Abstract
Background
The purpose of this study was to evaluate the precision of intraocular pressure measurements obtained by PT100 noncontact tonometry in a handheld and slit lamp-mounted position in comparison with that of Goldmann applanation tonometry in healthy young adults.
Methods
Sixty eyes from 60 subjects (30 men and 30 women) aged 22 ± 1 (range 20–24) years participated in this study. Triplicate intraocular pressure measurement of a randomly selected eye was obtained by a noncontact tonometer in a handheld and slit lamp-mounted position in a randomized order, with the Goldmann applanation tonometer always performed last. A second measurement session was carried out after one week to assess repeatability.
Results
The mean ± standard deviation of intraocular pressure readings in the first and second session, respectively, with the three techniques were: handheld position, 14.52 ± 3.28 mmHg and 15.26 ± 2.11 mmHg; slit lamp-mounted position, 14.01 ± 2.80 mmHg and 15.16 ± 2.34 mmHg; and Goldmann applanation tonometer, 14.86 ± 3.26 mmHg and 15.16 ± 2.42 mmHg. There were no significant differences (P > 0.05) between the techniques in the intraocular pressure measurements returned (Goldmann applanation tonometer vs handheld and Goldmann applanation tonometer vs slit lamp-mounted). The Goldmann applanation tonometer measured intraocular pressure 0.34 mmHg higher than handheld and 0.85 mmHg higher than slit lamp-mounted in session 1, and in session 2 Goldmann applanation tonometer intraocular pressure measurement was the same as with the slit lamp-mounted method but lower than with the handheld method by 0.11 mmHg. In PT100 handheld vs slit lamp-mounted comparisons, there were no significant differences (P > 0.05) between intraocular pressure measurements returned by both techniques in sessions 1 and 2. Intrasession and intersession repeatability coefficients for Goldmann applanation tonometer intraocular pressure and slit lamp-mounted intraocular pressure were similar, and better in comparison with those for handheld intraocular pressure.
Conclusion
The Goldmann applanation tonometer and PT100 noncontact tonometer in both positions studied here are reliable, consistent techniques for measurement of intraocular pressure, and can be used interchangeably for obtaining intraocular pressure values in young normal subjects. Repositioning of the PT100 tonometer from hand-held to slit lamp-mounted improved its precision and reduced variation with respect to the Goldmann applanation tonometer.
Introduction
Intraocular pressure is currently the only treatable risk factor for developing primary open-angle glaucoma, and when neglected, predisposes the eye to subsequent deterioration in vision and visual field damage.Citation1 It is one of a ternary of clinical signs monitored for the diagnosis and/or management of glaucoma, especially primary open-angle glaucoma, in which the pathogenesis of the disease is insidious.Citation2 Intraocular pressure measurement is essential in glaucoma diagnosis and also in assessment of the efficiency of glaucoma treatment with various antiglaucoma agents.Citation3
The Goldmann applanation tonometer is the gold standard in clinical practice for measurement of intraocular pressure, against which all other types of tonometers are compared. Although manometry is the most accurate method, its invasive nature has limited its applications in clinical settings.Citation4 While the Goldmann applanation tonometer is preferred in adults, it is often inconvenient or impossible to use in children, which is why devices such as PT100 were developed.Citation5,Citation6 Goldmann tonometry requires the instillation of fluorescein, ocular topical anesthesia, and corneal contact to obtain precise intraocular pressure measurements. To do this, the probe must be in contact with the central cornea so as to applanate a fixed corneal area, thereby increasing the risk of spreading infectious diseases of the cornea and conjunctiva, and of possible damage to the corneal epithelium.Citation7 The Goldmann applanation tonometer only gives an estimate of the true intraocular pressure as measured by manometry. However, the accuracy of noncontact tonometers is limited by the accuracy of the Goldmann applanation tonometer, because they are all calibrated against it.Citation8 Description of the clinical use of noncontact tonometers introduced in 1974 by Forbes et alCitation9 has since undergone various transitions and has led to technological improvements in the design and manufacture of more accurate, reliable, and easy to use noncontact tonometers.
