Abstract
Introduction
We developed a new technique that uses two of the vitrectomy ports as intraocular lens (IOL) haptic fixation sites and compared that with a conventional T-fixation method.
Methods
A total of 33 eyes were retrospectively divided into the port-fixation (n=21) and conventional (n=12) groups. For the port-fixation group, supranasal and inferotemporal trocars (25-gauge) were placed in the center of a T-shaped lamellar scleral incision 2 mm from the corneal limbus and a supratemporal trocar at 3.5 mm. Following a vitrectomy, along with lens or IOL extraction as needed, the infusion cannula was changed from an inferotemporal to supratemporal trocar. The first IOL haptic and trocar were then simultaneously withdrawn from the eye by grasping with vitreoretinal forceps, with the same performed for the second IOL haptic and trocar, after which the infusion cannula was removed. In the conventional group, 2 T-shaped scleral incisions and three trocars were separately placed.
Results
Postoperatively, transient ocular hypotension and hypertension were observed in a few eyes in both groups. At 6 months after surgery, astigmatism was 1.71±1.13 D in the port-fixation group and 2.21±1.78 D in the conventional group (p=0.40, t-test).
Conclusion
This new technique may be effective because of the lower number of scleral wounds.
Introduction
Intrascleral fixation as a second surgery for intraocular lens (IOL) implantation, reported by GaborCitation1 in 2007 and AgarwalCitation2 in 2008, has undergone improvements, such as the use of small gauge devices for passing through the scleral tunnels.Citation3 Recently, OhtaCitation4,Citation5 reported an improved scleral incision technique, TotanCitation6,Citation7 developed a method using trocars for passing IOL haptics through the sclera, and YamaneCitation8 noted the development of a haptic tip with a flange shape to prevent drop off into the vitreous. In the cases who need vitrectomy, three ports for vitrectomy, two scleral incisions or tunnels and a corneal limbal incision for IOL insertion were needed.
To simplify the procedure for intrascleral IOL fixation for an aphakic or lens dislocated eye that also requires a simultaneous vitrectomy procedure, we have developed a new technique that uses two of the vitrectomy ports as IOL loop fixation sites and compared it with a conventional T-fixation method.
Methods
The protocol for this retrospective study was approved by the Institutional Review Committee of the Hirosaki University Graduate School of Medicine. All clinical procedures were conducted according to the principles of the Declaration of Helsinki. Written informed consent was obtained from all patients prior to the procedure, and possible complications were explained. Inclusion criteria were aphakia, lens subluxation or luxation, or IOL subluxation or luxation, while exclusion criteria were vitreoretinal disease that required a gas tamponade, high myopia, or glaucoma. All surgeries were performed by six vitreoretinal surgeons working at our hospital.
From 2015 to 2018, IOL intrascleral fixation surgery was performed for a total of 33 eyes due to IOL subluxation or dislocation into the vitreous (n=17), lens subluxation or dislocation into the vitreous (n=7), or extraction of a lens placed in a previous operation (n=9) (). Subject eyes were retrospectively divided into the port-fixation group (n=21) and conventional (T-fixation techniqueCitation4) (n=12) groups. Age and gender of the patients, and surgery for right or left eye for both groups are presented in .
Table 1 Preoperative Status
As for preoperative lens or IOL status, IOL subluxation was observed in seven eyes in the port-fixation group and two eyes in the conventional group, while IOL dislocation in the vitreous was noted in six and two eyes, respectively, lens subluxation or luxation in two and five eyes, respectively, aphakia due to previous vitreoretinal surgery in four and two eyes, respectively, and aphakia due to incomplete cataract surgery (complicated cataract surgery with posterior capsule rupture) in two and one eye, respectively ().
