Abstract
Purpose
To analyze the patterns, causes, and outcome of pediatric ocular trauma at Assiut University Hospital in Upper Egypt (South of Egypt).
Methods
All ocular trauma patients aged 16 years or younger admitted to the emergency unit of Ophthalmology Department of Assiut University between July 2009 and July 2010 were included in the study. The demographic data of all patients and characteristics of the injury events were determined. The initial visual acuity and final visual acuity after 3 months follow-up were recorded.
Results
One hundred and fifty patients were included. The majority of injuries occurred in children aged 2–7 years (50.7%). There were 106 (70.7%) boys and 44 (29.3%) girls. The highest proportion of injuries occurred in the street (54.7%) followed by the home (32.7%). Open globe injuries accounted for 67.3% of injuries, closed globe for 30.7%, and chemical injuries for 2%. The most common causes were wood, stones, missiles, and glass. LogMar best corrected visual acuity at 3 months follow-up was: 0–1 in 13.3%; <1–1.3 in 27.3%; <1.3–perception of light (PL) in 56%; and no perception of light (NPL) in 3.3%.
Conclusions
Pediatric ocular trauma among patients referred to our tertiary ophthalmology referral center in Upper Egypt over a period of 1 year was 3.7%. Of these, 67.3% of cases had open globe injury, 30.7% had closed injury, and only 2% had chemical injury. In Upper Egypt, socioeconomic and sociocultural status, family negligence, and lack of supervision are important factors in pediatric eye injuries, as 92% of children were without adult supervision when the ocular trauma occurred. Nearly 86.6% of children with ocular trauma end up legally blind. Modification of these environmental risk factors is needed to decrease pediatric ocular morbidity.
Keywords:
Introduction
Ocular trauma is an important, preventable, worldwide public health problem. The etiology, severity, and outcome of ocular trauma depend on many factors in the environment that are constantly changing.Citation1 Trauma is a significant cause of monocular blindness. In population-based surveys, the percentage of monocular blindness due to trauma ranged from 20%–50% and of bilateral blindness from 3.2%–5.5%. Hospital-based studies of eye trauma indicate that about two-thirds of those affected are males, predominantly children and young adults. Injuries with sticks, stones, and metallic objects are the most common. The use of traditional eye medicine is common, and its use potentially worsens otherwise minor conditions and delays treatment for serious injury and disease.Citation2 Children often report the injury after substantial damage has already occurred. They are not aware of the objects or circumstances which can lead to ocular injury with grave visual consequences. Delayed medical and surgical intervention in pediatric ocular trauma cases often leads to poor visual outcome. Identifying the etiologies of such injuries among children may help in determining the most effective measures to prevent visual loss.Citation3 Pediatric ocular trauma has a significant impact on the future quality of life as patients are exposed to a major risk of amblyopia.Citation4
Ocular injury occurs in three forms: open globe, closed globe, and chemical injuries. Open globe injuries are one of the common emergencies in ophthalmologic clinics and require immediate operation.Citation5 Nearly 90% of eye injuries can be prevented by relatively simple measures such as better education, appropriate use of safety eye wear, and removal of common and dangerous risk factors.Citation6 Despite the fact that ocular trauma is an important worldwide cause of preventable monocular blindness, scant information is available regarding its epidemiology outside the United States and other developed countries. In developing countries, most published studies are based on data provided by outpatient departments, hospital admission/discharge, or emergency departments. Consequently, reliable estimates of incidence in developing countries are not available. Citation7 There is a high rate of ocular trauma in Upper Egypt.Citation8
The purposes of this study were to analyze the epidemiological factors, causes, and the outcome of pediatric ocular trauma at Assiut University Hospital, in Upper Egypt, and also to suggest prevention plans for the most common injuries.
Materials and methods
This descriptive, interventional, noncomparative study included ocular trauma in children aged 16 years or younger admitted to Assiut University Hospital over 1 year from July 2009 to July 2010. Assiut University Hospital is the largest hospital in Upper Egypt. It is characterized by easy access, and is a catchment area for Assiut Governorate, located close to the river Nile, as well as nearby Governorates. The population of Assiut Governorate is about 3 million. The hospital has highly qualified medical staff, good equipment, and facilities, encouraging referral from near as well as distant areas. Subjects who had received open globe injury repair elsewhere, who had undergone any ocular surgery in the past 3 months, or who had injury in the atrophic eye were excluded from the study.
