 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
The purpose of this study was to characterize central macular thickness and retinal volume following intravitreal injections using time domain and spectral domain optical coherence tomography (TD-OCT and SD-OCT, respectively).
Methods
Nine patients with macular edema secondary to diabetes or retinal vein occlusion treated with intravitreal triamcinolone 4.0 mg and/or bevacizumab 1.25 mg were enrolled. Central macular thickness and volume was measured by SD-OCT and TD-OCT scan at baseline, and 1, 3, 6, 24, 48 hours, and 1 week postinjection.
Results
Equations were derived to describe central macular thickness and volume reduction in the hours following intravitreal injection. Measurements of central macular thickness by SD-OCT were significantly reduced by 3 hours (P = 0.03) and retinal volume by 6 hours (P = 0.03). Central macular thickness measured 40.9 (28.6–53.2) μm thicker on the SD-OCT instrument while volume measured 3.47 (3.27–3.66) mm3 higher.
Conclusion
Significant central macular thickness and volume reductions occur in the first hours after injection with triamcinolone and/or bevacizumab.
Introduction
Diabetic retinopathy and retinal vein occlusion are the leading causes of vision loss in working aged adults due to retinal vascular abnormalities.Citation1–Citation3 Macular edema is a major common pathway for vision loss in both these diseases.Citation4 Laser photocoagulation has been the mainstay of treatment for both diabetic macular edema and macular edema secondary to branch but not central retinal vein occlusion.Citation3,Citation5–Citation7 However, recent studies have shown that intravitreal delivery of corticosteroids and antivascular endothelial growth factor (VEGF) agents can provide significant visual benefits for branch and central retinal vein occlusion.Citation8–Citation12
The corticosteroid most often used for intravitreal injections is triamcinolone because of its long therapeutic response of up to 3 months.Citation13 Ranibizumab (rhuFab V2, Lucentis®, Genentech, South San Francisco, CA) is the affinity-matured anti-VEGF antibody recently approved for retinal vein occlusion.Citation11,Citation12 The full-length antibody, bevacizumab (Avastin®, Genentech, South San Francisco, CA), is commonly used off-label.Citation14 These agents are effective in improving visual acuity and reducing macular edema associated with diabetic retinopathy and retinal vein occlusion in prospective randomized trials.Citation15–Citation23 However, a durable effect is often not achieved, with macular edema recurring after several months, and retreatment is required.Citation18,Citation24 When both triamcinolone and bevacizumab were used in a combined injection, visual improvement was faster but the added benefit disappeared in longer follow-up.Citation25 Compared with laser photocoagulation, intravitreal injections may be more effective in the months after intervention, but laser may offer better visual outcomes in the following years.Citation26,Citation27 A recent trial suggests that a combined therapeutic approach using intravitreal ranibizumab or triamcinolone injections for their short-term effects and laser for long-term control may be optimal.Citation28 However, the most cost-effective and convenient approach from both the patient and physician perspective remains unclear.
A better understanding of the immediate effects of these drugs would provide insight into their mechanisms of action and could lead to the development of more targeted and effective treatments. Additionally, it may help clarify the role of each type of therapeutic intervention, elucidating the optimal dosing regimens for patients. This pilot study used spectral domain optical coherence tomography (SD-OCT) to characterize short-term changes in macular thickness in the first hours and days following a single intravitreal injection of one or both of these agents, and investigated potential measurement differences between two widely used OCT methods, ie, SD-OCT and time domain OCT (TD-OCT).
Materials and methods
The research protocol for this observational study was approved by the Stanford University School of Medicine Institutional Review Board. A total of 45 patients with macular edema secondary to either diabetic retinopathy or retinal vein occlusion were identified by computerized review of patient records and were asked to participate in the study between November and December 2008. Patients who were pregnant were excluded from the study, as were children. An initial power calculation using a power of 80% and significance level of 0.05 indicated that approximately 10 patients were needed to determine a central macular thickness difference of 90 μm with a standard deviation of 100 μm, as had been shown in previous studies.Citation25,Citation29 A total of nine patients were able to be enrolled during the study period, of which six were treated with intravitreal triamcinolone 4.0 mg alone (including five with diabetic macular edema). Of the four patients with retinal vein occlusion, one had branch vein occlusion and three had central vein occlusion. The patient with branch retinal vein occlusion received bevacizumab 1.25 mg. For the three patients with central retinal vein occlusion, one received triamcinolone 4.0 mg, one received bevacizumab 1.25 mg, and one received both agents simultaneously. The clinical judgment of the treating physician determined the type of injection given to the patients; all had previously received some sort of intravitreal injection. A summary of each patient’s disease process and injection received can be found in .
