Abstract
We report five cases of unexplained retinal hemorrhage after 23-gauge sutureless vitrectomy. A 23-gauge sutureless vitrectomy was performed for four cases of macular holes (MH) and one case of macular hole retinal detachment (MHRD). Retinal hemorrhages were observed on the first day after surgery and disappeared within several months without leaving any recognizable damage. We speculate that the retinal hemorrhages might have resulted from repeated collapse of the globe through a cannula under air perfusion, but other causes such as retinal vein congestion by face-down positioning are also possible.
Introduction
In microincision vitrectomy surgery (MIVS), the entrance incision at the conjunctiva and scleral wound is so small that wound suturing is unnecessary.Citation1,Citation2 Postoperative patient discomfort and astigmatism are less after MIVS than after 20-gauge standard vitrectomy and the postoperative recovery is faster.Citation3
However, patients who undergo MIVS also have a higher risk of developing postoperative hypotony and endophthalmitis because of sutureless surgery.Citation4 Various attempts to prevent these complications have been reported.Citation5,Citation6 As a result of these surgical modifications, the incidences of such complications have decreased markedly.Citation7
The primary focus is directed toward preventing postoperative complications; however, little attention has been paid to the problematic use of cannulae.
We experienced five cases of retinal hemorrhages after 23-gauge sutureless vitrectomy that might have resulted from sharp intraocular pressure (IOP) fluctuations under air perfusion in the vitreous cavity.
Case reports
A 23-gauge vitrectomy using a cannula without a closure valve was performed to treat four cases of macular holes (MH) and one case of macular hole retinal detachment (MHRD). The internal limiting membrane (ILM) was peeled away from the inner retina over the entire macular area, using brilliant blue G (BBG) dye solution (0.25 mg/mL) (Sigma Aldrich, St Louis, MO) to stain the ILM. A fluid–air exchange was carried out with 30 mm Hg of air perfusion pressure. At the end of surgery, 20% SF6 gas for the MH or 12% C3F8 gas for the MHRD was injected into the globe. Cataract surgery was simultaneously performed in all cases.
A 67-year-old woman (Case 1) visited our clinic 4 months after she noticed blurred vision in her left eye. The visual acuity (VA) level of the left eye was 4/20 at the initial visit. A stage II MH in her left eye was diagnosed by optical coherence tomography (OCT). A 23-gauge vitrectomy was performed. The globe collapsed when a perioperative instrument was inserted and removed after fluid–air exchange with 30 mm Hg of air perfusion pressure. The IOP on the day after surgery was 16 mmHg, and the IOP values ranged between 10 and 16 mmHg during the following 5-month observation period. MH closure was confirmed by postoperative OCT. Scattered intraretinal hemorrhages were identified in the fundus 1 day after surgery (). The retinal hemorrhage completely resolved in about 2 months. Four months postoperatively, Goldmann perimetry showed no visual field constriction in that eye. In the other four cases, the collapse of the globes was similar to that in Case 1, and the hemorrhages resolved between 1 and 4 months in all cases without other complications. The IOPs were normal during the follow-up period in those four cases. Goldmann perimetry was within normal limits, similar to that in Case 1 (). In all patients, retinal hemorrhage was seen only in the operated eye, and the fellow eye was normal. Neither eye showed hemorrhage preoperatively.
Figure 1 The retinal hemorrhage is observed over three quadrants in the fundus just after disappearance of the 20% SF6 gas.