Data regarding the demographic characteristics of patients were collected including: child age; sex; activity; place; cause; date of trauma; time before seeking medical care; and presence and level of attention of an adult at the time of the accident.
Information on the income and educational level of the parents was also obtained. The income level of the family was defined in relation to an income level of 100 pounds (US$20) per month: low = up to 100 pounds (US$20) per month; average = up to 300 pounds (US$60) per month; and high = more than 300 pounds (US$60) per month.
All patients had baseline clinical examinations which included: Snellen visual acuity examination by Illiterate C chart; naming picture or matching letters for young children; slit lamp examination of the anterior segment; intraocular pressure measurement using applanation tonometry in closed injury; fundus biomicroscopy with volk 90 and 78 diopter lenses; and dilated fundus examination with indirect ophthalmoscopy if possible. Diagnosis and treatment, either medical or surgical, were recorded. Follow-up for 3 months after injury with final visual acuity was recorded. Decimal visual acuity data were converted into logarithm of the minimum angle of resolution (logMAR) values and hand motion was converted into a decimal visual acuity of 0.002.
The patients were examined each day during hospitalization, every week during the first month, and every month until 3 months. Before data collection, the objectives of the study were explained using a verbal process. Written consent from the patients and their family and agreement to participate in the study was obtained.
Statistical analysis was assessed using a t-test (v 13; SPSS Inc, Chicago, IL). Descriptive analysis was used in the form of frequency, percentages, mean, and standard deviation (SD). A P-value of less than 0.05 was considered statistically significant, and highly significant when it was less than 0.001. The study adhered to the guidelines of the Declaration of Helsinki and was conducted after Assiut Faculty of Medicine institutional review board approval.
Results
A total of 150 children were admitted to the hospital with ocular injuries during the study period. The sociodemographic characteristics of children with eye injuries including, age, sex, governorate, level of education, and family income are displayed in . Results showed that pediatric ocular trauma (patients aged 2–16 years) among patients attending the ophthalmology department over a period of 1 year was 3.7%.
Table 1 Characteristics of children with eye injuries
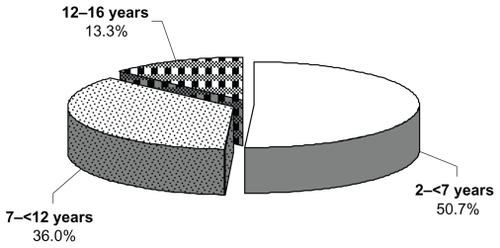
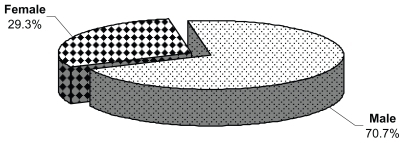
shows that the patients were divided into three groups according to age: 2–<7 years; 7–<12 years; and 12–16 years. Seventy-six patients (50.7%) were 2–<7 years old. Injury occurred more commonly in boys than in girls (3:1 ratio, see and ). More than half of the cases (64.7%) were from Assiut Governorate and only 1.3% were from Aswan Governorate. Parents with only primary education constituted 38% of the sample, secondary education 51%, and college education 11%. It was noted that there were no severe injuries in children whose parents had college-level education. One hundred and thirty-eight patients (92%) were alone or without adult supervision when the ocular trauma occurred, while twelve (8%) were under adult supervision at the moment of the accident. Of the families involved in this study, 88.7% had low or average economic status. The characteristics of the eye injuries are displayed in .
Table 2 Characteristics of eye injuries
More eye injuries occurred at midday (46.7%) than at other times of day, and the injuries occurred most commonly in the street (54.7%), followed by home (32.7%), school (6.7%), and at work (6%). In the street injuries, open injuries constituted 65.9% of the total, while closed injuries were 34.1%.
The elapsed time between injury and seeking medical care was most commonly within the same day of trauma (31.3%) followed by after 3 days or more of trauma (24.7%). It was noted that in lower socioeconomic levels (primary education and low income level), the delay period was much longer than in higher socioeconomic levels, regardless of whether the injury was mild or severe. Sixty-eight percent (25 of 37) of patients who sought medical care more than 72 hours after injury were in the low socioeconomic level.