As for the vitrectomy procedure, in the port-fixation group, a full vitrectomy (cored and peripheral vitrectomy) was performed in 12 eyes, and a full vitrectomy with peeling of the epiretinal membrane and internal limiting membrane was performed in 1, while a peripheral vitrectomy was performed in 8 eyes that had previously undergone a cored vitrectomy. In the conventional group, a full vitrectomy was performed in 10 eyes and a peripheral vitrectomy in 2 ().
An IOL intrascleral fixation procedure was performed after a vitrectomy and extraction of the dislocated lens or IOL when needed in both groups. For the process of lens/IOL extraction in the port-fixation group, the whole IOL was floated on perfluorocarbon liquid (PFCL) and extracted in five eyes, extracted with a hook in three eyes, or divided into two pieces with IOL scissors and extracted in four eyes, while a pars plana lensectomy (PPL) was performed with a fragmatome in two eyes, the IOL dislocated in the vitreous was reused for intrascleral fixation in one eye, and no extractions of the lens/IOL were performed due to aphakia caused by previous surgery in six eyes ().
Table 2 Procedure for Lens Extraction and Vitrectomy
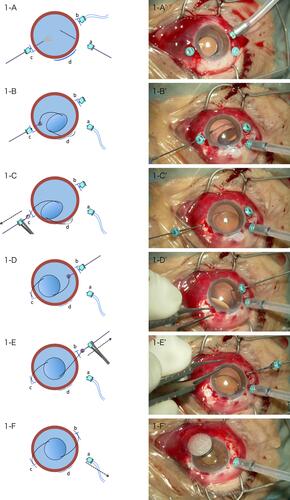
As for intrascleral IOL fixation procedure, in the port-fixation group (n=21), 2 T-shaped lamellar scleral incisions were placed at 2 mm from the corneal limbus on the opposite sites (inferotemporal and supranasal sites), 2 trocars were inserted through the sclera into the vitreous cavity at the center of those T-shaped lamellar scleral incisions, and 1 trocar was inserted through the full thickness sclera at 3.5 mm from corneal limbus at the supratemporal site (’). When the vitrectomy was finished, the infusion cannula was changed from the inferotemporal to the supratemporal trocar (’), then IOL intrascleral fixation was performed using the inferotemporal and supranasal trocars. In right eye cases, during IOL insertion, the first IOL haptic and the trocar were simultaneously withdrawn from the supranasal scleral port by grasping with 25-gauge vitreoretinal forceps (’, ’); then, the second haptic was withdrawn from the inferotemporal scleral port in the same manner (, ’, , ’). In left eye cases, during IOL insertion, the first IOL haptic and trocar were simultaneously withdrawn from the inferotemporal scleral port by grasping with 25-gauge vitreoretinal forceps; then, the second haptic was withdrawn from the supranasal scleral port in the same manner. The IOL haptic tips were mined into intrascleral incisions made with a 24-gauge micro-vitreoretinal blade (MVR); then, the incisions were sutured with 8–0 Vicryl® or 10–0 nylon, as necessary (, ’). Scleral ports for the vitrectomy were sutured when needed and miosis was obtained with intracameral acetylcholine.
Figure 1 Port-fixation group. Representative case, right eye. (A)Supranasal (c) and inferotemporal (b) trocars (25-gauge) were placed in the center of a T-shaped lamellar scleral incision 2 mm from the corneal limbus and a supratemporal trocar (a) was placed 3.5 mm from that. (B, C) Following a vitrectomy, the infusion cannula was changed from an inferotemporal to supratemporal trocar. At the time when the IOL was halfway inserted into the eye (d), the first IOL haptic and a supranasal trocar were simultaneously withdrawn through the sclera by grasping with 25-gauge vitreoretinal forceps. (D, E) The second IOL haptic and an inferotemporal trocar were simultaneously withdrawn through the sclera by grasping with 25-gauge vitreoretinal forceps. (F) Both tips of the IOL haptics were embedded into preliminary intrascleral spaces and the infusion cannula was finally removed.