Several studies have compared intraocular pressure measurements made with noncontact tonometers and Goldmann tonometers.Citation2,Citation10–Citation13 In one study,Citation13 the accuracy of two noncontact tonometers, including the Reichert AT550, Goldmann applanation tonometer, and a Perkins tonometer was tested in a young normal population. The results showed a high level of agreement between the AT550 and Goldmann applanation tonometer. Therefore, the investigators concluded that intraocular pressure readings obtained by AT550 are comparable clinically with those obtained by the Goldmann applanation tonometer in a population having intraocular pressure within the normal range.Citation13 However, very few studies have compared readings obtained by the PT100 and Goldmann applanation tonometer. So far, three studies have reported a good correlation between the PT100 and Goldmann applanation tonometer.Citation11,Citation14,Citation15 Murase et alCitation14 analyzed their data based on the effect of central corneal thickness on intraocular pressure measurements obtained by the PT100 and the Goldmann applanation tonometer, whilst the comparative study of the PT100 and the Goldmann applanation tonometer done by Salim et alCitation11 had a large variation in age among the recruited subjects, which may have affected the accuracy of their results. However, neither the Salim et alCitation11 nor Murase et al studyCitation14 was able to demonstrate the repeatability of intraocular pressure measurements in normotensive subjects obtained by the PT100 NCT when compared with the Goldmann applanation tonometer. The only study to demonstrate the repeatability of Goldmann applanation tonometry in comparison with the PT100 observed that the intrasession repeatability of both techniques for test-retest differences was within ±5 mmHg.Citation15 It is important to note that the intraocular pressure measurements in the three studies cited above were obtained by the PT100 noncontact tonometer in a handheld position.
The portable noncontact tonometer, Reichert PT100 (Buffalo, Depew, NY) is increasingly used in optometry practices due to its rapidity and convenience in obtaining intraocular pressure measurements. It is also the first truly handheld noncontact tonometer (this increases its versatility), making it a useful screening instrument in preference to the Goldmann applanation tonometer. The readings obtained by noncontact tonometers are largely independent of the operator.Citation16 While one studyCitation15 noted no statistically significant difference in mean intraocular pressures measured by Goldmann applanation tonometer and the PT100, another studyCitation11 observed a significant difference in intraocular pressure measurements returned by the Goldmann applanation tonometer and the PT100 when handheld. They further suggested that instability of the PT100 instrument was a possible reason for the variation in intraocular pressure readings between the Goldmann applanation tonometer and the PT100. Hence, this study was conducted to assess any possible differences in the precision of intraocular pressure measurements obtained when the PT100 noncontact tonometer was used in different positions (handheld and slit lamp-mounted) in comparison with the Goldmann applanation tonometer intraocular pressure measurements.
Methods
Data
Data for this study were obtained from 69 subjects recruited from students of various colleges at King Saud University. The study adhered to the tenets of the Declaration of Helsinki, and the protocol was approved by the ethics committee of the College of Applied Medical Sciences, King Saud University. Each subject gave their informed consent, after having the risks and benefits of participation explained to them. For inclusion in this study, subjects were required to be oculovisually healthy during the study period, and should not have participated in any of our similar studies. Patients with any corneal disease, previous history of corneal surgery, glaucoma or a family history of glaucoma, recent use of steroids, or a high refractive error were excluded. Nine subjects were excluded because of recent completion of systemic steroid therapy (n = 3), and family history of glaucoma (n = 6). Overall, only intraocular pressure readings obtained from 60 eyes of 60 subjects (30 men and 30 women) were included in the statistical analysis. The sample size was calculated on average values of intraocular pressure obtained with a Goldmann applanation tonometer to warrant a power of 80% with a statistical significance level of 0.05.
