Abstract
Background
The purpose of this study was to compare differences in visual outcomes, higher-order aberrations, contrast sensitivity, and dry eye in patients undergoing photorefractive keratectomy using wavefront-guided VISX CustomVue™ and wavefront-optimized WaveLight® Allegretto platforms.
Methods
In this randomized, prospective, single-masked, fellow-eye study, photorefractive keratectomy was performed on 46 eyes from 23 patients, with one eye randomized to WaveLight Allegretto, and the fellow eye receiving VISX CustomVue. Three-month postoperative outcome measures included uncorrected distance visual acuity, corrected distance visual acuity, refractive error, root mean square of total and grouped higher-order aberrations, contrast sensitivity, and Schirmer’s testing.
Results
Mean values for uncorrected distance visual acuity (logMAR) were −0.03 ± 0.07 and −0.06 ± 0.09 in the wavefront-optimized and wavefront-guided groups, respectively (P = 0.121). Uncorrected distance visual acuity of 20/20 or better was achieved in 91% of eyes receiving wavefront-guided photorefractive keratectomy, and 87% of eyes receiving wavefront-optimized photorefractive keratectomy, whereas uncorrected distance visual acuity of 20/15 was achieved in 35% of the wavefront-optimized group and 64% of the wavefront-guided group (P ≥ 0.296). While root mean square of total higher-order aberration, coma, and trefoil tended to increase in the wavefront-optimized group (P = 0.091, P = 0.115, P = 0.459, respectively), only spherical aberration increased significantly (P = 0.014). Similar increases were found in wavefront- guided root mean square of total higher-order aberration (P = 0.113), coma (P = 0.403), trefoil (P = 0.603), and spherical aberration (P = 0.014). There was no significant difference in spherical aberration change when comparing the two platforms. The wavefront-guided group showed an increase in contrast sensitivity at 12 cycles per degree (P = 0.013).
Conclusion
Both VISX CustomVue and WaveLight Allegretto platforms performed equally in terms of visual acuity, safety, and predictability in photorefractive keratectomy. The wavefront-guided group showed slightly improved contrast sensitivity. Both lasers induced a comparable degree of statistically significant spherical aberration, and tended to increase other higher-order aberration measures as well.
Introduction
Reoperation rates for primary conventional myopic photorefractive keratectomy surgery are reported to be between 16% and 20%.Citation1–Citation3 Conventional photorefractive keratectomy is capable of correcting lower-order aberrations, such as hyperopia, myopia, and astigmatism. However, the higher-order aberrations, such as coma, spherical aberration, and trefoil, are induced by (and remain uncorrected in) traditional photorefractive keratectomy.Citation4–Citation6
For patients undergoing traditional photorefractive keratectomy, image quality may suffer as a result of induced higher-order aberrations.Citation4,Citation7–Citation11 Advanced optical measurements and more sophisticated laser algorithms are found in wavefront-based treatments, which have been shown to diminish induced higher-order aberrations and increase predictability of visual outcomes compared with traditional keratorefractive surgery.Citation12–Citation16 With the development of multiple wavefront-based platforms, it is important to ascertain if there are significant differences in visual outcomes and higher-order aberrations between specific wavefront-guided and wavefront-optimized lasers used in photorefractive keratectomy. Wavefront-guided laser ablations utilize preoperative wavefront aberrometer data to treat higher-order and lower-order aberrations. These data are strictly relied upon for the final treatment pattern. In contrast, wavefront-optimized laser ablations utilize preoperative refraction data for the treatment pattern. Wavefront-optimized platforms deliver more laser pulses to the periphery, which maintains the prolate structure of the cornea, and thereby minimizes higher-order aberrations.
Based on our most recent literature search using the PubMed keywords “wavefront”, “wavefront-guided”, “wavefront-optimized”, “photorefractive keratectomy”, “photorefractive keratectomy”, and “higher-order aberration”, there are no known published studies comparing wavefront-guided lasers with wavefront-optimized lasers in patients undergoing photorefractive keratectomy. However, laser in situ keratomileusis (LASIK) studies have compared these two lasers, with some studies suggesting an advantage to wavefront-guided platforms,Citation17–Citation20 and others showing no significant difference between the two.Citation21,Citation22 In this prospective, randomized, fellow-eye study, we compared the wavefront-guided VISX CustomVue platform (Abbott Medical Optics, Santa Ana, CA) with the wavefront-optimized WaveLight Allegretto platform (Alcon Inc, Hüenberg, Switzerland) in the same patient undergoing photorefractive keratectomy, with respect to visual acuity, refractive error, higher-order aberrations, contrast sensitivity, and dry eye.