Table 1 Summary of disease process, injection, visual acuity, and calculated coefficient for exponential decline in macular edema in enrolled patients 48 hours after treatment
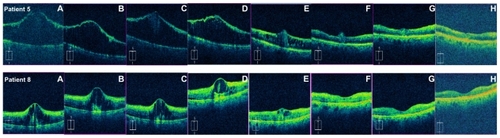
Imaging was performed using TD-OCT (Stratus OCT Software Version 5.0 Carl Zeiss Meditec, Dublin, CA) and SD-OCT (Cirrus HD-OCT Software Version 3.0; Carl Zeiss Meditec) prior to injection and then at 1 hour, 3 hours, 6–9 hours, 1 day, 2 days, and 1 week after injection. A six-line fast macular scanning protocol was used for the TD-OCT device and a 512 × 128 macular cube protocol was used for the SD-OCT device. Snellen visual acuity with pinhole was recorded before each scan. Additional SD-OCT scans were obtained from seven patients at their final visit 4–6 weeks later. shows an example of the SD-OCT images collected for patients 5 and 8. After the first patient, the following four patients with diabetic retinopathy had imaging performed on both eyes so that the fellow (noninjected) eye could serve as a control for any fluctuations in levels of macular edema.
Figure 1 Representative spectral domain optical coherence tomography scans from two patients showing the macula at (A) prior to intravitreal injection, (B) 1 hour, (C) 3 hours, (D) 6–9 hours, (E) 24 hours, (F) 48 hours, (G) 1 week, and (H) 1 month following injection. Patient 5 (top) received an injection of triamcinolone 4.0 mg while patient 8 (bottom) received bevacizumab 1.25 mg.
Software-generated measurements for central subfield mean thickness were recorded as central macular thickness. Central macular thickness and macular volume measurements at each time point were plotted and fitted to both an exponential and linear regression model to determine the rate of reduction in the first 24 and 48 hours after injection. Results for each individual patient were then averaged to generate a mean and confidence interval for the measurement. Individual scans on the SD-OCT instrument were reviewed and any abnormalities in the segmentation software that would have resulted in incorrect calculations of central macular thickness and macular volume were manually corrected using the analysis software for two of the 91 scans collected in this study. Lines from the TD-OCT scans with gross errors in automated segmentation were discarded, because the review software did not have an editing feature. Paired t-tests were used to determine the time at which the reduction in central macular thickness and macular volume became significant. Data were analyzed for each injection type and disease process separately, and also for all nine patients together using the Analyse-It software program (Analyse-It Software, Leeds, UK). Both percent and absolute changes are reported because it has been shown that absolute changes in thickness are the preferred measure in mild thickening, and relative change is preferred in more severe thickening.Citation30 The mean difference in central macular thickness and volume measurements from both instruments were compared to determine if a systematic difference in measurement existed for patients with macular edema.
Results
The mean age of the patients in this study was 70.6 (55–82) years; six were female and three were male. summarizes the disease, injection type, and visual acuity for each patient, as well as the extent to which they could be fit to a regression model. Baseline visual acuity was correlated with central macular thickness, with a linear coefficient of 0.68. When central macular thickness was tracked over time, correlation coefficients were uniformly higher for exponential than for linear regressions, and only the exponential coefficients are displayed. All patients except patient 1 displayed some improvement in visual acuity in the first week after their intravitreal injection. All patients except for patient 2 showed a negative correlation coefficient, indicating an exponential reduction in central macular thickness during the first 48 hours following an injection. Patient 2 (regression coefficient 0.002 per hour) also had the lowest correlation coefficient (R2 = 0.03). Five patients had correlation coefficients greater than 0.9 (patient 1 and patients 5–8), and of these, two were perfectly described by an exponential function (patients 5 and 8). One of the remaining patients had a correlation coefficient less than 0.5 (patient 9), while the coefficient for the other two was approximately 0.7 (patients 3 and 4). The aggregate data for all patients by injection and by disease process medication is shown in . When separated into subgroups, the confidence intervals for the coefficient of reduction in central macular thickness include 0. However, when the patients are analyzed together, the exponential coefficient of reduction was −0.010 (−0.018 to −0.002) per hour (R2 = 0.83). is a graphical representation of the central macular thickness for each patient in the first 48 hours after their injection.
