Abstract
Background:
The purpose of the study was to evaluate vitreoretinal interface (VRI) alteration with a short-wavelength scanning laser ophthalmoscope (swSLO), the Nidek F-10, and compare the results with those obtained by means of spectral-domain optical coherence tomography (SD-OCT).
Methods:
Thirty-six eyes were studied (20 patients, mean age 68 ± 12.3 years). All patients underwent a complete ophthalmologic examination, which comprised SD-OCT and Nidek F-10 analysis with short-wavelength blue laser. Eyes were divided into four groups depending on the degree of VRI alteration observed with the swSLO and SD-OCT. Statistical analysis was performed using the Chi-square test. P values less than 0.05 were considered statistically significant.
Results:
OCT analysis: eight eyes (22%) grade 0 (no abnormalities), 15 eyes (42%) grade 1 (preretinal cellophane); seven (19%) grade 2 (preretinal wrinkling); six (17%) grade 3 (macular pucker or hole). Nidek F-10 analysis: seven (19%) grade 0, 16 (45%) grade 1; seven (19%) grade 2; six (17%) grade 3. Chi-square = 0.099, P = 0.992. There was no statistically significant difference between the two instruments.
Conclusion:
Nidek F-10 allows both a quantitative and a qualitative evaluation of VRI and is equal to SD-OCT in detecting alteration of the inner portion of the retina, providing an easy way to evaluate and map differences in the inner vitreoretinal surface.
Introduction
Evaluation of the vitreoretinal interface (VRI) in the macular region is today widely performed using optical coherence tomography (OCT) scans.
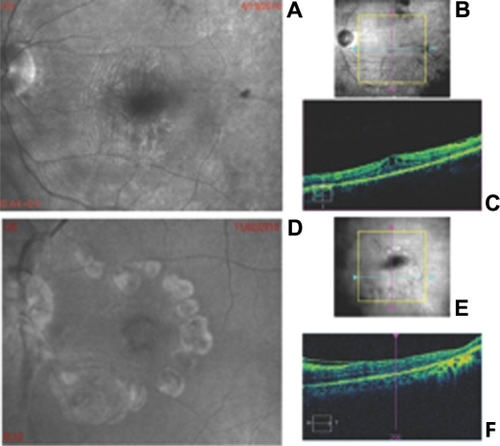
Figure 1 (A) Representative F-10 blue laser imaging of one eye with pre-retinal wrinkling; (B) Infra-red fundus photograph of the same patient showing the position of the scan in image (C); (C) optical coherence tomography scan of the same eye, which shows pre-retinal wrinkling. (D) Representative F-10 blue laser imaging on one eye with macular pucker and macular hole; (E) Infra-red fundus photograph of the same patient showing the position of the scan in image (F); (F) optical coherence tomography of the same eye which shows macular pucker.
Although OCT has provided valuable information on the morphologic features of vitreoretinal interface (VRI) alterations, some problems remain. First of all, the extent of the area of a macular traction is determined by a cross-section of the lesion in the line scan mode of the OCT. This may fail to detect the full extent of a macular alteration unless the scan happens to pass through the entire extent of the lesion. Serial OCT sections are helpful in detecting VRI alteration, but multiple scans require a considerable amount of time, and it is also difficult to obtain serial images in patients with poor fixation because of macular pucker or hole.
NIDEK Co Ltd (Gamagori, Japan) has recently developed a new scanning laser ophthalmoscope (SLO) (Nidek F-10). The Nidek F-10 is able to capture many different images of the retinal fundus thanks to its wide range of available light sources. It is provided with four laser wavelengths (IR 790 nm, red 660 nm, green 532 nm, blue 490 nm). SLO allows retinal examination using blue (490 nm), which is especially useful for vitreoretinal surface and inner retina; red (660 nm) which is capable of imaging deeper tissues; and infrared (790 nm) for choroidal examination.Citation1,Citation2
With focusing to obtain images in direct confocal and indirect modes, SLO can display the reflection of a particular surface on the screen, minimizing the visualization of deeper surfaces.Citation1,Citation2
The purpose of this study was to evaluate whether the short wavelength (blue) laser beam of this new device is able to identify and map areas where the VRI is altered.