Measurement procedure
All measurements of intraocular pressure were taken between 2 pm and 4 pm to minimize the effect of diurnal variations on intraocular pressure measurements.Citation17–Citation19 All measurements were obtained in a sitting position, and for the PT100 slit lamp-mounted and Goldmann applanation tonometer, measurements were taken only after proper alignment of the patient on a slit lamp.
A total of nine intraocular pressure measurements were obtained for each patient in each measurement session. The average of triplicate intraocular pressure measurements for each subject formed the data points used for our statistical analysis. For assessment of repeatability of the different techniques, subjects were required to return for a second measurement session separated by one week.
In session 1, the eye assessed and the order of all intraocular pressure measurements obtained by PT100 were randomized. Goldmann applanation tonometer measurements were performed after use of the noncontact tonometer to eliminate the reported possible effect of ocular massage by the Goldmann applanation tonometer.Citation20 In the second measurement session, except for randomization, the order of use of the instruments and the eye assessed was the same as in session 1. Randomization was by a set of random numbers generated from Microsoft Excel (2003; Microsoft, Redmond, WA).
For measurements of intraocular pressure by PT100, all outlying readings (that varied by 4 mmHg compared with other measurements) and those having a low confidence interval (marked with an asterisk or put in brackets) were repeated.Citation11 For Goldmann applanation tonometer measurements, one drop of 0.4% oxybuprocaine hydrochloride was used for each tonometry measurement session. Saline wetted fluorescein was then applied to the superior bulbar conjunctiva before each session measurement was obtained. The tonometer drum was reset to 10 mmHg and recorded by a second clinician (JC) after each reading was obtained. To reduce observer bias, one experienced examiner made all tonometry measurements.
Statistical analysis
All statistical analysis was performed using GraphPad Instat for Windows program (v 3.10; GraphPad Software Inc, San Diego, CA, www.graphpad.com). Normal distribution of variables was assessed using the Kolmogorov–Smirnov test. The mean ± standard deviation [SD] of the average intraocular pressure readings is stated in the results along with the minimum and maximum intraocular pressure values in each session and with each technique. Descriptive statistics were used to summarize the data for the sets of measurement using the three techniques. A repeated-measures analysis of variance was performed once to evaluate the differences between instruments and between sessions. The columns analyzed were: Goldmann applanation tonometer vs PT100 handheld vs PT100 slit lamp-mounted (session 1); Goldmann applanation tonometer vs PT100 handheld vs PT100 slit lamp-mounted (session 2). The 95% limits of agreement (mean of the difference ±1.96 SD of differences) were also depicted in a combined session Bland and AltmanCitation19 plot of mean difference (between techniques) against the averages for each pair of techniques (ie, Goldmann applanation tonometer vs handheld, Goldmann applanation tonometer vs slit lamp-mounted, and handheld vs slit lamp-mounted).
Assessment of repeatability of the three techniques
A measurement technique is considered repeatable if repeated measurements obtained in the same individual produce the same results.Citation17 This is usually done to ensure that factors contributing to the variability of results remain constant and exert little or no influence on the final result.
Intrasession and intersession repeatability coefficients were calculated using the Bland–AltmanCitation21 formula of 1.96 × SDmean differences for both positions of the PT100 and for the Goldmann applanation tonometer. In each session and for each technique, the intrasession repeatability coefficient was calculated using the mean differences of the triplicate intraocular pressure measurements obtained for each subject. The mean intersession difference was plotted against the averages of sessions 1 and 2 of same technique using the Bland–Altman formula, and 95% confidence limits were depicted. To assess the magnitude of intrasession and intersession differences, repeated-measures analysis of variance was conducted on the columns of averages in each session. The columns considered in this analysis were: Goldmann applanation tonometer session 1 vs session 2; PT100 handheld session 1 vs session 2; and PT100 slit lampmounted session 1 vs session 2.
