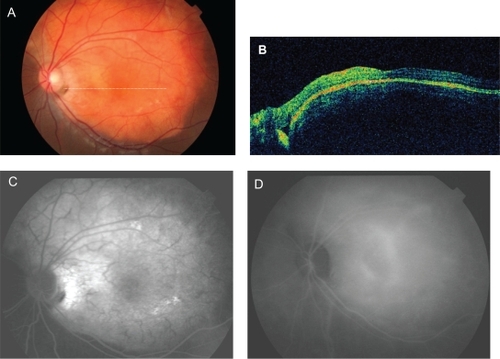
Figure 4 Microperimetric findings. Findings before (A) and 3 years after (B) two intravitreal injections of bevacizumab. Fixation indicated by small blue dots is improved.

The patient was followed for 4 years, and microperimetry showed that the average sensitivities improved from 8.0 dB before, to 6.0 dB at 4 months, 4.8 dB at 6 months, and 10.0 dB at 42 months after the IVB (). At 4 years, her VA remained good at 0.7 OS.
Discussion
A choroidal osteoma is mostly found in healthy young women. Alyward et al reported that 89% of patients with a choroidal osteoma were women with a mean age of 21 years.Citation2 This tumor is usually slow growing but can grow rapidly in some cases.Citation14 One study reported that the VA decreased in 26% of the cases at 5 years and 45% at 10 years.Citation15 In another study, the VA decreased to ≤0.1 in 45% of the cases at 5 years, 56%–58% at 10 years, and 62% at 20 years.Citation2,Citation15
Thus, there is a slow but progressive decrease of vision in eyes with choroidal osteoma, even those treated with photocoagulation.
The long-term visual prognosis of a choroidal osteoma is not good. The decrease in vision is due to SRD, CNV, atrophy of the RPE, or a combination of these. A CNV was found in 31% of the cases at 5 years, 31%–47% at 10 years, and 56% at 20 years.Citation2,Citation15
There is no standard treatment for a choroidal osteoma. Various treatments for CNV have been tried, but the treatments do not usually stop the vision decrease. The results of one study showed that photocoagulation of an extrafoveal classic CNV was successful in 25% of the cases, and the neovascular membrane was eliminated.Citation2 However, photocoagulation can stimulate rapid vascular remodeling and anastomoses in choroidal osteoma.Citation3 Another study reported that the CNV can be surgically removed, but the postoperative VA was poor at 0.06.Citation4
PDT has been partially successful in treating CNV in eyes with choroidal osteoma. Earlier studies show that 6 months after a single PDT the metamorphopsia can resolve completely; in one study the visual acuity was not changedCitation5 and in another study it even improved from 0.1 to 1.0.Citation6 Another study reported that four PDT applications obstructed the CNV completely, but the final VA was 0.17.Citation7
TTT was effective in obstructing the CNV but the visual outcome was also poor. An earlier report indicates that at 10 months after one TTT application, the VA improved from 0.25 to 0.33, and the vision was maintained with a scarred CNV.Citation8 In another report, the final VA was 0.1 after three TTT applications.Citation9
The cause for the development of a CNV in eyes with a choroidal osteoma has not been determined, but it has been hypothesized that tumors with overlying hemorrhage and irregular surface were at greater risk of developing a CNV.Citation15 Because of the long duration of the tumor, the normal tissue may be slightly damaged. In addition, the mild ischemic stress and chronic inflammation of the choroidal membrane and the retina may upregulate the expression of VEGF. The disruption of the RPE and thinning or loss of the Bruch membrane and choriocapillaris might also contribute to the development of a CNV. A thin, degenerated RPE overlying the osteoma allows the growth of new abnormal vessels stimulated by VEGF. Therefore anti-VEGF therapy may be effective under such pathological conditions.
The results of recent studies have suggested that IVB is a good treatment for reducing CNV of choroidal osteomata, with improvements in VA. For example, the VA improved from 0.1 to 0.8 nine months after one injection,Citation11 and from finger counting to 0.16 at 4 months after two injections.Citation12 In another study, the vision improved from finger counting to 0.1 ten months after two injections of IVB.Citation13 In these three reports, the effects of bevacizumab were followed for 4–10 months. In our case, the effects of bevacizumab remained stable for over 4 years.