Figure 2 Reduction in central macular thickness in the first 48 hours after injection.
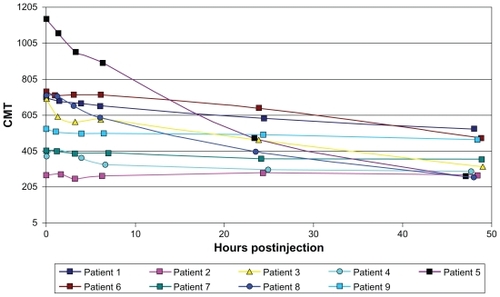
Table 2 Exponential regression coefficients for the first 48 hours after injection shown for all patients combined and also divided by treatment and by disease process
Volume measurements were more poorly described by both exponential and linear regression models, although again the exponential regression produced higher correlation coefficients. Four patients had correlation coefficients less than 0.5. Three patients had correlation coefficients between 0.7 and 0.9 (patients 3, 6, and 8) and two patients had correlation coefficients greater than 0.9 (patients 1 and 5). Again, the confidence interval included 0 when patients were separated by injection type and disease process, but when all the data were combined, the average exponential coefficient of reduction was −0.005 (−0.009 to −0.0002) per hour (R2 = 0.34).
displays the mean reduction in central macular thickness in the hours to days after intravitreal injections measured by both the TD-OCT and SD-OCT devices. A statistically significant reduction was found by the SD-OCT instrument starting at 3 hours after injection (P = 0.027) and persisted throughout the following period. By 48 hours, the mean reduction in central macular thickness was 260.44 (46.41–474.47) μm (33.51%). This accounted for 80% of the eventual reduction achieved in a week, ie, 310.33 (88.56–532.11) μm (41.17%). However, on the TD-OCT instrument, a significant reduction was not seen until 24 hours (P = 0.035) or longer after injection. At 48 hours after injection, the mean reduction was 259.78 (72.75– 446.81) μm (37.92%) or 90% of the reduction achieved at 1 week. When the data were separated by injection types, the statistical significance disappeared for scans taken from both machines as the group sizes were not powered to detect a difference. Additionally, when the data were separated by disease process as shown in , there was a significant difference in central macular thickness starting at 3 hours for patients with diabetic retinopathy and 6 hours for those with retinal vein occlusion (P = 0.003, P = 0.048, respectively). However, this difference between the groups was no longer significant after 24 hours, although the mean difference continued to grow larger. No significant trends were observed in the four diabetic patients whose fellow eyes with macular edema were also scanned as a control for variations in macular edema as the natural progression or fluctuation of the disease.
Table 3 Pooled data for mean reduction (n = 9) in central macular thickness compared with baseline measurements made before injection on both SD-OCT and TD-OCT instruments
Table 4 Data for mean reduction in central macular thickness compared with baseline measurements before injection in patients with diabetic retinopathy or retinal vein occlusion
Reductions in macular volume were also evaluated and showed similar trends. The reduction in volume seen on SD-OCT scans reached statistical significance at 6 hours (P = 0.031), while the mean difference was 0.89 (0.11–1.67) mm3 (5.42%). At 48 hours, volume reduction was 3.20 (0.27–6.13) mm3 (17.90%). This was over 80% of the reduction in volume reached in 1 week, 3.88 (0.85–6.91) mm3 (22.21%). The TD-OCT instrument did not show a significant change until 24 hours after the injection (P = 0.041). Similar to the SD-OCT scans, at 48 hours after injection, volume was reduced by 3.39 (0.74–6.04) mm3 (25.08%). This was over 80% of the reduction in volume achieved in a week, ie, 3.10 (0.10–6.09) mm3 (21.80%). When analyzed separately by type of injection and by disease, none of the reductions in macular volume were statistically significant.
Compared with the CMT measurements made by the TD-OCT instrument, SD-OCT measurements were on average 40.9 (28.6–53.2) μm thicker (n = 84, all scans). The SD-OCT instrument also calculated a greater volume, on average 3.47 (3.27–3.66) mm3 higher than TD-OCT data.
