Abstract
Background and objective
The aim of the present study was to compare intraocular pressure (IOP) reduction and inflammation after selective laser trabeculoplasty (SLT) treatment in patients suffering from primary open angle (POAG) vs pseudoexfoliative (PXFG) glaucoma.
Study design/patients and methods
Sixty patients (60 eyes) participated in the study. Glaucoma patients (POAG or PXFG) scheduled for treatment with SLT were included. Inflammation was measured with a laser flare meter (Kowa FM-500). Measurements were made before SLT and 2 hours, 1 week, and 1 month after SLT treatment. IOP was also checked at the same time intervals.
Results
Inflammation after SLT showed no significant difference between the groups (t-test, before: P = 0.16; 2 hours: P = 0.14; 1 week: P = 0.12; and 1 month: P = 0.36). IOP reduction was the same in both groups (t-test, P = 0.27).
Conclusion
SLT safely reduces IOP in both POAG and PXFG. Pseudoexfoliation does not seem to be a risk factor for post-laser complications.
Introduction
Glaucoma is a progressive neuropathy localized in the optic nerve that may lead to blindness. Reducing intraocular pressure (IOP) seems to be the only treatment proven to slow progression in glaucoma.Citation1 There are several methods to reduce IOP: pharmaceutical treatment, laser treatment, and surgery. In the Glaucoma Laser Trial Follow-up Study, after 7 years of follow-up, patients who had undergone argon laser trabeculoplasty (ALT) had lower IOP than patients on pharmaceutical treatment.Citation2,Citation3 However, there has been no randomized trial comparing SLT to medical treatment. SLT appears to be less costly than current medical treatment.Citation4
Argon laser trabeculoplasty (ALT) was introduced about 35 years ago and involves the use of a blue/green argon laser (major wavelength peaks at 488 nm and 514 nm) to treat the outer part of the trabecular meshwork and thereby improve aqueous flow and thus reduce IOP. Selective Laser Trabeculoplasty (SLT) uses a 532-nm frequency-doubled, Q-switched Nd:YAG laser that delivers a low-energy, large spot, very brief pulse to selectively target cells of the trabecular meshwork. This “milder” laser application is thought to stimulate the pigmented trabecular meshwork cells and thus facilitate improved aqueous outflow. The exact mechanism of action for reducing the IOP is not known.Citation5
Pseudoexfoliation prevalence varies between different countries. In the US, Karger et alCitation6 showed an annual incidence of 25.9 per 100,000 (mean age 73) and found an increased number with increasing age. Although pseudoexfoliation has a worldwide distribution, it appears more common in Scandinavia. Pseudoexfoliation prevalence in northern Sweden is estimated to be 23% at 66 years and 61% at 87 years.Citation7 Pseudoexfoliative glaucoma is estimated to account for around 50% of all glaucoma patients diagnosed in Sweden.Citation8,Citation9 Information regarding the influence of pseudoexfoliation on SLT results is scarce. Gracner et alCitation10 showed no difference in SLT results (IOP reduction) comparing pseudoexfoliative and primary open angle glaucoma when ten patients were followed for 18 months. Shazly et alCitation11 showed SLT to be safe for IOP reduction as a primary treatment in PXFG. Goldenfeld et alCitation12 showed that after SLT in PXFG, the amount of medication was reduced.
The aim of the present study was to compare IOP reduction and inflammation after SLT treatment in primary open angle glaucoma (POAG) vs pseudoexfoliative glaucoma (PXFG) patients.
Patients and methods
Study design
This was a prospective nonrandomized comparative study. A comprehensive medical and ocular history was obtained. All patients were asked about present inflammatory diseases and treatments. Ophthalmological examination was performed before including patients in the study. Visual acuity, IOP measurements, optic nerve status, gonioscopy, and the presence or absence of exfoliation were registered. Visual acuity was recorded using a Snellen’s chart. IOP was measured using a Goldmann’s applanation tonometer. The optic nerve status was then evaluated using a 90-D lens through an undilated pupil. Gonioscopy was performed in a darkroom using a goniolens with an undilated pupil and the anterior chamber angle was classified into 0–IV (according to Shaffer) and pigmentation was classified into 0–3.Citation13 Pupils were dilated and exfoliation was checked; exfoliation was registered as present or absent. IOP, slit-lamp, and laser flare measurements were made before SLT and 2 hours, 1 week, and 1 month after SLT. All included patients had at least two reliable visual fields showing typical glaucoma visual field damage. Visual fields were checked using the Humphrey 24-2, SITA fast program (Carl Zeiss Meditec, Inc, Dublin, CA). For calculations, an average of the values of mean deviation (MD) and visual field index (VFI) were calculated using the two last visual fields.