Methods and materials
This prospective, single-masked, randomized, fellow-eye study evaluated and compared the outcomes of photorefractive keratectomy performed in 23 patients (46 eyes) using the VISX CustomVue laser system and the WaveLight Allegretto laser system. Patients were recruited and enrolled at the John A Moran Eye Center, Department of Ophthalmology and Visual Science, University of Utah, between November 2010 and July 2011. All patients were older than 21 years.
The University of Utah Hospital institutional review board approved the research protocol in accordance with the tenets of the Declaration of Helsinki. All patients provided informed consent after they received an explanation of the procedure, including all risks and benefits. All patients had a preoperative discussion of relevant medical history, including history of herpetic eye disease and family history of keratoconus.
Patients were excluded if they had a history of clinically significant lens opacity, previous corneal or intraocular surgery, thin corneas, keratoconus, unstable refraction, amblyopia, or autoimmune disease, and also if they were pregnant or breastfeeding, or on immunosuppressive therapy. Patients desiring monovision were not included in the study.
Eligible patients were scheduled for bilateral photorefractive keratectomy and correction for distance in both eyes. The patients were randomly assigned (Research Randomizer software, Urbaniak, http:\\www.randomizer.org) to treatment in one eye with the WaveLight Allegretto system (wavefront-optimized group), which utilizes the WaveLight® Allegretto 400 Hz Wave® Eye-Q Laser. The fellow eye was assigned treatment with the VISX CustomVue™ STAR S4 IR™ Excimer Laser with ActiveTrack™ iris registration (wavefront-guided group).
Soft contact lenses were discontinued 2 weeks before screening and rigid gas-permeable contact lenses were discontinued 6 weeks before screening. All patients had a preoperative examination including manifest refraction and cycloplegic refraction, uncorrected distance visual acuity, corrected distance visual acuity, tonometry, slit lamp examination, and dilated fundus evaluation. Corneal topography and thickness were measured using the Pentacam (Oculus Optikgeräte GmbH, Wetzlar, Germany) and Humphrey Atlas (Carl Zeiss Meditec Inc, Jena, Germany) systems. Pupil size was measured in the dark using the Colvard pupillometer (Oasis Medical Inc, Glendora, CA). Contrast sensitivity was performed using the VectorVision CSV-1000 (Dayton, OH) chart in controlled mesopic conditions (70 lux) at 3, 6, 12, and 18 cycles per degree (cpd). Schirmer’s testing evaluation for dry eye was measured in millimeters with topical anesthetic after 5 minutes. Manifest refraction and wavefront measurements were repeated on two separate visits to ensure refractive stability.
All eyes received five preoperative wavefront analyses using the VISX CustomVue WaveScan aberrometer v3.62 (Fourier) without pharmacologic intervention, under mesopic conditions, with a minimum pupil diameter of 6.0 mm. The emmetropic correction target was based on manifest refraction, topography, and wavefront analysis for the wavefront-guided group. For the wavefront-optimized group, the emmetropic correction target was based on topography and manifest refraction. Iris registration was obtained for eyes receiving wavefront-guided treatment. A physician-adjustment factor was used based on previously established Moran Laser Center wavefront-guided photorefractive keratectomy nomograms for the laser system used for surgery. The nomograms were generated using Datagraph-med Outcomes Analysis Software for Refractive Surgery (version 3.20a; Ingenieurbüro Pieger GmbH, Wendelstein, Germany).