Results
Sixty eyes from 60 subjects divided equally among men (n = 30, 50%) and women (n = 30, 50%) aged 22 ± 1 (range 20–24) years were used for statistical analysis in this study.
Mean intraocular pressure readings
shows the average (±SD) and range of readings for intraocular pressure obtained with each of the techniques used in this study at each measurement session. On average, the Goldmann applanation tonometer showed the highest mean values for intraocular pressure, followed very closely by the handheld PT100, with the slit lamp-mounted PT100 showing the lowest mean values.
Table 1 Average, standard deviation, and range (minimum and maximum) of intraocular pressure measurements (mmHg) obtained by Goldmann applanation tonometer, PT100 handheld, and PT100 slit lamp-mounted
Agreement between intraocular pressure measurements using the three techniques
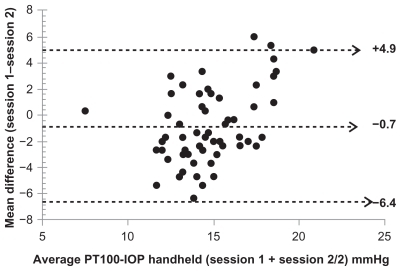
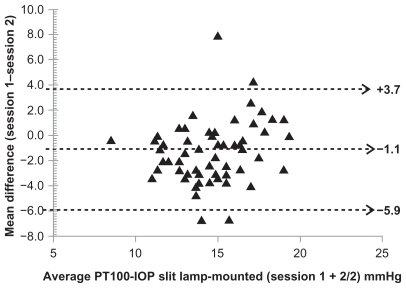
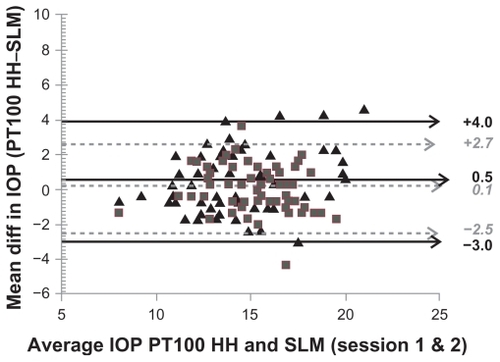
In sessions 1 and 2, no significant differences in intraocular pressure measurements were found between the Goldmann applanation tonometer and handheld PT100 (P > 0.05), Goldmann applanation tonometer and slit lamp-mounted (P > 0.05), and between handheld and slit lamp-mounted PT100 (P > 0.05). – illustrate the agreement between techniques represented as a combined session Bland–Altman plot of the mean difference against the averages of two techniques (Goldmann applanation tonometer vs handheld, ; Goldmann applanation tonometer vs slit lamp-mounted, ; slit lamp-mounted vs handheld, ) with 95% limits of agreement shown. Using linear regression, intraocular pressure with the Goldmann applanation tonometer was correlated significantly with the slit lamp-mounted intraocular pressure (Pearson’s r = 0.5498, 0.5510; P > 0.0001) and handheld intraocular pressure (Pearson’s r = 0.5748, 0.5618 ; P > 0.0001) measurements in sessions 1 and 2, respectively.
Figure 1 A Bland–Altman plot of the mean difference in intraocular pressure measurements between the Goldmann applanation tonometer and PT100 noncontact tonometer in a handheld position as a function of their averages in both sessions. Solid straight lines are for session 1 and dotted lines for session 2.
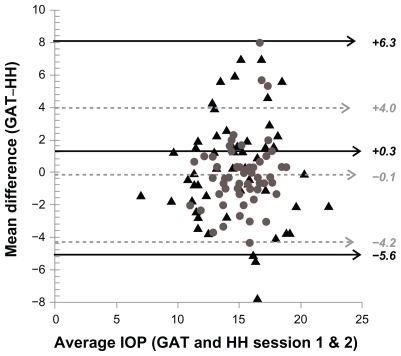
Figure 2 A Bland–Altman plot of the mean difference in intraocular pressure measurements between the Goldmann applanation tonometer and the PT100 noncontact tonometer in a slit lamp-mounted position as a function of their averages in both sessions. Solid straight lines are for session 1 and dotted lines for session 2.