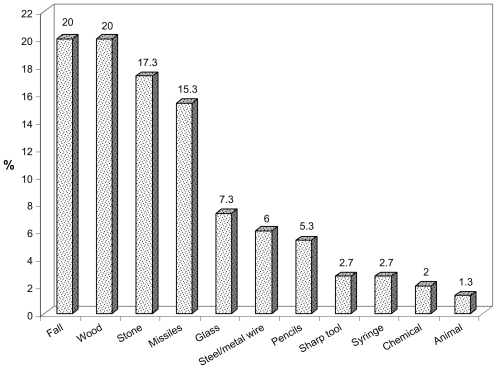
The most common cause of injury was a fall on the ground (20%), followed by wood (20%), stones (17.3%), missiles and Airsoft toy guns (15.3%), while the least common was animal injury (1.3%; ).
The most frequent findings were hyphema in closed globe injury, corneal wounds in open injury, and corneal abrasion in chemical injuries ().
Table 3 Distribution of eye injuries according to diagnosis
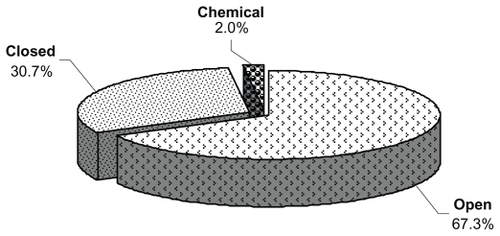
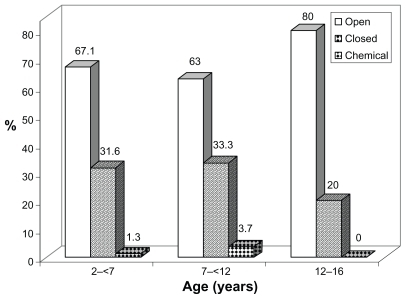
About 67.3% of cases had open globe injury, 30.7% had closed injury, and only 2% had chemical injury (). Most cases of open injury occurred in children aged 2–<7 year (51 cases). Closed injury also was highest in the same age group (24 cases), but chemical injuries were higher in the 7–<12 year group (2 cases) ( and ). Surgical management was performed in 130 children (86.6%) and medical treatment in 20 children (13.3%).
Table 4 Relationship between age and mechanism of injury
All patients in this study were admitted to the hospital with admission times ranging from 4 to 10 days. Thirty-three patients out of 130 who underwent surgery also had another surgical procedure.
The difference between the initial and final visual acuity at the end of 3 months was statistically significant using a t-test (P = 0.0005; ).
Table 5 Distribution of initial and final visual acuity
Discussion
Ocular trauma remains an important cause of avoidable and predominantly monocular visual morbidity in children. In general, children are more susceptible to eye injuries because of their immature motor skills, and their tendency to imitate adult behavior without evaluating risks.Citation9
Socioeconomic and sociocultural status and family negligence are important factors in eye injuries in children.Citation10 Patients from Upper Egypt accounted for 56.2% of ocular emergencies in a large 5-year study on the epidemiology of ocular emergencies in the Egyptian population.Citation8
Our study was a hospital-based study among children attending the ophthalmology department in Assiut University Hospital. Its results showed that the percentage of pediatric ocular trauma among patients attending the ophthalmology department during a period of 1 year was 3.7%. This is in agreement with Dandona et alCitation11 who found a rate of ocular trauma of 3.97% in their study.
Our study showed that about 50.7% of pediatric ocular trauma occurred in children aged 2–<7 years, followed those aged 7–<12 years (36%), with the lowest incidence (13.3%) in children aged 12–16 years. Young children have in common physical vulnerability, lack of coordination, and limited ability to avoid or escape from danger. Also young children show curiosity and a desire to explore, which may expose them to serious hazards. Abraham et al found that one-third of the injuries occurred in those less than the age of 20 years.Citation12 Also, Niiranen and Raivio found that children with ocular trauma represented 34.5% of all eye injuries and 3% of all patients treated.Citation13 El-Mekawey et al found that pediatric ocular trauma constituted 37.1% of all ocular emergencies in a 5-year study in Egypt.Citation8
In our study, 70.7% of cases were males (male to female ratio 3:1). Male predominance may be related to social and or environmental factors, as males are allowed to go outdoors more and also undertake hard jobs with high levels of physical contact. The aggressive nature of males may also be a factor. An Egyptian ocular trauma study reported that 69% of patients were males.Citation8 Our study showed that 38% of parents were illiterate and this could be a cause of the high rate of pediatric trauma in our locality.