Prior to laser treatment, ethanol diluted to 20% in sterile water was placed on the cornea in an 8.5 mm Camellin-style laser epithelial keratomileusis (LASEK) alcohol fixation well (Katena Products Inc, Denville, NJ) for 35 seconds. Epithelial removal was performed with a Sloane LASEK epithelial micro hoe (Katena Products Inc). For stromal ablations greater than 65 mm (n Z 17), a circular sponge soaked in mitomycin C 0.02% was applied for 20 seconds. The eye was then immediately flushed with 15 mL of a chilled balanced salt solution, after which a bandage contact lens (Softlens Plano T, Bausch and Lomb, Rochester, NY) was placed. All surgeries were performed by MM and MDM.
Postoperatively, one drop of gatifloxacin 0.3% (Allergan Inc, Irvine, CA), prednisolone acetate 1.0% (Allergan Inc), and ketorolac tromethamine 0.4% (Allergan Inc) was instilled. Ketorolac tromethamine 0.4% was administered four times a day for the first 72 hours and then discontinued. Gatifloxacin 0.3% and prednisolone acetate were continued four times a day for 1 week with a subsequent steroid taper over 2–3 months. Bandage contact lenses were removed upon complete epithelial healing, typically 3–5 days after surgery.
Data were collected at 1 day, 1 week, and 1 and 3 months after surgery. Uncorrected and corrected distance visual acuity were both recorded in Snellen notation and logarithm of the minimum angle of resolution (logMAR) format. Contrast sensitivity and Schirmer’s testing were performed. Higher-order aberrations, including root mean square of total higher-order aberration, coma Z(3,1), trefoil Z(3,3), and spherical aberration Z(4,0) were measured using the WaveScan aberrometer. Undilated scans of both eyes were taken at 3 months postoperatively regardless of the wavefront platform used for treatment. The Quality of Life Impact of Refractive Correction (QIRC) survey instrument was used to record subjective outcomes, as previously described.Citation23
Statistical analysis
After the study was completed, the results were compiled and the data were unmasked for statistical analysis. Manifest refraction, refractive error, visual acuity, contrast sensitivity, higher-order aberration values for coma, trefoil, and sphere, and root mean square of higher-order aberration wavefront values were treated as continuous variables and analyzed for statistical significance using the Student’s t-test. A P value of 0.05 was considered statistically significant. Data analysis was performed using Microsoft Excel (Microsoft Corp, Redmond, WA).
Results
Twenty-three patients (46 eyes) with 3 months of follow-up were evaluated in this study. The study population consisted of 18 men and five women of mean age 31.4 ± 5.8 years, with no significant differences in preoperative corrected distance visual acuity and refraction ().
Table 1 Preoperative group comparisons
Visual acuity
Uncorrected and corrected distance visual acuity was not statistically different between the groups at 1 or 3 months (). At 3 months postoperatively, 20/15 uncorrected distance visual acuity was achieved in 35% of wavefront-optimized eyes and 64% of wavefront-guided eyes, and 20/20 uncorrected distance visual acuity was achieved by 87% and 91% of the eyes in both groups, respectively ().
Table 2 One month and 3-month visual acuity comparisons
Table 3 Efficacy, predictability, and safety comparison of Allegretto and VISX laser platforms
Safety, efficacy, and predictability
At 3 months, 16 of 23 eyes (70%) in both groups maintained equal corrected distance visual acuity. Five eyes (22%) in the wavefront-optimized group and six eyes (26%) in the wavefront-guided group gained one line of corrected distance visual acuity. One eye in the wavefront-optimized group gained two lines. In each group, one eye lost one line of corrected distance visual acuity. In the wavefront-optimized group, the loss of vision was from residual astigmatism due to a central island. In the wavefront-guided group, the loss was due to irregular corneal epithelium secondary to superficial punctate keratopathy. No other eyes in the study population lost any lines of corrected distance visual acuity (P = 1.000, ).
At 1 month, 20 eyes (87%) in the wavefront-optimized and 21 eyes (91%) in the wavefront-guided group were within ± 0.50 diopters (D) of emmetropia. In addition, 16 eyes (70%) and 17 eyes (74%), respectively, were within ± 0.25 D of emmetropia (P = 0.775). At 3 months, 20 eyes (87%) in the wavefront-optimized group and 22 eyes (96%) in the wavefront-guided group were within ± 0.50 D of emmetropia; 17 (74%) and 15 (65%), respectively, were within ± 0.25 D (P = 1.000).