Discussion
The results reported here indicate that the reduction in central macular thickness occurs rapidly in the first few hours after intravitreal drug injection and generally follows an exponential rather than linear decay. This suggests that the drugs may immediately change the permeability of the retinal pigment epithelium to fluid movement or can recruit pumps to expel accumulated proteins and fluid actively. The rate of reduction in central macular thickness is best described by the following exponential function:
Volume measurement data were less consistent, but can be described by the equation:
Prior studies by Marmor have determined 0.1 μL/hour/mm2 to be the rate at which the retinal pigment epithelium is capable of pumping out fluid, or an expected reduction of 0.1 mm3/hour in the 1 mm2 space of measurement for central macular thickness.Citation31 Even higher flow rates are achievable when the retina is damaged, like in retinal detachments, and passive transport is the predominant force driving fluid movement.Citation31 Our study found a linear rate of reduction of −0.066 mm3/hour or an exponential coefficient −0.0005 per hour, a very similar rate to the one reported previously. This suggests that intravitreal triamcinolone and bevacizumab injections may be enhancing some mechanism of active transport to cause efflux of macular edema fluid. Blood retinal junctions in this case are likely intact and passive forces do not come into play.
The focus of previous pharmacokinetic studies has been the period of time in which an agent remains in the vitreous. Studies of high-dose triamcinolone injections (20–25 mg) showed that the steroid is still detectable in eyes without prior vitrectomy even a year and a half after the injection, and for 3 or more months afterwards in eyes that had undergone vitrectomy.Citation24,Citation32,Citation33 Bevacizumab 1.5 mg has been shown to have an aqueous half-life of 9.8 days.Citation34 Given the different rates of clearance of these agents, it seems worthwhile to compare the rates at which they act in the initial period. It has been hypothesized that corticosteroids may act by inhibiting the VEGF gene or by modulating the effector proteins related to the VEGF signaling pathway.Citation13 A similar drug effect time would be evidence in support of the two agents affecting a common pathway. The results in this study suggest that this is possibly the case; the rates of reduction in macular edema are likely to be comparable between patients receiving intravitreal triamcinolone and bevacizumab.
This study also reveals that significant reductions in both central macular thickness and macular volume occur as early as the first 6 hours after an intravitreal injection. While study enrollment was insufficiently powered to detect differences in patients receiving triamcinolone 4.0 mg alone or bevacizumab 1.25 mg alone, the pooled data strongly suggest that a robust change occurred rapidly in the injected eyes. When the data were separated by disease process, an initially significant change at 3 and 6 hours occurred, but because of the lack of power and increase in variance, the calculations after 24 hours were no longer significant, even though the mean difference grew larger. After 1 week, patients on average saw a reduction of 41% in their central macular thickness, with over half of this change occurring in the first day and 80% of the change by 48 hours. Further, patients generally had an improvement in Snellen visual acuity measured at these visits. Only patient 1 experienced no change in visual acuity, despite having a dramatic reduction in her central macular thickness from 706 μm to 459 μm. However, she had long-standing, poorly controlled disease previously treated with vitrectomy and extensive peripheral ischemia on fluorescein angiography, severely limiting her visual potential. Previous studies have shown that patients with ischemic central retinal vein occlusion do not respond to triamcinolone injections, while those with nonischemic central retinal vein occlusion do respond.Citation18 It may be that the degree of ischemic damage already incurred in the retina is the limiting factor for response. Only patient 2 experienced no reduction in central macular thickness, although he did have an improvement in visual acuity. He did not have extensive areas of ischemia by fluorescein angiography. He did start with a relatively more normal central macular thickness measurement (271 μm) which left relatively little headroom for a statistically significant decrease in central macular thickness compared with the other eight patients, all of whom had considerably larger starting values for central macular thickness. Studies have also shown that the link between visual acuity and macular thickness may be tenuous, with only a modest correlation between best corrected visual acuity and macular thickness.Citation35,Citation36
It is also interesting to note that patient 2 had a correlation coefficient of 0.03 when fit to an exponential curve and patient 9 had a correlation of 0.43. This suggests that there may be infrequent nonresponders to triamcinolone 4.0 mg injections. Because there were only two patients who received bevacizumab 1.25 mg injections, it is difficult to determine whether this phenomenon is also true for that drug, although there is anecdotal evidence for this phenomenon in some diabetic patients, at least for single injections. This effect will be important to understand in order to optimize treatment schedules for patients and eliminate injections that do not benefit patients. The results of this study indicate that responders to treatment would likely show a change within hours of the injection. Future studies can evaluate if a strategy of remeasuring central macular thickness within 24–48 hours and choosing an alternative agent in nonresponders would lead to better resolution of macular edema and improved visual outcomes. A study with longer follow-up would also be helpful to evaluate whether the initial response is predictive of long-term sustainability of the reduction in macular edema.