In lower socioeconomic levels there was a delay in the time between receiving the injury and seeking medical care. Sixty-eight percent (25 of 37) of patients who sought medical care more than 72 hours after injury were in the low socioeconomic level. This may reflect deficient parental supervision in the lower socioeconomic level.
Our study showed that no persons were present with children during time of trauma in 92% of cases, indicating negligence and lack of supervision during play, and increased participation in outdoor activities without strict adult supervision. The present study showed that a higher frequency of ocular trauma occurred on roads (54.7%), followed by home (32.7%), school (6.7%), and finally the workplace (6%). This agrees with Kaimbo,Citation14 who stated that street- and home-related injuries accounted for 54% of all ocular injuries, while work-related injuries have been reported as 13%–18% of total eye trauma cases.
Wood was the cause of injury in 20% of patients, followed by stones (17.3%), missiles and Airsoft toy guns (15.3%), glass (7.3%), steel (6%), pencils (5.3%), sharp tools and syringes (2.7% each), chemicals (2%: two cases caused by lime and one case by potash), and animals (1.3%). Injuries with sticks, stones, and metallic objects were also the most common in a study by Mselle.Citation15 This is in contrast to other studies which stated that 25% of ocular injuries in children are from gunshots, 24.2% from tools, and 21.8% from assault.Citation16 Our study showed that more than one-third of cases with ocular trauma (34.4%) were associated with injury to multiple parts of the eye. The most commonly injured part was the cornea with corneal wounds (45.3%), followed by the lens with traumatic cataract (33.3%), hyphema (24%), lid and conjunctival lacerations (12.7%), endophthalmitis (19.3%), corneal and conjunctival foreign body (7.3%), and disorganized globe (4.7%). In this study traumatic cataract predominated in both open and closed injuries. In open injuries, corneal wounds predominated while in closed injuries, most cases suffered from hyphema. In chemical injuries, there were corneal abrasions in addition to lid and conjunctival laceration. Corneal involvement, scleral wounds, and disorganized globe were found in 19.6%, 6.9%, and 19.1% of cases, respectively, in a study by Bejiga.Citation17 Ariturk et al found that hyphema is the most common outcome in blunt trauma, and corneal laceration in perforating injury.Citation10
In this study, penetrating injuries (open globe) formed 67.3% of cases (by either objects thrown at children or by falling on sharp objects), blunt injuries (closed globe) 30.7%, and chemical injuries 2%. Penetrating injuries, in general, carry a poor prognosisCitation18 and they are more likely to require surgery and subsequently to result in long-term visual impairment. Final visual acuity in our study was no perception of light (NPL) in 3.3% of cases; perception of light (PL)–<3/60(1.3 logMar) in 56%; 3/60(1.3 logMar)–<6/60(1 logMar) in 27.3%; and 6/60(1 logMar) – 6/6(0 logMar) in 13.3%. This means that 86.6% of children in this study ended up legally blind according to the definition of legal blindness in USA (best corrected visual acuity of 20/200 (US notation) or 6/60(6 m notation) or 1(logMar) in the better eye).Citation19 The poor visual results agree with Niiranen and RaivioCitation13 who noted that despite therapeutic advances, visual prognosis in children is still worse than adults due to the nature of the injuries and amblyopic problems.
In pediatric ocular trauma, prevention is superior to the most effective treatment of trauma. Many childhood injuries could be prevented with foresight, and good supervision from parents. Education of both parents and children about the hazards of buying certain toys and paying attention to the child’s age and responsibility level is needed. It is important to avoid projectile toys and air guns because they are capable of inflicting serious and permanent ocular damage as noticed in our study and other Egyptian studies.Citation20 Manufacturers must clearly display warnings if a toy is unsuitable for children under a certain age. Syringes that have been improperly disposed of are an important issue and a risk for pediatric ocular trauma and were the cause of injury in 2.7% of cases in our study. This subject was previously studied by Al-Hussaini et al,Citation21 who found that syringes may be a significant risk for pediatric ocular injury and visual loss.
