Abstract
Introduction
Intravitreal injection of ranibizumab has become one of the most commonly performed ophthalmic procedures. It is timely to conduct an evaluation of the injection procedure from the patient’s perspective so as to determine ways to improve patient experience. The purpose of this study was to quantitatively describe patients’ experiences of the different stages of the intravitreal injection procedure and provide suggestions for improvement.
Method
Following intravitreal injection, patients were administered a questionnaire to score the distress felt for each of ten parts of the whole injection process from the initial waiting to the final instillation of topical antibiotic at the end. A score of higher than 4 was regarded as significantly unpleasant. The proportion of scores above 4 for each step was used to evaluate the relative distress experienced by patients for the different parts of the procedure.
Results
A total of 42 patients were surveyed. The step with the highest percentage of patients scoring more than 4 was the injection step (19%). However, cumulatively, the steps relating to the application of the drape, the speculum, and the removal of drape accounted for 53% of scores greater than 4.
Conclusion
There is considerable variation in how patients tolerate different stages of the injection procedure. The needle entry was the most unpleasant step followed by the draping steps cumulatively. Use of subconjunctival anesthesia, a perforated drape, and alternative lid exclusion devices may help to improve the patient’s tolerability of the procedure and experience.
Introduction
Intravitreal injection of ranibizumab is now an established treatment modality in wet age-related macular degeneration (AMD) and has become one of the most commonly performed ophthalmic surgical procedures in our clinical practice. In a hospital department providing services for a population of about 500,000 it is estimated that about 50–100 injection procedures are performed every week.Citation1 It is also a procedure that is experienced repeatedly by any individual patient who is being treated for wet AMD. Although the frequency of injections varies widely from patient to patient, on average about ten injections per eye are required over a 2-year period.Citation2
It is also anticipated that an increasing number of patients, especially those of a younger age group, will require intravitreal injections as the indications for intravitreal ranibizumab extend to include other conditions such as diabetic macular edema and retinal vein occlusions. It is timely, therefore, to conduct an evaluation of the intravitreal injection procedure from the perspective of the patient to learn about the experiences of the patient undergoing repeated injections and also to determine whether there are ways to improve the technique.
The objective of this study was to quantitatively describe the patients’ experiences by determining their opinion on separate and distinct steps of the whole injection process.
Methods
Patients attending for routine injection visits as part of a two-stop wet AMD treatment program were intended for the study. Prior to listing for intravitreal ranibizumab, patients were fully counseled. This included details of the procedure including what to expect during and following the procedure. During the surgical visits, patients typically followed a fixed pathway of procedures, which included: logMAR visual acuity measurement; and instillation of topical proxymethocaine 0.5%, tropicamide 1%, and chloramphenicol 0.5% (Chauvin Pharmaceuticals, Surrey, UK) before entering a clean room for the injection procedure. A questionnaire was designed to capture the detail of patients’ experiences of the injection procedure by dividing the process into ten discreet steps, each of which was scored by patients using a visual analogue scale. The ten discreet steps included: (1) waiting for injection, (2) instillation of drops, (3) application of drape, (4) cutting of drape, (5) insertion of speculum, (6) povidone flush, (7) needle entry, (8) irrigation, (9) speculum and drape removal, and (10) instillation of antibiotics. In the pilot study, patients did not comment on post procedure symptoms (such as floaters) being of concern, and therefore these were not included in the questionnaire.
Patients attending for a routine injection visit and who had had five or more injections previously were invited to participate. Patients who had had less than five previous injections were not recruited, as in our experience they tended to be more anxious and their recall post procedure was less accurate. Patients were given explanatory information about the study prior to entering the clean room. Trained retinal specialists and experienced ophthalmologists performed all injections. A nurse immediately at the end of the injection procedure administered the questionnaire. Patients were asked to rank their experience for each of the ten steps on a visual analogue scale of 1–10, with 1 being the most bearable and 10 most unpleasant. Comments from patients who expressed specific concerns were noted. The results of the questionnaire were tabulated and analyzed with descriptive statistics. An arbitrary discomfort cutoff score of 4 or more was used as significant (significant discomfort).
Results
Forty-two (14 female, 28 male) patients completed questionnaires. The mean age of the cohort was 76 years. At the time of completing the questionnaire the mean number of previous injections experienced by the participants was 7.80.
The distributions of the mean and range of scores for each step are shown in . In terms of proportions of patients scoring each item as significantly uncomfortable or unpleasant (ie, >4), the most unpopular steps included waiting for injection, application of drape, insertion of speculum, and also the needle entry itself. The proportions of patients scoring each step as significantly unpleasant are shown in . When the steps associated with the whole draping process were grouped together, they accounted for 53% of the high scorers (). Following the “draping process,” the injection itself accounted for 19%, and waiting in the waiting area accounted for 13% of patient discomfort.
Figure 1 Distribution of patients’ responses of significant discomfort (score ≥ 4) for each step of the intravitreal injection procedure.
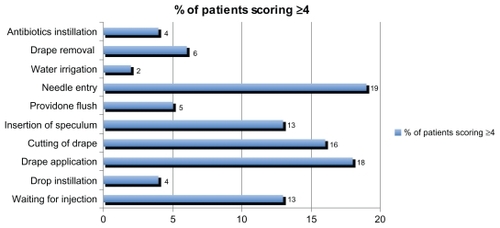
Figure 2 Distribution of patients’ responses of significant discomfort (score ≥ 4) with the “draping process,” grouped as a whole. The draping process accounts for 53% of the total number of significant discomfort responses.