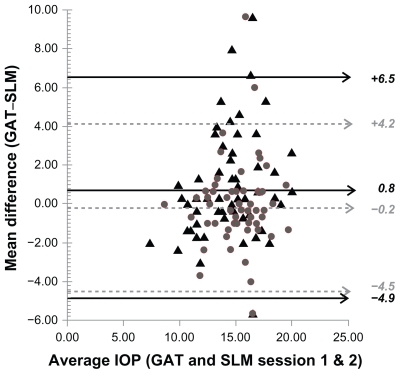
Figure 3 A Bland–Altman plot of the mean difference in intraocular pressure measurements between the PT100 noncontact tonometer in a slit lamp-mounted position and in a handheld position as a function of their averages in both sessions. Solid straight lines are for session 1 and dotted lines for session 2.
Intrasession and intersession repeatability of intraocular pressure measurements
For the Goldmann applanation tonometer and handheld techniques, repeated-measures analysis of variance showed that mean intrasession and intersession differences in intraocular pressure did not vary in session 1 (P > 0.05) or in session 2 (P > 0.05). For the slit lamp-mounted technique, a small but statistically significant (P > 0.05) mean intrasession difference in intraocular pressure of about 1.15 mmHg was observed on analysis.
The intrasession repeatability coefficients for the Goldmann applanation tonometer (±2.03/±2.28 mmHg sessions 1 and 2), PT100 handheld (±2.64/±2.49 mmHg, sessions 1 and 2), and PT100 slit lamp-mounted (±2.08/±1.77 mmHg, sessions 1 and 2) were comparable in both sessions, but superior for PT100 slit lamp-mounted. The intrasession difference in intraocular pressure for the three techniques was within ±0.5 mmHg.
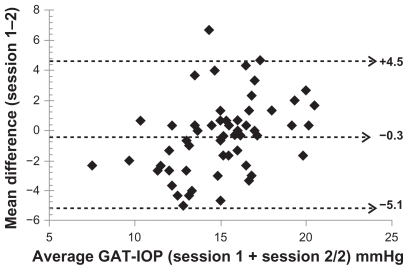
The intersession repeatability coefficient was similar for the Goldmann applanation tonometer (±4.75 mmHg) and slit lamp-mounted (±4.80 mmHg), which was better in comparison with handheld (±5.68 mmHg).
Intersession repeatabilities are represented as a Bland– Altman plot of mean difference against averages of the Goldmann applanation tonometer (), handheld (), and slit lamp-mounted () with the 95% limits of repeatability depicted. The intersession difference in intraocular pressure for each technique was within ±1 mmHg for all techniques.
Figure 4 A Bland–Altman plot of the mean intersession difference of the Goldmann applanation tonometer intraocular pressure as a function of the averages in sessions 1 and 2.
Discussion
In this study we assessed the precision of intraocular pressure measurement using the PT100 noncontact tonometer in two different positions, ie, handheld and slit lamp-mounted, as compared with Goldmann applanation tonometer values. A previous studyCitation11 had suggested that improper fixation might be a major limitation to intraocular pressure measurements obtained with the PT100.
The intrasession intraocular pressure variations for the Goldmann applanation tonometer, handheld and slit lampmounted, did not differ significantly in sessions 1 and 2 for the same technique, and furthermore, the mean intersession intraocular pressure differences for the three techniques did not vary. Although the slit lamp-mounted intraocular pressure measurements varied significantly between sessions by 1.15 mmHg, the difference was not clinically important because intraocular pressure obtained by noncontact tonometer can vary between consecutive measurements by as much as 7 mmHg. This suggests that the three techniques used in this study have a similar consistency in measurements of intraocular pressure within a session.