Schirmer’s testing
The preoperative average Schirmer’s test value for the wavefront- optimized group was 16.4 ± 9.43 mm and 15.9 ± 9.02 mm for the wavefront-guided group. At 1 month, the values were 16.2 ± 9.75 mm and 15.8 ± 8.38 mm for the wavefront-optimized and wavefront-guided groups, respectively. The 3-month postoperative values were 15.4 ± 8.89 mm for the wavefront-optimized and 15.7 ± 8.43 mm for the wavefront-guided group. There were no significant changes in Schirmer’s testing data between both groups before or after surgery (P ≥ 0.591).
Contrast sensitivity
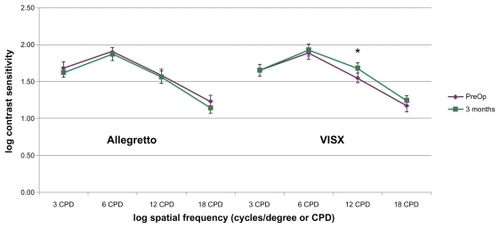
There were no significant changes in wavefront-optimized contrast sensitivity (P ≥ 0.137). The wavefront-guided group showed a significant increase in contrast sensitivity at 12 cpd following surgery (P = 0.013), but no significant changes at 3 (P = 0.909), 6 (P = 0.458), or 18 cpd (P = 0.131, ).
Higher-order aberrations
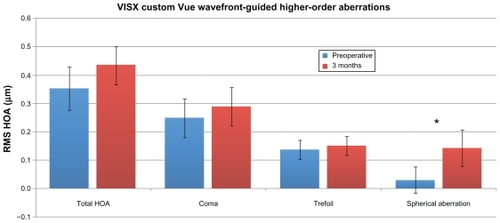
Three months following surgical correction, 87% of patients in each group completed Custom WaveScan analysis. In the wavefront- optimized group, root mean square of total higher-order aberration (P = 0.091), coma (P = 0.115), and trefoil (P = 0.459) all showed an increasing trend 3 months postoperatively, with a statistically significant two-fold increase in spherical aberration (P = 0.014, ). In the wavefront-guided group, spherical aberration had a significant three-fold (P = 0.014) increase while root mean square of total higher-order aberration (P = 0.113), coma (P = 0.403), and trefoil (P = 0.603) increased, but without statistical significance (). Although spherical aberration showed a statistically significant increase in both groups, there was no significant difference when comparing this change between the wavefront-guided and wavefront-optimized platforms (P ≥ 0.320).
Figure 2 Comparison of higher-order aberrations before surgery (n = 20) and 3 months postoperatively (n = 20) in the wavefront optimized platform. Total, coma, Z(3, 1), trefoil, Z(3, 3), and spherical aberration, Z(4, 0) were measured using the Wavescan at a mean diameter of 6 mm. RMS HOA = root-mean-square higher-order aberration
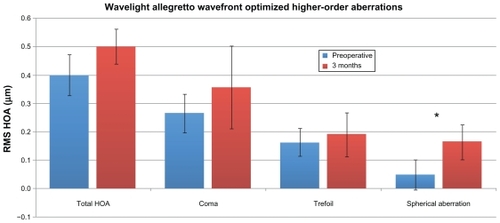
Figure 3 Comparison of higher-order aberrations before surgery (n = 20) and 3 months postoperatively (n = 20) in the wavefront-guided platform. Total, coma, Z(3, 1), trefoil, Z(3, 3), and spherical aberration, Z(4, 0) were measured using the Wavescan at a mean diameter of 6 mm. (p ≥ 0.126). RMS HOA = root-mean-square higher order aberration.
Quality of life
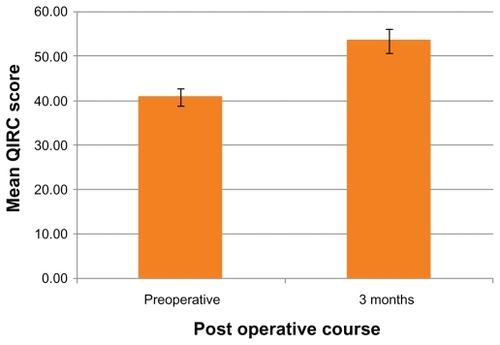
Mean QIRC values were obtained preoperatively and 3 months postoperatively (). Postoperative mean QIRC increased by 31% over the preoperative mean QIRC (P < 0.001).