The SLT is a Q-switched, frequency-doubled Nd:YAG, with a wavelength around 532 nm. The SLT uses a single pulse (pulse duration 3 ns) and the spot size is estimated to be 400 μm. In the present study, SLT treatment was performed over 90° with the SLT Solo laser (Ellex, Australia) using some 25–30 spots applied to the trabecular meshwork. Traditionally, 180° of the trabecular meshwork is treated, but a recent studyCitation14 has shown that 90° treatment provides a similar effect. The initial energy used was 0.9 mJ. The energy was increased or decreased until bubble formation appeared and was then decreased by 0.1 mJ for the remainder of the treatment. The energy used in the present study was in the range 0.9–1.1 mJ.
All patients continued with the same medical treatment after SLT. No patient was treated with corticoids, NSAIDs, or apraclonidine before or after SLT treatment.
Inflammation was measured using a laser flare meter Kowa FM-500 (Kowa Europe, Düsseldorf, Germany). The Kowa FM-500 is based on the measurement principle of detecting scattered laser light. The unit of measurement employed by the FM-500 is photon counts per millisecond (pc/ms). A 1+ seen in the slit-lamp corresponds to a laser flare photometry value of 28.3 ± 4.8 pc/ms and a flare of 3+ to a value of 82.5 ± 5.2 pc/ms according to Guex-Crosier et al.Citation15 Herbort et alCitation16 have shown that even normal eyes express a normal flare measured to be 4 pc/ms.
Study population
Patients presenting at the Glaucoma Department at the St Erik Eye Hospital for SLT treatment who fulfilled the inclusion criteria were asked to participate in the study. Patients were enrolled consecutively between January 2009 and December 2009.
Every patient provided informed consent to participate in the study and had ample opportunity to pose questions to the study’s principal investigator. No direct rewards for participation or other incentives were given. The study was approved by the Ethical Committee at the Karolinska Institutet (approval number: 2009/1:1).
Inclusion criteria
Patients suffering from POAG or PXFG who will be treated with SLT. All patients had at least two reliable visual fields (HFA, SITA fast) showing glaucoma damage.
Gonioscopy: open angle defined as >grade II (Shaffer classification: scale 0–IV).
Exclusion criteria
Patients treated with cortisone or immunosuppressive drugs.
Patients suffering from ocular or systemic inflammatory diseases.
Patients who cannot be treated with SLT due to the eye’s characteristics (shallow anterior chamber) or bad collaboration.
Patients treated with pilocarpine (miosis makes laser flare measurements very difficult).
Statistical considerations
IOP
The IOP was measured before treatment and 2 hours, 1 week, and 1 month after SLT in both the treated and the untreated eye. For statistical purposes, the authors considered the difference in IOP between the measurements made before treatment and 1 month after SLT in the treated eyes. A comparison was then made between the POAG and the PXFG groups using a double-tailed Student’s t-test.
Laser flare measurements
The laser flare measurements were performed before SLT and 2 hours, 1 week, and 1 month after SLT. A double-tailed Student’s t-test was performed to test significance in the POAG vs PXFG comparison, with a significance level of 5%.
Sample size was estimated using STATA software (StataCorp, College Station, TX), with a power of 95%. The sample size was estimated to be 26 patients in each group.
Results
Sixty patients (60 eyes) were included in the study. When both eyes were treated, one eye was chosen at random. All participants attended their appointments. The average age was 72.6 (SD 10.38) years. The gender distribution was 32 men/28 women. Each group included 16 men and 14 women.
Regarding patient distribution, n = 30 pseudoexfoliative glaucoma, n = 30 open angle glaucoma (two patients in the PXFG group were excluded at random to make both groups equal). Regarding the number of SLT procedures undergone, n = 45 were treated with SLT for the first time; n = 8 were treated for the second time; and n = 7 were treated for the third time. All patients were treated with at least one kind of pressure-lowering eye drop ().
Table 1 Baseline characteristics of the subjects included in the study
Intraocular pressure
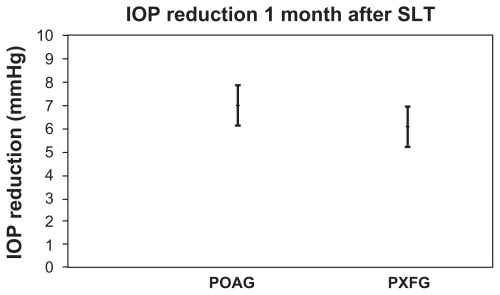
The intraocular pressure reduction 1 month after SLT was 6.87 mmHg in the POAG group and 6.19 mmHg in the PXFG group. The t-test showed no significance (P = 0.27; ).