Methods
Thirty-six eyes were studied (20 patients, mean age 68 ± 12.3 years) from September 2009 to April 2010. Inclusion criteria were: clear media and no prior surgical intervention. Exclusion criteria were: high myopia (>10D), hyperopia (>3), intraocular pressure (IOP) higher than 25 mmHg, or anterior chamber abnormalities.
A comprehensive ocular examination, including OCT and noninvasive imaging by Nidek F-10 was performed. The Cirrus OCT (Carl Zeiss Meditec, Oberkochen, Germany) was used to detect the presence and the extent of the VRI alteration. The entire area of the posterior fundus within the retinal arcade vessels was scanned carefully with 5-line mode and 512 × 128 volume cube (each image had a 5 μm axial and 10 μm transverse resolution).
After completing the OCT scans of the entire fundus area within the vascular arcade, the fundus was examined using the short wavelength laser of the Nidek F-10 SLO.
In short-wavelength imaging, blue laser light (490 nm) is used to noninvasively scan the fundus under non-mydriatic conditions. The F-10 acquires one photograph of the entire posterior fundus using the blue laser settings in 1–2 seconds.
Patients were divided into four groups depending on the degree of V-R alteration.
Grade 0: no abnormality, Grade 1: pre-retinal cellophane, Grade 2: pre-retinal wrinkling, Grade 3: macular pucker or hole.
One masked examiner graded the OCT and F-10 examination. Statistical analysis was performed with Chi-square test, using SPSS software (v 15; SPSS Inc, Chicago, IL). P values less than 0.05 were considered statistically significant.
Results
According to OCT examination, the eyes were divided into the following: eight eyes (22%) grade 0 (no abnormalities), 15 eyes (42%) grade 1 (pre-retinal cellophane), seven eyes (19%) grade 2 (pre-retinal wrinkling), and six eyes (17%) grade 3 (macular pucker or hole).
According to the F-10 blue laser photographs, the eyes were divided into the following: seven eyes (19%) grade 0, 16 eyes (45%) grade 1, seven (19%) grade 2, and six (17%) grade 3.
The only error was due to the identification of one eye in a higher group because of the presence of high parafoveal reflection in temporal areas not corresponding to high reflectivity of epiretinal layers in OCT scans of the same area. Chi-square test was = 0.099, P = 0.992. There was no statistically significant difference between the two instruments.
Discussion
Previous studies have shown that the scanning laser ophthalmoscope is useful for fluorescein angiography, ophthalmoscopy with a low amount of light, retinal perimetry, and localized retinal acuity testing.Citation3–Citation5
Scanning laser ophthalmoscopy has been used in the diagnosis of VRI abnormalities in combination with other devices. Tammewar et alCitation6 used high resolution coronal-plane optical coherence tomography (OCT) scanning linked with simultaneous scanning laser ophthalmoscope (SLO) imaging obtained with a SLO-OCT (OTI, Montreal, QC). The authors evaluated patients with VRI abnormalities including epiretinal membranes, macular hole, incomplete posterior vitreous detachment, vitreomacular traction syndromes, and diabetic and cystoid macular edema in a retrospective study. In this study the SLO-OCT produced simultaneous SLO and confocal images of the retina and vitreous. Combining the images allowed the identification of traction forces of the epiretinal membrane, contour of the hyaloid membrane and changes in the inner retinal surface. Simultaneously obtained OCT scan and SLO images of the fundus offered exact colocalization of retinal structures and vitreomacular interface abnormalities.