Previous studies and meta-analyses have determined that patients often see an improvement in the months following an injection, and many need repeated injections for a sustained effect.Citation20,Citation37 A 2007 DRCRnet study showed that patients receiving bevacizumab 1.25 mg and 2.25 mg injections had greater reductions in central macular thickness than those who received laser treatment. These patients also had better improvements in visual acuity at 12 weeks with no short-term benefits of combining laser and bevacizumab injections.Citation38 Laser photocoagulation was also shown to be less effective than triamcinolone 4.0 mg injections in the short term, but the effect was no longer present at 1 year and even reversed later, with patients receiving laser having better visual outcomes after 2 years.Citation26,Citation27 Based on those results and the preliminary results generated from this study, similar mechanisms may be activated by both injection types.
It is possible that the effects of triamcinolone are more short-term than those of bevacizumab, but this is yet to be shown in a prospective comparison. Overall, it appears that intravitreal injections of anti-VEGF agents and corticosteroids could be used for their short-term effects (days and weeks) to reduce macular edema to a level at which laser photocoagulation can be considered to achieve long-term control (years and more). A recent DRCRnet study was performed to evaluate the efficacy of such a combination approach, using intravitreal triamcinolone or ranibizumab injections for their short-term effects and laser for long-term control. Participants were randomized to sham injection and prompt laser, ranibizumab 0.5 mg and prompt laser, ranibizumab 0.5 mg and delayed laser, or triamcinolone 4.0 mg and prompt laser. Patients who received drug injections and laser treatments had more reduction in central macular thickness than those who received sham injections and laser after one and 2 years.Citation28
Since the initiation of this study, more work has been done to understand the measurement differences between the Stratus and the Cirrus OCT systems. Kiernan et al found that in conditions of increased macular thickness, the thickness measured by the Cirrus is 43 μm greater than the Stratus, likely due to measurement differences built into the detection algorithms of the machines.Citation39 Our study showed a similar increase in thickness of 40.9 μm and a volume of 3.47 (3.27–3.66) μm3 higher.
The conclusions able to be drawn from this study are limited by the small sample size. While 45 patients were approached to participate, only nine were enrolled because of the time commitment on the day of injection and for follow-up visits. However difficult the recruitment, it would be valuable to pursue future investigations involving more patients receiving each type of injection and underlying disease processes. An effective treatment strategy could be determined more rapidly because it appears that patients who are destined to respond to treatment are likely to declare themselves within the first 24 hours after receiving an intravitreal injection of triamcinolone or bevacizumab. Additionally, further studies could lead to new insights into the mechanism of action of different therapies for macular edema, paving the way for the development of more targeted therapeutics.
Acknowledgment
This research was partially supported by an equipment loan from Carl Zeiss Meditech Inc, Dublin, CA.
Disclosure
This study was presented in part at the meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, FL, May 2–6, 2010. None of the authors have any proprietary interest in any of the products used in this study.
References
- RogersSMcIntoshRLCheungNThe prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and AustraliaOphthalmology2010117231331920022117
- Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study GroupAm J Ophthalmol19849832712826383055
- McIntoshRLMohamedQSawSMWongTYInterventions for branch retinal vein occlusion: an evidence-based systematic reviewOphthalmology2007114583585417397923
- Wilkinson-BerkaJLMillerAGUpdate on the treatment of diabetic retinopathyScientific World Journal200889812018264628
- SchachatAPA new approach to the management of diabetic macular edemaOphthalmology201011761059106020522333
- MohamedQMcIntoshRLSawSMWongTYInterventions for central retinal vein occlusion: an evidence-based systematic reviewOphthalmology2007114350751917324695
- KariaNRetinal vein occlusion: pathophysiology and treatment optionsClin Ophthalmol2010480981620689798
- HallerJABandelloFBelfortRJrRandomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusionOphthalmology201011761134114620417567
- IpMSScottIUVan VeldhuisenPCA randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 5Arch Ophthalmol200912791101111419752419