Inflammation
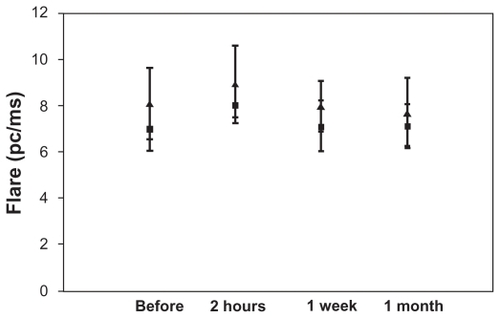
Flare in the anterior chamber was measured at the four different time intervals: before SLT and 2 hours, 1 week, and 1 month after SLT in both the POAG group and the PXFG group. No significant difference in flare was found between the two groups at any of the time intervals tested: (t-test, before: P = 0.16; 2 hours: P = 0.14; 1 week: P = 0.12; and 1 month: P = 0.36; ).
Figure 2 Flare measurements in both groups at different time intervals after SLT treatment.
Discussion
The present study showed no difference in IOP reduction and inflammation after SLT treatment when comparing POAG and PXFG. Scarce information was found regarding inflammation after SLT treatment. One of the first studies of SLT was that by Latina et al,Citation17 who evaluated inflammation using the same device as that used in this study, the Kowa laser flare meter, and found significantly lower flare readings after SLT than ALT.
The absolute average (POAG + PXFG) flare values for treated eyes in our study after SLT treatment were around 8 pc/ms. A 1+ seen in the slit-lamp corresponds to a laser flare photometry value of 28.3 ± 4.8 pc/ms according to Guex-Crosier et al.Citation15 SLT does not seem to induce clinically significant inflammation in our glaucoma patients. The study confirms previous results.Citation18
Several studies into the effects of pseudoexfoliation in ALT treatment have been published. The overall results show quite a similar IOP reduction in POAG compared to PXFG.Citation19–Citation22 Threlkeld et alCitation19 compared the effects of ALT in POAG vs PXFG and concluded that although the initial response to ALT in PXFG was greater, the long-term outcome (IOP reduction) in PXFG and POAG was similar.
With regard to the effects of SLT and pseudoexfoliation, the results of this study agree with Shazly et al,Citation11 who found a similar IOP reduction in POAG and PXFG in a long-term study published recently.
One of the limitations of our study was the rather short follow-up time. GracnerCitation10 reported no difference in IOP reduction after SLT treatment comparing POAG and PXFG (the author followed ten patients in each group over 18 months). The original purpose of the present study was to evaluate the inflammation following SLT treatment, so a longer follow-up would not provide any additional information. According to previous studies,Citation17,Citation23 inflammation decreases 1 month after SLT treatment. Furthermore, after this time, some patients from each group had their glaucoma medication discontinued or their SLT treatment repeated and this could have altered the results. Considering IOP, several studies have indicated that IOP remains stable at 6 monthsCitation17 and 18 months.Citation24 Therefore, the 1-month IOP values are likely to be predictive of future IOP control.
Another limitation could be selection bias. The St Erik Eye Hospital is a tertiary ophthalmic care institution, located in the centre of Stockholm, Sweden. The Glaucoma Department serves glaucoma patients from Stockholm County as well as from other counties. The Glaucoma Department takes care of the most complicated glaucoma cases. The POAG patients included in the study showed advanced glaucoma damage (MD: −18 dB, VFI: 45%) and were perhaps not very representative of all POAG patients. It is possible that the results would have been different if patients with less visual field damage were included.
Pseudoexfoliation and pseudoexfoliative glaucoma are common findings among patients in Northern Europe.Citation7 It was not difficult to recruit patients suffering from pseudoexfoliative glaucoma for our study, in part due to the high pseudoexfoliation prevalence in Sweden, but also due to the fact that pseudoexfoliative glaucoma usually requires additional therapy and SLT seems to be a good alternative. The energy used for SLT treatment in patients with pseudoexfoliation was the same as that used in patients without pseudoexfoliation. Pseudoexfoliation is often associated with increased pigmentation in the trabecular meshwork. In ALT treatment, it has been postulated that a greater IOP reduction in PXFG than in POAG is probably due to the greater degree of pigmentation. It is possible that the thermal effect of ALT is absorbed more at angles containing greater amounts of melanin.Citation21
In conclusion, SLT effectively and safely lowers IOP in eyes with both POAG and PXFG. Pseudoexfoliation does not seem to be a risk factor for post-laser complications.
Acknowledgments
Supported in part by grants from the Karolinska Institutet’s Foundation and the Signhild Engkvist Foundation.