Combining optical coherence tomography and scanning laser ophthalmoscopy (OCT/SLO) longitudinal imaging was used to identify vitreomacular traction, vitreoschisis, and measure retinal thickness.Citation7,Citation8
Past and present imaging methodologies, and new technologies, are currently in development for future research and clinical applications. Histological techniques such as dark field slit microscopy, clinical slit lamp biomicroscopy, standard and scanning laser ophthalmoscopy (SLO), ultrasonography, optical coherence tomography (OCT), combined OCT-SLO, magnetic resonance and Raman spectroscopies, and dynamic light scattering were employed to view uncommon features with mixed results.Citation9 None of them became the standard of care in vitreoretinal surveillance. The author concluded that OCT enables better in vivo visualization of the vitreoretinal interface than SLO and ultrasonography, but does not adequately image the vitreous body and vitreo-retinal interface.
The combination of OCT with SLO provides new imaging capabilities. Better understanding of normal vitreous physiology and structure and how it changes in aging and disease is still a challenge that swSLO may elucidate.
Our data demonstrate that the swSLO has the capacity to show the extension of areas of VRI abnormalities, allowing both quantitative and qualitative evaluation of the alteration. Furthermore, the data are comparable with those obtained with SD-OCT. Blue laser offers a micrometric resolution of the VRI abnormality and can optimize the vitreoretinal imaging especially over the macular area.
We demonstrated that swSLO can offer good sensitivity for the detection of abnormalities of the internal limiting membrane (ILM) and posterior hyaloid, since the blue laser beam is reflected and scattered by these surfaces, resulting in a good view of epiretinal membranes. Radiating retinal folds around the membrane can also be well visualized; additionally, it is possible to make a good estimate of the thickness of the epiretinal membrane using the confocal facility of the scanning laser ophthalmoscope.
The swSLO can highlight the demarcation line where the VRI abnormality starts and ends, and offers images similar to those obtained intraoperatively with a xenon laser, which is very useful for vitreoretinal surgeons. The ophthalmologist can obtain images of the VRI abnormality in 1–2 seconds, whereas a complete OCT scan of the entire posterior fundus within the vascular arcade takes at least 1 minute in patients who can maintain a good fixation during the examination. Furthermore, we can roughly measure the area of the abnormality, follow it over time, superimpose the results of retinal sensitivity obtained with microperimetry on swSLO images (both instruments run with the same software) and study the functionality of the diseased area of the retina.
The main disadvantages of this technique are the high cost of the device and the time required for the ophthalmologist/technician to learn how to take pictures suitable for clinical analysis.
Acknowledgements
The authors thank Philip Buscemi for his critical discussion and final manuscript revision.
Disclosure
The authors report no conflicts of interest in this work.
References
- VaranoMBilliBScassaCRossiTStirpeMScanning laser ophthalmoscopy in the early diagnosis of vitreoretinal interface syndromeRetina19971743003059279945
- OguraYHondaYEvaluation of idiopathic epiretinal membranes by a scanning laser ophthalmoscopeBr J Ophthalmol19937785345358025057
- WebbRHHughesGWDeloriFCConfocal scanning laser ophthalmoscopeApplied Optics19872681492149920454349
- MainsterMATimberlakeGTWebbRHHughesGWScanning laser ophthalmoscopy. Clinical applicationsOphthalmology19828978528577122056
- WolfSArendOToonenHRetinal capillary blood flow measurement with a scanning laser ophthalmolscope. Preliminary resultsOphthalmology199198699610001866155
- TammewarAMBartschDUKozakIImaging vitreomacular interface abnormalities in the coronal plane by simultaneous combined scanning laser and optical coherence tomographyBr J Ophthalmol200993336637219019945
- ChangLKFineHFSpaideRFKoizumiHGrossniklausHEUltrastructural correlation of spectral-domain optical coherence tomographic findings in vitreomacular traction syndromeAm J Ophthalmol2008146112112718439563
- SebagJGuptaPRosenRRGarciaPSadunAAMacular holes and macular pucker: the role of vitreoschisis as imaged by optical coherence tomography/scanning laser ophthalmoscopyTrans Am Ophthalmol Soc200710512112918427601
- SebagJTo see the invisible: the quest of imaging vitreousDev Ophthalmol20084252818535377