Complications
No intraoperative complications occurred in the study population. Observed complications included superficial punctate keratopathy leading to loss of one line of corrected distance visual acuity for a patient in the wavefront-guided group, and a central island leading to residual astigmatism and loss of one line of corrected distance visual acuity for a patient in the wavefront-optimized group.
Discussion
There are numerous studies comparing wavefront-optimized and wavefront-guided platforms in LASIK, which have generally shown a lack of reproducible evidence favoring one platform over the other.Citation17–Citation22 To the best of our knowledge, this is the first reported study comparing these platforms in photorefractive keratectomy. The findings of our prospective, randomized, fellow-eye study support previous research that the VISX CustomVue wavefront-guided and the WaveLight Allegretto wavefront-optimized platforms are both effective and predictable in photorefractive keratectomy.Citation24–Citation26 Falavarjani et al showed that the wavefront-optimized Allegretto platform and a topography-guided platform had similar statistical outcomes.Citation26 Bababeygy and Manche observed that the VISX CustomVue platform used in photorefractive keratectomy was both safe and effective for low-to-moderate and high myopia, as well as compound myopic astigmatism.Citation25 In our study, there were no statistically significant differences in outcomes of uncorrected distance visual acuity, corrected distance visual acuity, root mean square of total higher-order aberration, or dry eye at 3 months postoperatively.
Our data showed a statistically significant increase in spherical aberration in both study platforms. However, when comparing the change induced by the wavefront-guided platform with the wavefront-optimized platform, there was no statistically significant difference. There was a nonstatistically significant increasing trend in all other higher-order aberration measures in both groups. Moshirfar et al also observed a trend similar to our results in their wavefront-guided photorefractive keratectomy vs LASIK study, showing postoperative increases in root mean square total higher-order aberration, coma, and spherical aberration for photorefractive keratectomy patients at 6 months. However, they also showed fewer induced higher-order aberrations in the photorefractive keratectomy group when compared with the LASIK group.Citation24 Randleman et al compared wavefront-optimized photorefractive keratectomy and 3-month LASIK outcomes using the Allegretto platform, and, in contrast with our study, showed no significant induction of higher-order aberrations.Citation16
The study showed a small statistically significant advantage exclusively at 12 cpd of contrast sensitivity for the VISX CustomVue platform. This supports other research, because Awwad et al compared two wavefront-guided platforms (VISX CustomVue and Alcon CustomCornea) in LASIK surgery, and reported statistically significant improvement in contrast sensitivity for both platforms.Citation27 Although we are unsure of the reason for this improvement in contrast sensitivity in the wavefront-guided group, we speculate that it may be a benefit of the custom ablation pattern. Further follow-up is needed to determine if this outcome will be sustained.
For quality of life measures, we observed significant increases in ratings postoperatively. Because the QIRC does not separate ratings based on right eye outcomes and left eye outcomes, we were unable to compare VISX Custom- Vue with Allegretto WaveLight. However, Yu et al showed no significant difference in objective measurements on the QIRC questionnaire when comparing wavefront-guided with wavefront-optimized LASIK.Citation28 We also administered a separate subjective survey; however, due to limited data, we were not able to derive conclusions from these data. Brief subjective surveys after LASIK have allowed for conclusions in previous literature,Citation29 and we believe our 10-item survey instrument would benefit from a larger sample size.
Our study showed that one eye lost one line of corrected distance visual acuity in each of the study groups. The patient in the wavefront-optimized group was found to have residual astigmatism due to a central island. In the wavefront-guided group, the loss was determined to be due to irregular corneal epithelium secondary to superficial punctate keratopathy. Both patients have been treated with ocular lubricating agents and will be re-evaluated postoperatively at 6 months.