- ScottIUIpMSVan VeldhuisenPCA randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6Arch Ophthalmol200912791115112819752420
- BrownDMCampochiaroPASinghRPRanibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III studyOphthalmology201011761124113320381871
- CampochiaroPAHeierJSFeinerLRanibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III studyOphthalmology201011761102111220398941
- SivaprasadSMcCluskeyPLightmanSIntravitreal steroids in the management of macular oedemaActa Ophthalmol Scand200684672273317083528
- PieramiciDJRabenaMDAnti-VEGF therapy: comparison of current and future agentsEye (Lond)200822101330133618497829
- IpMKahanaAAltaweelMTreatment of central retinal vein occlusion with triamcinolone acetonide: an optical coherence tomography studySemin Ophthalmol2003182677314566625
- ParkCHJaffeGJFekratSIntravitreal triamcinolone acetonide in eyes with cystoid macular edema associated with central retinal vein occlusionAm J Ophthalmol2003136341942512967793
- BashshurZFMalufRNAllamSJurdiFAHaddadRSNoureddinBNIntravitreal triamcinolone for the management of macular edema due to nonischemic central retinal vein occlusionArch Ophthalmol200412281137114015302653
- IpMSGottliebJLKahanaAIntravitreal triamcinolone for the treatment of macular edema associated with central retinal vein occlusionArch Ophthalmol200412281131113615302652
- AstamNBatiogluFOzmertEShort-term efficacy of intravitreal bevacizumab for the treatment of macular edema due to diabetic retinopathy and retinal vein occlusionInt Ophthalmol200929534334818553061
- GroverDLiTJChongCCIntravitreal steroids for macular edema in diabetesCochrane Database Syst Rev20081CD00565618254088
- GunduzKBakriSJIntravitreal bevacizumab for macular oedema secondary to branch retinal vein occlusionEye (Lond)20082291168117118344969
- HauserDBukelmanAPokroyRIntravitreal triamcinolone for diabetic macular edema: comparison of 1, 2, and 4 mgRetina200828682583018536598
- YilmazTWeaverCDGallagherMJIntravitreal triamcinolone acetonide injection for treatment of refractory diabetic macular edema: a systematic reviewOphthalmology2009116590291119410949
- JermakCMDellacroceJTHeffezJPeymanGATriamcinolone acetonide in ocular therapeuticsSurv Ophthalmol200752550352217719372
- AhmadiehHRamezaniAShoeibiNIntravitreal bevacizumab with or without triamcinolone for refractory diabetic macular edema; a placebo-controlled, randomized clinical trialGraefes Arch Clin Exp Ophthalmol2008246448348917917738
- Diabetic Retinopathy Clinical Research NetworkA randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edemaOphthalmology200811591447144918662829
- BeckRWEdwardsARAielloLPThree-year follow-up of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular edemaArch Ophthalmol2009127324525119273785
- ElmanMJAielloLPBeckRWRandomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edemaOphthalmology201011761064107720427088
- SoheilianMRamezaniABijanzadehBIntravitreal bevacizumab (Avastin) injection alone or combined with triamcinolone versus macular photocoagulation as primary treatment of diabetic macular edemaRetina20072791187119518046223
- BrowningDJGlassmanARAielloLPOptical coherence tomography measurements and analysis methods in optical coherence tomography studies of diabetic macular edemaOphthalmology200811581366137118675696
- MarmorMFMarmorMFWolfensbergerTJControl of subretinal fluid and mechanisms of serous detachmentThe Retinal Pigment Epithelium: Function and DiseaseNew York, NYOxford University Press1998
- KosobuckiBRFreemanWRChengLPhotographic estimation of the duration of high dose intravitreal triamcinolone in the vitrectomised eyeBr J Ophthalmol200690670570816531422
- JonasJBIntraocular availability of triamcinolone acetonide after intravitreal injectionAm J Ophthalmol2004137356056215013884
- KrohneTUEterNHolzFGMeyerCHIntraocular pharmacokinetics of bevacizumab after a single intravitreal injection in humansAm J Ophthalmol2008146450851218635152
- BrowningDJGlassmanARAielloLPRelationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edemaOphthalmology2007114352553617123615
- BlumenkranzMSHallerJAKuppermannBDCorrelation of visual acuity and macular thickness measured by optical coherence tomography in patients with persistent macular edemaRetina20103071090109420616686
- KhuranaRNDoDVNguyenQDAnti-VEGF therapeutic approaches for diabetic macular edemaInt Ophthalmol Clin200949210911919349791
- ScottIUEdwardsARBeckRWA phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edemaOphthalmology2007114101860186717698196
- KiernanDFHariprasadSMChinEKKiernanCLRagoJMielerWFProspective comparison of cirrus and stratus optical coherence tomography for quantifying retinal thicknessAm J Ophthalmol2009147226727518929353