In the conventional group,the whole IOL was extracted with the PFCL in two eyes, with a lens hook in two eyes, and was divided into two pieces and extracted in one eye, while five eyes underwent PPL with fragmatome, lens fragments in the vitreous were extracted with a vitreous cutter in one eye, and no extraction was performed due to aphakia in one eye.
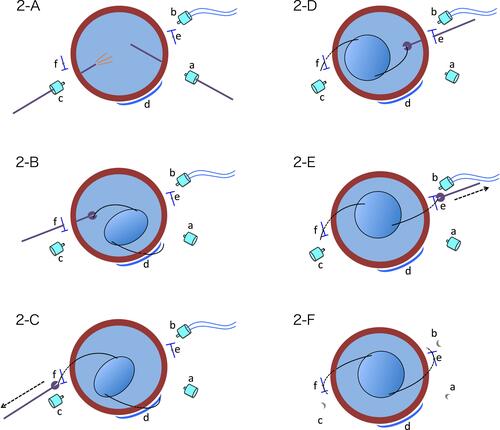
In the conventional group (n=12), 3 trocars were placed at the sclera 3.5 mm from the corneal limbus for a 3-port system vitrectomy, with the lensectomy and vitrectomy completed using 2 T-shaped lamellar scleral incisions, as reported by Ohta,Citation4 placed 2 mm from the corneal limbus at 180°opposite sides so as to avoid the trocar sites (). Next, a 25-gauge MVR was inserted through the sclera at the center of each T-shaped lamellar scleral incisions, and then an IOL was inserted, and the first IOL haptic was grasped with vitreoretinal forceps through the incision and withdrawn from the sclera (,). The second haptic was grasped in the same manner, and then the tips of the IOL haptics were mined into the intrascleral incisions made with a 24-gauge MVR, with the lamellar incisions sutured with 8–0 Vicryl® or 10–0 nylon, when necessary (–). Scleral ports for the vitrectomy were sutured as needed and miosis was obtained with intracameral acetylcholine.
Figure 2 Conventional group. Representative case,righteye. (A) Supratemporal (a),inferotemporal (b) and supranasal (c) trocars (25-gauge) were placed 3.5 mm from the corneal limbus. Two T-shaped lamellar scleral incisions were placed 2 mm from that (e,f). In the center of T-shaped lamellar scleral incisions,full-thickness scleral perforations were performed with 25-gauge MVR. (B,C) Following a vitrectomy,IOL was halfway inserted into the eye (d) and the first IOL haptic was withdrawn through the scleral perforation site (f) by grasping with 25-gauge vitreoretinal forceps. (D,E) The second IOL haptic was withdrawn through the scleral perforation site (e) by grasping with 25-gauge vitreoretinal forceps. (F) Both tips of the IOL haptics were embedded into preliminary intrascleral spaces (e,f),and two trocars (a,c) and the infusion cannula were finally removed.
The postoperative observation period ranged from 6 to 23 months (mean 13.8 months) for the port-fixation group and 6 to 30 months (mean 19.7 months) for the conventional group. Postoperative complications were noted and postoperative best-corrected visual acuity findings at 6 months after the surgery were compared to preoperative findings in both groups.
Statistical Analysis
Decimal visual acuity (VA) was converted to a logarithm of the minimum angle of resolution (logMAR) units for statistical analysis. Student’s unpaired t-test was used to compare age at the time of surgery, total operation time, postoperative observation period between the two groups, and the period between preoperative and postoperative VA in both groups.
Results
The total operation time was 118.3±25.6 mins in the port-fixation group and 134.0±27.6 mins in the conventional group (P=0.054, t-test). In the port-fixation group, intraoperative iris damage occurred in one eye (5%).