Limitations of the study include a small sample size and short-term follow-up. It is well known that final refractive and visual acuity outcomes in photorefractive keratectomy can take beyond 3 months to become established, although results are typically permanent and finalized at 6-month follow-up.Citation30,Citation31 Serrao et al recently concluded in their 6-year follow-up study that the higher-order aberrations after traditional photorefractive keratectomy stabilized after 1 year for myopia up to −9.00 D.Citation32 Similarly, long-term analysis of wavefront photorefractive keratectomy can provide more information on stability of induced higher-order aberrations, which we hope to obtain in the future.
A potential limitation in comparing the VISX wavefront-guided platform with the Allegretto wavefront-optimized platform is the use of the VISX CustomVue WaveScan aberrometer to determine higher-order aberrations for both platforms. The WaveScan aberrometer is specifically designed for the STAR S4 platform. One may argue that the aberrometer (WaveLight® Analyzer, Alcon Inc) made for use with the Allegretto platform may have shown different results. However, use of a single aberrometer platform to compare various wavefront platforms has been documented in the literature.Citation18,Citation21 A final possible limitation is the exclusive use of Schirmer’s testing in our study to measure dry eye symptoms. Tear film stability, measured via dry eye symptoms and tear break-up time, may have enhanced our analysis on the impact of photorefractive keratectomy on the patients’ eyes.
In conclusion, there were no significant differences in visual acuity, refractive error, or dry eye between the wavefront-guided VISX CustomVue STAR S4 IR Excimer Laser with ActiveTrack iris registration and the wavefront-optimized WaveLight Allegretto Wave Eye-Q Laser for photorefractive keratectomy. While not statistically significant, a greater percentage of patients in the wavefront-guided group achieved 20/15 uncorrected distance visual acuity. VISX CustomVue showed improved contrast sensitivity at 12 cpd. Both platforms induced spherical aberration after photorefractive keratectomy surgery at 3-month follow-up, and other higher-order aberration values had a tendency to increase as well. However, we observed no statistically significant difference between the changes in spherical aberration when comparing the two platforms. We feel that both lasers are equally effective in treating refractive errors in photorefractive keratectomy.
Acknowledgments
This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the Public Health Services, National Center for Research Resources, and Research to Prevent Blindness Foundation, New York, NY.
Disclosure
The authors have no financial interests in any materials or products discussed in the manuscript or any other conflicts of interest to report in this work.
References
- AlioJLArtolaAClaramontePJAyalaMJSanchezSPComplications of photorefractive keratectomy for myopia: Two year follow-up of 3000 casesJ Cataract Refract Surg19982456196269610444
- ShojaeiAMohammad-RabeiHEslaniMElahiBNoorizadehFLong-term evaluation of complications and results of photorefractive keratectomy in myopia: An 8-year follow-upCornea200928330431019387232
- EpsteinDFagerholmPHamberg-NystromHTengrothBTwenty-four- month follow-up of excimer laser photorefractive keratectomy for myopia. Refractive and visual acuity resultsOphthalmology19941019155815638090458
- OshikaTKlyceSDApplegateRAHowlandHCEl DanasouryMAComparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusisAm J Ophthalmol19991271179932992
- MrochenMKaemmererMMierdelPSeilerTIncreased higher-order optical aberrations after laser refractive surgery: A problem of subclinical decentrationJ Cataract Refract Surg200127336236911255046
- YoonGMacraeSWilliamsDRCoxIGCauses of spherical aberration induced by laser refractive surgeryJ Cataract Refract Surg200531112713515721705
- Moreno-BarriusoELlovesJMMarcosSNavarroRLlorenteLBarberoSOcular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracingInvest Ophthalmol Vis Sci20014261396140311328757
- KulkamthornTSilaoJNTorresLFWavefront-guided laser in situ keratomileusis in the treatment of high myopia by using the CustomVue wavefront platformCornea200827778779018650664