In agreement with the suggestion of Salim et al,Citation11 the stability introduced to the PT100 intraocular pressure measurements (by mounting it on a slit lamp) improved its precision because the intrasession (±2.08 mmHg, ±1.77 mmHg, session 1 and 2) and intersession repeatability coefficients (±4.80 mmHg) were superior to those of the handheld PT100 (intrasession ±2.64 mmHg, ±2.49 mmHg, session 1 and 2; intersession ±5.68 mmHg) and slightly better than that of Goldmann applanation tonometer (intrasession ±2.03 mmHg, ±2.28 mmHg, session 1 and 2; intersession ±4.75 mmHg). However, all three techniques produced reliable intraocular pressure measurements within and between sessions. These findings were comparable with the repeatability coefficients (1.8 mmHg and 2.1 mmHg, Goldmann applanation tonometer sessions 1 and 2; 1.9 and 1.8 mmHg PT100 handheld sessions 1 and 2) reported in another study;Citation15 this study also reported the repeatability coefficient for test-retest differences of both techniques to be within ±5 mmHg, which is similar to that found in the current study (±6 mmHg).
The difference in intraocular pressure measurements between techniques did not differ significantly (P > 0.05) in both sessions, thus PT100 in both positions and Goldmann applanation tonometer can be used interchangeably for the measurement of intraocular pressure in normal subjects. This reaffirms the findings of Almubrad.Citation15 Overall, Goldmann applanation tonometer and PT100 handheld intraocular pressure measurements were consistently higher than PT100 slit lampmounted intraocular pressure values, whereas a comparison of Goldmann applanation tonometer and handheld intraocular pressure values resulted in Goldmann applanation tonometer measurements being insignificantly higher in session 2 while handheld was insignificantly higher in session 1.
The mean intraocular pressure in the present observation (14.89 mmHg, 14.58 mmHg, 15.01 mmHg, for handheld, slit lamp-mounted, and Goldmann applanation tonometer, respectively) is comparable with that reported in two previous studies (15.98 mmHg, 15.65 mmHg, PT100 and Goldmann applanation tonometer, respectively),Citation11 and 15 mmHg for both PT100 and Goldmann applanation tonometer.Citation15 However, in one of the studies,Citation11 the variability in intraocular pressure measurements using both techniques (±5.98 mmHg and ±4.26 mmHg for the PT100 and Goldmann applanation tonometer, respectively) was larger than that obtained in the present study (±2.35 mmHg, ±2.27 mmHg, and ±2.61 mmHg, for handheld, slit lamp-mounted, and Goldmann applanation tonometer, respectively). This is probably a reflection of the older subjects enrolled in the study by Salim et al.
It was the aim of this study to compare the PT100 noncontact tonometer with the Goldmann applanation tonometer which is the clinical gold standard for intraocular pressure measurements. Many intraocular pressure studies have shown good clinical agreement between the noncontact tonometer and Goldmann applanation tonometer, with lower consistency in noncontact tonometry when the pressure is in the higher range.Citation2,Citation5,Citation7,Citation13,Citation22 In our study, within the normal range of intraocular pressure levels, PT100 in both positions demonstrated a close level of agreement when compared with the Goldmann applanation tonometer, as depicted by the Bland–Altman plots of agreement.