Postoperatively, transient ocular hypotension was observed in 2 (10%) eyes in the port-fixation group and in 2 (17%) in the conventional group, while transient ocular hypertension was seen in 2 (10%) and 1 (8%), respectively. Exposure of the IOL haptic outside of the conjunctival wound was observed in two eyes (10%) in the port-fixation group. Strong postoperative astigmatism greater than 5 diopters was noted in one (5%) eye in the port-fixation group and in one (8%) in the conventional group, while postoperative transient vitreous hemorrhage occurred in one (5%) and one (8%), respectively ().
Table 3 Postoperative Complications, Pre- and Postoperative Visual Acuity
Postoperative astigmatism at 6 months after surgery was 1.71±1.13 D in the port-fixation group and 2.21±1.78 D in the conventional group, which was not a significant difference (p=0.40, t-test). Preoperative and postoperative VA (logMAR) were 0.45±0.60 and 0.36±0.51, respectively, in the port-fixation group, and 0.59±0.60 and 0.36±0.50, respectively, in the conventional group (t-test: p=0.160 and p=0.116, respectively, ).
Discussion
Transscleral or intrascleral IOL fixation is generally performed for cases with aphakia after complicated cataract surgery or postoperative IOL or lens dislocation. However, because of its advantages over transscleral fixation,Citation9 intrascleral IOL fixation is now more frequently performed in such cases. Gabor,Citation1 Agarwal,Citation2 and Rodriquez-AgirretxeCitation10 have reported sutureless intrascleral IOL fixation methods using a 24- or 25-gauge MVR, while OhtaCitation4,Citation5 reported a simplified method that employs a Y-fixation lamellar scleral incision and 24-gauge MVR.
To avoid postoperative ocular hypotension, Yamane,Citation11 Can,Citation12 and KhatriCitation13 reported the use of a new method in which the IOL haptics are guided by 27-gauge needles and withdrawn from the eye. Also, YamaneCitation8 reported a novel method that used two 30-gauge thin-wall needles, which were inserted into the sclera to withdraw 2 IOL haptics, after which the tips of the haptics were cauterized using an ophthalmic cautery device to make a flange shape so as to not naturally drop into the vitreous. TotanCitation6 and HuCitation14 used modified methods with vitrectomy trocars to guide the IOL haptic thorough the scleral tunnels, while WalshCitation15 reported guidance with 27-gauge trocars and cauterization with an ophthalmic cautery device.
Intrascleral IOL fixation is a relatively new procedure, some complications such as postoperative exposure of an IOL hapticCitation16 might be encountered in the future. By reviewing various methods of sutureless scleral fixation, KaradagCitation3 mentioned that the short-term results of these new methods were acceptable and studies including more cases with longer follow-up were needed to determine their long-term success. Furthermore, some improvements and modifications are likely necessary so as to decrease postoperative complications and make the intrascleral IOL fixation easy for surgeons.
In 2019, Thanos presented a report of a 3-port sutureless posterior chamber intraocular lens intrascleral fixation technique,Citation17 which has similarities with our technique. For the present study, we attempted a mixed procedure with a small gauge vitrectomy using a 25-gauge trocar and simultaneous intrascleral IOL fixation through the same trocar within the lamellar scleral incision. There were some minor postoperative complications noted, such as transient postoperative ocular hypotension, ocular hypertension, mild vitreous hemorrhage and exposure of an IOL haptic, but none were severe. Concerning operation time and postoperative astigmatism, this new method is not inferior compared to the conventional procedure. We consider that the method is more convenient than a conventional because of the lower number of wound, thus recommend it as a procedure.
Consent for Publication
Written informed consent for publication was obtained from the patient presented the operation pictures.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The protocol for this retrospective study was approved by the Institutional Review Committee of the Hirosaki University Graduate School of Medicine. All clinical procedures were conducted according to the principles of the Declaration of Helsinki. Written informed consent was obtained from all patients prior to the procedure, and possible complications were explained.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank the patients who participated in this study and thereby made this work possible. This work will be presented at a conference of World Ophthalmology Congress 2020 in Cape Town.