- ChalitaMRChavalaSXuMKruegerRRWavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topographyOphthalmology2004111344745315019317
- BuhrenJMartinTKuhneAKohnenTCorrelation of aberrometry, contrast sensitivity, and subjective symptoms with quality of vision after LASIKJ Refract Surg200925755956819662912
- YamaneNMiyataKSamejimaTOcular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusisInvest Ophthalmol Vis Sci200445113986399015505046
- LiangJWilliamsDRMillerDTSupernormal vision and high-resolution retinal imaging through adaptive opticsJ Opt Soc Am A Opt Image Sci Vis19971411288428929379246
- MrochenMKaemmererMSeilerTWavefront-guided laser in situ keratomileusis: Early results in three eyesJ Refract Surg200016211612110766379
- KohnenTBuhrenJKuhneCMirshahiAWavefront-guided LASIK with the Zyoptix 3.1 system for the correction of myopia and compound myopic astigmatism with 1-year follow-up: Clinical outcome and change in higher order aberrationsOphthalmology2004111122175218515582071
- ZhouCChaiXYuanLHeYJinMRenQCorneal higher-order aberrations after customized aspheric ablation and conventional ablation for myopic correctionCurr Eye Res200732543143817514528
- RandlemanJBPerez-StraziotaCEHuMHWhiteAJLoftESStultingRDHigher-order aberrations after wavefront-optimized photorefractive keratectomy and laser in situ keratomileusisJ Cataract Refract Surg200935226026419185240
- PadmanabhanPMrochenMBasuthkarSViswanathanDJosephRWavefront-guided versus wavefront-optimized laser in situ keratomileusis: Contralateral comparative studyJ Cataract Refract Surg200834338939718299062
- BrintSFHigher order aberrations after LASIK for myopia with alcon and wavelight lasers: A prospective randomized trialJ Refract Surg2005216S799S80316329383
- TranDBShahVHigher order aberrations comparison in fellow eyes following IntraLase LASIK with WaveLight Allegretto and CustomCornea LADARVision4000systemsJ Refract Surg2006229S961S96417124897
- StonecipherKGKezirianGMWavefront-optimized versus wavefront-guided LASIK for myopic astigmatism with the Allegretto Wave: Three-month results of a prospective FDA trialJ Refract Surg2008244S424S43018500097
- Perez-StraziotaCERandlemanJBStultingRDVisual acuity and higher-order aberrations with wavefront-guided and wavefront-optimized laser in situ keratomileusisJ Cataract Refract Surg2010363437S44120202542
- MiraftabMSeyedianMAHashemiHWavefront-guided vs wavefront-optimized LASIK: A randomized clinical trial comparing contralateral eyesJ Refract Surg201027424525020839665
- PesudovsKGaramendiEElliottDBThe Quality of Life Impact of Refractive Correction (QIRC) Questionnaire: Development and validationOptom Vis Sci2004811076977715557851
- MoshirfarMSchliesserJAChangJCVisual outcomes after wavefront-guided photorefractive keratectomy and wavefront-guided laser in situ keratomileusis: Prospective comparisonJ Cataract Refract Surg20103681336134320656157
- BababeygySRMancheEEWavefront-guided photorefractive keratectomy with the VISX platform for myopiaJ Refract Surg201127317318020873706
- FalavarjaniKGHashemiMModarresMSanjariMSDarvishNGordizATopography-guided vs wavefront-optimized surface ablation for myopia using the WaveLight Platform: A contralateral eye studyJ Refract Surg2011271131720349856
- AwwadSTBowmanRWCavanaghHDMcCulleyJPWavefront-guided LASIK for myopia using the LADAR CustomCornea and the VISX CustomVueJ Refract Surg2007231263817269241
- YuJChenHWangFPatient satisfaction and visual symptoms after wavefront-guided and wavefront-optimized LASIK with the WaveLight platformJ Refract Surg200824547748618494340
- MoshirfarMHatchBBChangJCKurzCJEugarriosMFMifflinMDProspective, contralateral comparison of 120-mum and 90-mum LASIK flaps using the IntraLase FS60 femtosecond laserJ Refract Surg201027425125920672771
- HatchBMoshirfarMOllertonASikderSMifflineMA prospective, contralateral comparison of photorefractive keratectomy (PRK) versus thin-flap LASIK: Assessment of visual functionClin Ophthalmol2011545145721573091
- SladeSDurrieDBinderPA prospective, contralateral eye study comparing thin-flap LASIK (sub-Bowman keratomileusis) with photorefractive keratectomyOphthalmology200911661075108219486798
- SerraoSLombardoGDucoliPLombardoMOptical performance of the cornea six years following photorefractive keratectomy for myopiaInvest Ophthalmol Vis Sci201152284685721051709