Disclosure
The authors report no conflicts of interest in this work.
References
- LeskeMCHeijlAHusseinMBengtssonBHymanLKomaroffEEarly Manifest Glaucoma Trial GroupFactors for glaucoma progression and the effect of treatment: the early manifest glaucoma trialArch Ophthalmol20031211485612523884
- The Glaucoma Laser Trial Research GroupThe Glaucoma Laser Trial (GLT). Results of argon laser trabeculoplasty versus topical medicinesOphthalmology19909711140314132255512
- The Glaucoma Laser Trial Research GroupThe Glaucoma Laser Trial (GLT) and glaucoma laser trial follow-up study: 7. ResultsAm J Ophthalmol199512067187318540545
- LeeRHutnikCMProjected cost comparison of selective laser trabeculoplasty versus glaucoma medication in the Ontario Health Insurance PlanCan J Ophthalmol200641444945616883360
- LatinaMAParkCSelective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactionsExp Eye Res19956043593717789416
- KargerRAJengSMJohnsonDHHodgeDOGoodMSEstimated incidence of pseudoexfoliation syndrome and pseudoexfoliation glaucoma in Olmsted County, MinnesotaJ Glaucoma200312319319712782834
- AströmSStenlundHLindénCIncidence and prevalence of pseudoexfoliations and open-angle glaucoma in northern Sweden: II. Results after 21 years of follow-upActa Ophthalmol Scand200785883283717986292
- RingvoldAEpidemiology of glaucoma in northern EuropeEur J Ophthalmol19966126298744847
- EkströmCPrevalence of open-angle glaucoma in central Sweden. The Tierp Glaucoma SurveyActa Ophthalmol Scand19967421071128739672
- GracnerTIntraocular pressure response of capsular glaucoma and primary open-angle glaucoma to selective Nd:YAG laser trabeculoplasty: a prospective, comparative clinical trialEur J Ophthalmol200212428729212219998
- ShazlyTASmithJLatinaMALong-term safety and efficacy of selective laser trabeculoplasty as primary therapy for the treatment of pseudoexfoliation glaucoma compared with primary open-angle glaucomaClin Ophthalmol2010551021311650
- GoldenfeldMGeyerOSegevEKaplan-MessasAMelamedSSelective Laser Trabeculoplasty in Uncontrolled Pseudoexfoliation GlaucomaOphthalmic Surg Lasers Imaging20111410.3928/15428877-20110630-601.
- KanskiJClinical Ophthalmology: A Systematic ApproachLondon, UKButterworth-Heinemann Ltd1990187
- ChenEGolchinSBlomdahlSA comparison between 90 degrees and 180 degrees selective laser trabeculoplastyJ Glaucoma2004131626514704546
- Guex-CrosierYPittetNHerbortCPSensitivity of laser flare photometry to monitor inflammation in uveitis of the posterior segmentOphthalmology199510246136217724179
- HerbortCPGuex-CrosierYde AncosEPittetNUse of laser flare photometry to assess and monitor inflammation in uveitisOphthalmology199710416471 discussion 71–729022106
- LatinaMASibayanSAShinDHNoeckerRJMarcellinoGQ-switched 532-nm Nd:YAG laser trabeculoplasty (selective laser trabeculoplasty): a multicenter, pilot, clinical studyOphthalmology19981051120822088 discussion 2089–20909818610
- AyalaMLandau HögbeckIChenEInflammation assessment after selective laser trabeculoplasty (SLT) treatmentActa Ophthalmol2011894e306e30921426533
- ThrelkeldABHertzmarkESturmRTEpsteinDLAllinghamRRComparative study of the efficacy of argon laser trabeculoplasty for exfoliation and primary open-angle glaucomaJ Glaucoma1996553113168897230
- TuulonenAAiraksinenPJLaser trabeculoplasty I in simple and capsular glaucomaActa Ophthalmol (Copenh)1983616100910156659904
- HigginbothamEJRichardsonTMResponse of exfoliation glaucoma to laser trabeculoplastyBr J Ophthalmol198670118378393790485
- BergeåBIntraocular pressure reduction after argon laser trabeculoplasty in open-angle glaucoma. A two-year follow-upActa Ophthalmol (Copenh)19866444014063776504
- Martinez-de-la-CasaJGarcia-FeijooJCastilloASelective vs argon laser trabeculoplasty: hypotensive efficacy, anterior chamber inflammation, and postoperative painEye (Lond)20041849850215131681
- MelamedSBen SimonGJLevkovitch-VerbinHSelective laser trabeculoplasty as primary treatment for open-angle glaucoma: a prospective, nonrandomized pilot studyArch Ophthalmol2003121795796012860797