To the best of our knowledge, this is the first study to demonstrate the variation in intraocular pressure measurements obtained when PT100 is used in the handheld and slit lamp-mounted position. The study is limited by the lack of patients with increased intraocular pressure, and the narrow age group of subjects recruited, because the noncontact tonometer has been shown to be less accurate with higher pressures.Citation2,Citation5,Citation7,Citation13,Citation22 There is also a possibility that central corneal thickness and curvature of the cornea may have influenced the intraocular pressure results obtained in this study. Studies have continuously shown that, while corneal curvature radius,Citation23 the elastic properties of the cornea, ie, rigidity and stiffness,Citation14,Citation23–Citation26 can influence intraocular pressure accuracy obtained by the Goldmann applanation tonometer and the noncontact tonometer, the noncontact tonometer is more affected by central corneal thickness than the Goldmann applanation tonometer.Citation12,Citation14,Citation26 Therefore, the data in the current study are limited by the lack of central corneal thickness and cornea curvature measurements for adequate comparison. Studies comparing the two position measurements of intraocular pressure obtained by the PT100 with the Goldmann applanation tonometer in subjects with higher intraocular pressure ranges should consider recruiting subjects of various age groups, and determining central corneal thickness measurements in those subjects. This is to verify if similar findings occur for higher intraocular pressure ranges, and determine the effects of the cornea biomechanical properties on intraocular pressure obtained with the PT100.
Nevertheless, this study suggests that the lack of head and chin rests may have an influence on the precision of PT100 intraocular pressure measurements obtained in a handheld position with respect to the Goldmann applanation tonometer, but does not result in any significant variation in intraocular pressure measurements obtained on repositioning the instrument.
Generally, a repositioning of the PT100 from the conventional hand-held position to a slit lamp-mounted position not only improved its precision but also reduced the variation in intraocular pressure measurements reportedCitation11,Citation14 when the Goldmann applanation tonometer was compared with the PT100. There was no difference in the variation between the two positions of the PT100 with respect to the Goldmann applanation tonometer in session 1 (11.39 mmHg/11.82 mmHg, slit lamp-mounted/handheld) and in session 2 (8.56 mmHg/8.25 mmHg, slit lamp-mounted/ handheld). Therefore, in a clinic setting, and for research purposes, incorporation of a head-rest or stabilizing the PT100 on a slit lamp will enhance the precision of the instrument. However, outside a clinic setting where intraocular pressure measurements might be obtained by medical personnel or nonmedical personnel, handheld positioning of the PT100 is still the preferred technique because its portability is beneficial.
The PT100, like other portable tonometers, makes noncontact glaucoma screening a possibility, given that the use of tonometry in glaucoma screening has been an ongoing debate, and appearing to be of limited diagnostic value as a solitary test.Citation29 However, it is commonly performed in glaucoma screenings in and out of clinic in conjunction with other diagnostic modalities.Citation30,Citation31 Screenings may be done by nonmedical and unlicensed personnel. Because noncontact tonometry does not require topical anesthetic or staining drops and the readings are infrequently affected by the operator, it allows screenings to be implemented without the direct supervision of medical doctors, allowing screening staff relative independence in operation.Citation22
In conclusion, the three techniques are consistent in their measurement of intraocular pressure in the same session and between sessions. The difference in intraocular pressure measurements between techniques did not differ significantly (P > 0.05) in both sessions, and therefore the three techniques can be used interchangeably for measurement of intraocular pressure in normal young adults.
Disclosure
The authors report no conflicts of interest in this work.