It is necessary to have public education campaigns about ocular trauma, and recognition of specific hazards and their prevention. Health education and safety strategies should target the home as well as the street as high-risk environments.
Improving rural health services by providing them with facilities and equipment is necessary for urgent management of ocular trauma. Good training in how to deal with different types of ocular trauma is important for resident ophthalmologists. Clinicians can provide parents with information on the risk of eye injury from different objects. Disseminators of information might include pediatricians, community leaders, and school teachers.
Our data support the need for eye injury prevention efforts, taking into consideration the developmental stages of children. Eye injuries, as well many other health problems, would be positively influenced by an improvement of the socioeconomic level of the entire population.
Disclosure
The authors report no conflicts of interest in this work.
References
- WongTYEpidemiological characteristics of ocular trauma in the US ArmyArch Ophthalmol20021209123612215108
- LewallenSCourtrightPBlindness in Africa: present situation and future needsBr J Ophthalmol200185889790311466240
- MacEwenCJBainesPSDesaiPEye injuries in children: the current pictureBr J Ophthalmol199983893393610413696
- MacEwenCJOcular injuriesJ R Coll Surg Edinb199944531732310550957
- ZagelbaumBMTostanoskiJRKernerDJHershPSUrban eye trauma. A one-year prospective studyOphthalmology199310068518568510896
- Ervin-MulveyLDNelsonLBFreeleyDAPediatric eye traumaPediatr Clin North Am1983306116711836646870
- DesaiPMacEwenCJBainesPMinassianDCIncidence of cases of ocular trauma admitted to hospital and incidence of blinding outcomeBr J Ophthalmol19968075925968795369
- El-MekaweyHEEinenKGAbdelmaboudMKhafagyAEltahawyEMEpidemiology of ocular emergencies in the Egyptian population: a five-year retrospective studyClin Ophthalmol2011595596021792285
- ThordarsonURagnarssonATGudbrandssonBOcular trauma. Observation in 105 patientsActa Ophthalmol (Copenh)1979575922928525311
- AriturkNSahinMOgeIErkanDSulluYThe evaluation of ocular trauma in children between ages 0–12Turk J Pediatr1999411435210770675
- DandonaLDandonaRSrinivasMJohnRKMcCartyCARaoGNOcular trauma in an urban population in southern India: the Andhra Pradesh Eye Disease StudyClin Experiment Ophthalmol200028535035611097281
- AbrahamDIVitaleSIWestSIIssemeIEpidemiology of eye injuries in rural TanzaniaOphthalmic Epidemiol199962859410420208
- NiiranenMRaivioIEye injuries in childrenBr J Ophthalmol19816564364387260016
- KaimboWKSpileersWMissottenLOcular emergencies in Kinshasa (Democratic Republic of Congo)Bull Soc Belge Ophtalmol2002284495312161990
- MselleJVisual impact of using traditional medicine on the injured eye in AfricaActa Trop19987021851929698264
- DesaiPMacEwenCJBainesPMinassianDCEpidemiology and implications of ocular trauma admitted to hospital in ScotlandJ Epidemiol Community Health19965044364418882228
- BejigaACauses and visual outcomes of perforating ocular injuries among Ethiopian patientsCommunity Eye Health20011439454617491927
- GilbertCMSoongHKHirstLWA two-year prospective study of penetrating ocular trauma at the Wilmer Ophthalmological InstituteAnn Ophthalmol19871931041063566032
- BronAMViswanathanACThelenUInternational vision requirements for driver licensing and disability pensions: using a milestone approach in characterization of progressive eye diseaseClin Ophthalmol201041361136921179219
- ShazlyTAAl-HussainiAKPediatric ocular injuries from airsoft toy gunsJ Pediatr Ophthalmol Strabismus20111421261240
- Al-HussainiAKShazlyTASevere ocular injuries from improperly disposed medical syringes in childrenJ Pediatr Ophthalmol Strabismus201047210811020349905