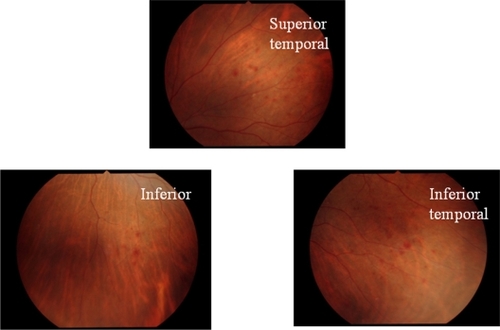
Table 1 Clinical patient data
Discussion
Regarding retinal hemorrhages related to sharp IOP fluctuations, Fechtner et al reported that a rapid drop in IOP after filtering glaucoma surgery may have caused the retinal hemorrhages, which the authors referred to as ocular decompression retinopathy.Citation8 Following that report, similar cases were reported. Rezende et al reported two cases with retinal hemorrhages simulating decompression retinopathy due to a rapid drop in postoperative IOP after 25-gauge sutureless vitrectomy.Citation9 These procedures were performed for retained lens fragments and elevated IOP after complicated phacoemulsification. Unlike their report, in the current cases, fluid–air exchange was performed and the postoperative IOP values were within the normal range during the follow-up periods. We speculated that the dramatic drop in IOP due to the repeated collapse of the globe under air perfusion in the vitreous cavity might be one of the causes of the retinal hemorrhages. We also cannot exclude the possibility that the retinal hemorrhages might have been the initial sign of expulsive hemorrhage rather than decompression retinopathy. In addition, the possibilities of other causes, such as retinal vein congestion in the gas-filled globe due to face-down positioning, still remain. However, we did not experience such cases in conventional 20-gauge vitrectomy for macular hole surgery.
The cannula system may have the advantages of a smaller incision and sutureless vitrectomy transconjunctivally, but the external and intraocular environments are directly connected through the cannula, which appears to cause a dramatic IOP drop when removing the instrument, especially under air perfusion conditions. We experienced similar conditions during conventional 20-gauge vitrectomy under air perfusion in cases where patients were inferred to have thin sclerae, such as in high myopia. However, we consider that a scleral wound in general may act as a loose-fit closure valve, in that the wound lets the fluid leak when intraocular pressure is high and stops the leak when it drops. In contrast, the placement of the cannula in the scleral wound renders it literally a “leak hole.” Greater attention to pressure fluctuations is considered necessary in this situation. The dramatic IOP drop during surgery may result in retinal circulatory disturbances. Considering these results, lower perfusion pressure should be used and the perioperative IOP fluctuations kept to a minimum, especially in a vitreous cavity filled with air. We postulate that cannulae with a valve would be useful for blocking leak flow to maintain a relatively steady IOP.
Along with expanded indications for MIVS,Citation10 maintenance of the integrity of a self-sealing wound and steady IOP values during vitreous surgery are important issues.
Disclosure
The authors report no conflicts of interest in this work.
References
- FujiiGYDe JuanEJrHumayunMSA new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgeryOphthalmology2002109101807181212359598
- EckardtCTransconjunctival sutureless 23-gauge vitrectomyRetina200525220821115689813
- OkamotoFOkamotoCSakataSChanges in corneal topography after 25-gauge transconjunctival sutureless vitrectomy versus after 20-gauge standard vitrectomyOphthalmology2007114122138214118054632
- KunimotoDYKaiserRSWills Eye Retina Service. Incidence of endophthalmitis after 20- and 25-gauge vitrectomyOphthalmology2007114122133213717916378
- TabanMSharmaSVenturaAAKaiserPKEvaluation of wound closure in oblique 23-gauge sutureless sclerotomies with Visante optical coherence tomographyAm J Ophthalmol2009147110110718835474
- ShimadaHNakashizukaHHattoriTMoriRMizutaniYYuzawaMConjunctival displacement to the corneal side for oblique-parallel insertion in 25-gauge vitrectomyEur J Ophthalmol200818584885118850574
- ShimadaHNakashizukaHHattoriTMoriRMizutaniYYuzawaMIncidence of endophthalmitis after 20- and 25-gauge vitrectomy: causes and preventionOphthalmology2008115122215222018930557
- FechtnerRDMincklerDWeinrebRNComplications of glaucoma surgery. Ocular decompression retinopathyArch Ophthalmol199211079659681637282
- RezendeFARegisLGKickingerMAicantaraSDecompression retinopathy after 25-gauge transconjunctival sutureless vitrectomy: report of 2 casesArch Opthalmol20081255699700
- ShimadaHNakashizukaHMoriRMizutaniYExpanded indications for 25-gauge transconjunctival vitrectomyJpn J Ophthalmol200549539740116187041