References
- VanVeldhuisenPCEdererFDouglasGAThe Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deteriorationAm J Ophthalmol200013042944011024415
- OgbuehiKCAssessment of the accuracy and reliability of the Topcon CT80 non-contact tonometerClin Exp Optom20068931031416907669
- FernandezPDiaz-ReyJAQueirosAGonzalez-MeijomeJMJorgeJComparison of the ICare rebound tonometer with the Goldmann tonometer in a normal populationOphthalmic Physiol Opt20052543644016101950
- CuckburnDMTonometryEskridgeJBAmosJBarlettJDClinical Procedures In Optometry1st edPhiladelphia, PALippincott Willams and Wilkins1991
- LamAKChanRChiuRLamCThe validity of a new noncontact tonometer and its comparison with the Goldmann tonometerOptom Vis Sci20048160160515300119
- GoldmannHSchmidtTApplanation tonometryOphthalmologica1957134221242 German13484216
- RegineFScuderiGLCesareoMRicciFCedroneCNucciCValidity and limitations of the Nidek-4000 non-contact tonometer: A clinical studyOphthalmic Physiol Opt200626333916390480
- Al MubradTMOgbuehiKCThe effects of repeated applanation on subsequent IOP measurementsClin Exp Optom20089152452918651843
- ForbesMPicoGJrGrolmanBA noncontact applanation tonometer. Description and clinical evaluationArch Ophthalmol1974911341404810646
- Garcia-ResuaCFernandezGMJYebra-PimentelEGarcia-MonteroSClinical evaluation of the Canon TX-10 noncontact tonometer in healthy eyesEur J Ophthalmol20102052353020037897
- SalimSLinnDJEcholsIIJRNetlandPAComparison of intraocular pressure measurements with the portable PT100 noncontact tonometer and Goldmann applanation tonometryClin Ophthalmol2009334134419668588
- TonnuPAHoTSharmaKWhiteEBunceCGarway-HeathDA comparison of four methods of tonometry: Method agreement and interobserver variabilityBr J Ophthalmol20058984785015965164
- JorgeJGonzalez-MeijomeJMDiaz-ReyJAAlmeidaPRParafitaMAClinical Performance of non-contact tonometry by Reichert AT550 in glaucomatous patientsOphthalmic Physiol Opt20032350350614622352
- MuraseHSawadaAMochizukiKEffects of corneal thickness on intraocular pressure measured with three different tonometersJpn J Ophthalmol2009531619184301
- AlmubradTMPerformance of the PT100 noncontact tonometer in healthy eyesClin Ophthalmol2011566166621629572
- McCaghreyGEMatthewsFEThe Pulsair 3000 tonometer – how many readings need to be taken to ensure accuracy of the average?Ophthalmic Physiol Opt20012133433811430628
- NoelCKaboAMRomanetJPMontmayeurABuguetATwentyfour- hour time course of intraocular pressure in healthy and glaucomatous Africans: Relation to sleep patternsOphthalmology200110813914411150279
- LiuJHKripkeDFTwaMDTwenty-four-hour pattern of intraocular pressure in the ageing populationInvest Ophthalmol Vis Sci1999402912291710549652
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet198613073102868172
- KrakauCEWilkeKOn repeated tonometryActa Ophthalmol (Copenh)1971496116145171572
- BlandJMAltmanDGApplying the right statistics: Analysis of measurement studiesUltrasound Obstet Gynecol200322859312858311
- Moreno-MontanesJGomez-DemmelELajara-BlesaJAliseda- PerezDComparative study of three non-contact tonometers and the Goldmann tonometerOphthalmologica19942081151188065693
- WhitacreMMSteinRSources of error with use of Goldmann-type tonometersSurv Ophthalmol1993381308235993
- MedeirosFAWeinrebRNHassaneinKThe effects of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzerJ Glaucoma20061536437016988597
- HaradaYHiroseNKubotaTTawaraAThe influence of central corneal thickness and corneal curvature radius on the intraocular pressure as measured by different tonometers: Noncontact and Goldmann applanation tonometersJ Glaucoma20081761962519092456
- TonnuP-AHoTNewsonTThe influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and Goldmann applanation tonometryBr J Ophthalmol20058985185415965165
- KoY-CLiuC-JHsuW-MVarying effects of corneal thickness on intraocular pressure measurements with different tonometersEye20051932733215258603
- SponselWETonometry in question: Can visual screening tests play a more decisive role in glaucoma diagnosis and management?Surv Ophthalmol1989332913002655142
- MundorfTKZimmermanTJNardinGFKendallKSAutomated perimetry, tonometry, and questionnaire in glaucoma screeningAm J Ophthalmol19891085055082683793
- TuckMWCrickRPThe cost-effectiveness of various modes of screening for primary open angle glaucomaOphthalmic Epidemiol199743179145411