Disclosure
Each author warrants that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, and patent/licensing arrangements) that might pose a conflict of interest in connection with the article.
References
- Gabor SGB, Pavilidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33(11):1851–1854. doi:10.1016/j.jcrs.2007.07.013
- Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinvasan S. Fibrin glue–assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refractive Surg. 2008;34(9):1433–1438. doi:10.1016/j.jcrs.2008.04.040
- Karadag R, Celik HU, Bayramlar H, Rapuano CJ. Sutureless intrascleral fixated intraocular lens implantation. J Refract Surg. 2016;32(9):586–597. doi:10.3928/1081597X-20160601-03
- Ohta T, Toshida H, Murakami A. Simplified and safe method of sutureless intrascleral posterior chamber intraocular lens fixation: Y-fixation technique. J Cataract Refract Surg. 2014;40(1):2–7. doi:10.1016/j-jcrs.2013.11.003
- Ohta T. Sutureless intrascleral posterior chamber intraocular lens fixation. Jpn J Clin Ophthalmol. 2014;68(13):1682–1690.
- Totan Y, Karadag R. Trocar-assisted sutureless intrascleral posterior chamber foldable intra-ocular lens fixation. Eye. 2012;26(6):788–791. doi:10.1038/eye.2012.19
- Totan Y, Karadag R. Two techniques for sutureless intrascleral posterior chamber IOL fixation. J Refract Surg. 2013;29(2):90–94. doi:10.3928/1081597X-20130117-02
- Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmol. 2017;124(8):1136–1142. doi:10.1016/j.ophtha.2017.03.036
- Sinha R, Bansal M, Sharma N, et al. Transscleral suture-fixated versus intrascleral haptic-fixated intraocular lens: a comparative study. Eye Contact Lens. 2017;43(6):389–393. doi:10.1097/ICL.0000000000000287
- Rodriguez-Agirretxe I, Acera-Osa A, Ubeda-Erviti M. Needle-guided intrascleral fixation of posterior chamber intraocular lens for aphakia correction. J Cataract Refract Surg. 2009;35(12):2051–2053. doi:10.1016/j.jcrs.2009.06.044
- Yamane S, Inoue M, Arakawa A, Kadonosono K. Sutureless 27-gauge needle-guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmol. 2014;121(1):61–66. doi:10.1016/j.ophtha.2013.08.043
- Can E. Flapless and sutureless intrascleral fixation of posterior chamber intraocular lens for correction of aphakia. J Cataract Refract Surg. 2018;44(8):929–931. doi:10.1016/j.jcrs.2018.03.037
- Khatri A, Singh S, Rijal R, Khatri BK, Kharel M. 27-gauge needle-assisted externalization and haptic securing technique for sutureless scleral fixation of the intraocular lens – moving toward simplicity. Clin Ophthalmol. 2018;12:1441–1447. doi:10.2147/OPTH.S166354
- Hu Z-X, Lin H, Ye L, Chen T, Lin K, Wu R-H. Sutureless intrascleral haptic-hook lens implantation using 25-gauge trocars. J Ophthalmol. 2018;5. doi:10.1155/2018/9250425.
- Walsh MA. Sutureless trocar-cannula-based transconjunctival flanged intrascleral intraocular lens fixation. Retina. 2017;37(11):2191–2194. doi:10.1097/IAE.0000000000001593
- Matsui Y, Matsubara H, Hanemoto T, Kondo M. Exposure of haptics of posterior chamber intraocular lens after sutureless intrascleral fixation. BMC Ophthalmol. 2015;15(1):104. doi:10.1186/s12886-015-0102-3
- Thanos A, Lau-Sjckon LK, Wolfe JD, Hassen TS. Three port sutureless posterior chamber intraocular lens intrascleral fixation: a novel approach. Retina. 2019;39(10):16–20. doi:10.1097/IAE.0000000000001925