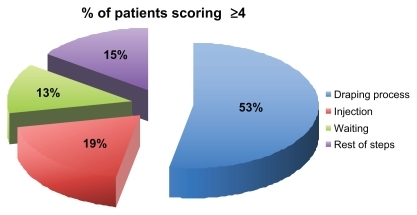
Table 1 Mean and range of scores for each step of the intravitreal injection procedure
In terms of comments, patients frequently repeated four comments. These were, despite having multiple injections: the experience is not any easier; fear as scissors (to cut the drape) pass over the eye, fear when seeing the injection needle coming, and discomfort when the drape is placed on and taken off.
Discussion
The intravitreal injection procedure is fairly standardized in the UK, with guidelines provided by the Royal College of Ophthalmologists that aim to ensure that the procedure is safe and sterile.Citation3 Other publications from outside the UK have also provided guidance on best practice for the intravitreal injection procedure.Citation4,Citation5
Patients with less than five previous injections were not recruited due to greater anxiety levels and poorer post-procedure recall of their experience. Chua et al (2009)Citation6 demonstrated in a group of treatment-naïve (34%) and previously treated (66%) patients that the anticipated discomfort was 31% higher compared with the actual discomfort experienced during the procedure. Chua et al did not perform subgroup analysis but, in our experience of over 5000 intravitreal injections, patients who are treatment naïve or have had less than five injections tend to be more anxious, with poorer recall.
In this study of the patient experience of the intravitreal injection procedure, there was a wide variation in the scores given by patients rating the discomfort of the various steps. These findings were supported qualitatively by the patients’ comments.
There have been several publications reviewing patients’ visual experiences during intravitreal injections,Citation7 cataract surgery,Citation8–Citation10 and during vitreoretinal surgery.Citation11 The evaluation of patients’ experiences during procedures under local anesthesia can help towards design of more patient-friendly techniques and procedures. This approach has been shown to result in patient-orientated approaches, especially in eye surgery when emotive factors are naturally more relevant to patients.Citation7–Citation11
The findings in this study can potentially help us improve patients’ experiences around the repeated exposures to intravitreal injections that they have to endure. Although it is widely acceptable for injections to be carried out under topical anesthesia, it is clear that a significant proportion of patients experience discomfort and express this as a variety of levels in a visual analogue scale. This single factor could be safely addressed by the use of a small quantity of subconjunctival anesthetic. Since the completion of this study, we have offered this option, especially to those patients who repeatedly feel a high level of discomfort; to date we have received good feedback.
The placement of a drape and insertion of speculum is necessary to exclude the lid margins and lashes from the surgical field and to prevent direct touch of the needle shaft with the lid margin or lashes. This is a very important aspect of the aseptic procedure and cannot be easily abandoned. An alternative to the standard ophthalmic drape is a pre-perforated drape, which obviates the need to cut the drape with scissors. Alternatively, recent developments of intravitreal injection aids which exclude the lids without a need for a drape and speculum, such as the Veni Vedi Invitria® device (FCI Surgical Devices, Paris, France)Citation12 may help. However, the substitution of the conventional speculum and drape with such a device represents a major change in technique, which warrants future studies or prospective surveillance for safety.
This study has highlighted some of the issues surrounding the tolerability of repeated injections for patients. Although these effects are transient and do not lead to any permanent clinical morbidity, they occur very frequently in a large number of patients and also frequently for individuals undergoing injections repeatedly. Implementation of steps to improve unpleasant aspects, such as sensation of needle entry and also the draping and speculum application procedures, where possible, should enable us to improve the patients’ experiences considerably.
Disclosure
The authors report no conflicts of interest in this work.
References
- AmoakuWAudit: Summary of Survey on Provision of AMD Services – March 2009 Available from: http://www.rcophth.ac.uk/page.asp?section=295&searc=Accessed April 4, 2011
- LalwaniGARosenfeldPJFungAEVariable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO StudyAm J Ophthalmol200914818791891
- AmoakuWPearceIBrowningAGuidelines for Intravitreal Injection ProcedureThe Royal College of OphthalmologistsUK2009 Available from: http://www.rcophth.ac.uk/page.asp?section=451§ionTitle=Clinical+GuidelinesAccessed on April 4, 2011
- AielloLPBruckerAJChangSEvolving guidelines for intravitreous injectionsRetina200424S3S1915483476
- FrenkelREPHajiSALaMFrenkelMPCReyesAA protocol for the retina surgeon’s safe initial intravitreal injectionsClin Ophthalmol2010411279128521139676
- ChuaPYSMitrutIArmbrechtAMVaniAAslamTDhillonBEvaluating patient discomfort, anxiety, and fear before and after ranibizumab intravitreous injection for wet age-related macular degenerationArch Ophthalmol2009127793994019597121
- CharalampidouSNolanJOrmondeGOBeattySVisual perceptions induced by intravitreous injections of therapeutic agentsEye20112549450121274011
- Au EongKGLeeHMLimATHVoonLWYongVSHSubjective visual experience during extracapsular cataract extraction and intraocular lens implantation under retrobulbar anaesthesiaEye19991332532810624426
- AngCLAu EongKGLeeSSGChanSPTanCSHPatients’ expectation and experience of visual sensations during phacoemulsification under topical anaesthesiaEye20072191162116716710431
- O’BrienPDFulcherTWallaceDPowerWPatient pain during different stages of phacoemulsification using topical anesthesiaJ Cataract Refract Surg200127688088311408135
- VohraSBAnyaCFarooqTMurrayPISubjective visual perceptions during vitreoretinal surgery under local anaesthesiaEye20092391831183518949005
- FCI Surgical Devices, Paris FranceVeni Vedi Invitria® device product information Available from: http://www.fciworldwide.com/retina/invitria.html