In our case, the average MP1-determined sensitivities improved from 8.0 dB before to 6.0 dB at 4 months and to 4.8 dB at 6 months after the IVBs. But the average sensitivities decreased to 10.0 dB at 42 months after the IVBs, which was most likely because the retinal sensitivity of the inferior nasal side probably decreased to lower the average sensitivity. RPE atrophy occurred in the inferior nasal region of the macula, and the fovea was not affected. This is why the VA remained good even after the retinal sensitivity decreased. Thus, this disagreement between VA and retinal sensitivity may not be too surprising in some cases. Because the fundus and FA findings showed marked RPE atrophy in the nasal inferior of the retina, the retinal sensitivity of the nasal inferior area could not be improved.
In conclusion, we report a case of choroidal osteoma with a CNV that was successfully treated with two injections of IVB. The vision was maintained at 0.7 for at least 4 years. Our findings indicate that intravitreal injections of bevacizumab may be effective in preventing vision decrease in eyes with a choroidal osteoma with a CNV.
Disclosure
The authors report no conflicts of interest in this work.
References
- GassJDMGuerryRKJackRLHarissGChoroidal osteomaArch Ophthalmol197896428435629679
- AlywardGWChangTSPautlerSEGassJDMA long-term follow-up of choroidal osteomaArch Ophthalmol199811610133713419790633
- BrowningDJChoroidal osteoma. Observations from a community settingOphthalmology200311071327133412867386
- FosterBSFernandez-SuntayJPDryjaTPJakobiecFAD’AmicoDJSurgical removal and histopathologic findings of a subfoveal neovascular membrane associated with choroidal osteomaArch Ophthalmol2003121227327612583798
- Battaglia ParodiMDa PozzoSTotoLSavianoSRavalicoGPhotodynamic therapy for choroidal neovascularization associated with choroidal osteomaRetina200121666066111756892
- BlaisePDuchateauEComhaireYRakicJMImprovement of visual acuity after photodynamic therapy for choroidal neovascularization in choroidal osteomaActa Ophthalmol Scand20058351551616029286
- SinghADTalbotJFUndlePARennieIGChoroidal neovascularization secondary to choroidal osteoma: successful treatment with photodynamic therapyEye20051948248415286675
- SharmaSSirbhargavaNShanmugamMPChoroidal neovascular membrane associated with choroidal osteoma (CO) treated with transpupillary thermo therapyIndian J Ophthalmol2004251232933015693329
- ShuklaDTanawadeGRamasamyKTranspupillary thermotherapy for subfoveal choroidal neovascular membrane in choroidal osteomaEye20062085684716113639
- AveryRLPieramiciDJRabenaMDCastellarinAANasirMAGiustMJINtravitreal bevacizumab (Avastin) for neovascular age-related macular degenerationOphthalmology2006113336337216458968
- AhmadiehHVafiNDramatic response of choroidal neovascularization associated with choroidal osteoma to intravitreal injection of bevacizumab (Avastin)Graefe’s Arch Clin Exp Ophthalmol200724517311733
- NarayananRShahVAIntravitreal bevacizumab in the management of choroidal neovascular membrane secondary to choroidal osteomaEur J Ophthalmol200818346646818465736
- SongWKKohHJKwonOWByeonSHLeeSCIntravitreal bevacizumab for choroidal neovascularization secondary to choroidal osteomaActa Ophthalmol20098710010119178391
- MizotaATanabeRAdachi-UsamiERapid enlargement of choroidal osteoma in a 3-year-old girlArch Ophthalmol1998116112811299715704
- ShieldsCLSunHDemirciHShieldsJAFactors predictive of tumor growth, tumor decalcification, choroidal neovascularization, and visual outcome in 74 eyes with choroidal osteomaArch Ophthalmol2005123121658166616344436