Abstract
Cytomegalovirus (CMV) retinitis remains the most common opportunistic ocular infection in immunocompromised patients. Patients with immunocompromising diseases, such as acquired immunodeficiency syndrome, inherited immunodeficiency states, malignancies, and those on systemic immunosuppressive therapy, are known to be at risk. Recently, it has been suggested that patients undergoing intravitreal injection of immunosuppressive agents may also be predisposed. One previous case report speculated that there may be an additional risk for CMV retinitis in acquired immunodeficiency syndrome patients with venoocclusive disease. This case study presents a case of CMV retinitis following central retinal vein occlusion in a patient on systemic immunosuppressants.
Case presentation
An 82-year-old Caucasian male presented to a community ophthalmologist with 6 months of decreased vision in the left eye. Initial workup revealed abnormal fundus findings and the patient was referred to a local retina specialist who diagnosed nonischemic central retinal vein occlusion (CRVO) of the left eye, demonstrated by fluorescein angiography. At that time, visual acuity in the affected eye was 20/30. Several weeks later, the patient was seen in follow-up and, on fundus exam of the affected eye, was noted to have new, apparently unrelated changes. He was subsequently referred to the Havener Eye Institute in July 2011 for further evaluation, with concern for a viral retinitis.
The patient’s past medical history was significant, as he had had a kidney transplant in 2007 following advanced diabetic nephropathy. His immunosuppressive regimen at the time of presentation consisted of tacrolimus 5 mg twice daily, mycophenolate mofetil 750 mg twice daily, and prednisone 5 mg daily. His cytomegalovirus (CMV) status at the time of transplant was donor and recipient positive, and he had no history of systemic CMV infection. Prior to the clinic’s evaluation, his most recent laboratory tests revealed a normal white blood cell count and a normal tacrolimus level.
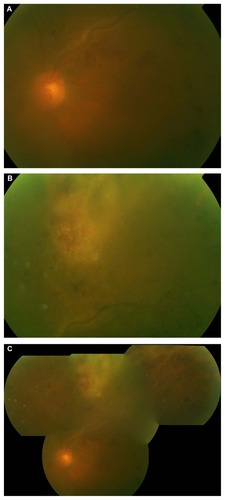
Examination revealed 20/40 vision in the left eye with no afferent papillary defect and normal intraocular pressure. There was 3+ nuclear sclerotic cataract and mild vitritis. Fundus examination showed a normal optic disc with scattered intraretinal hemorrhage in the macula, tortuousity, and sheathing of the superior arcades and, in the superior periphery, a 5-disc diameter area of granular whitening with intralesional hemorrhage consistent with CMV retinitis ().
Figure 1 Color fundus photos showing: (a) Dilation, tortuousity, and sheathing along the superior venous arcade, with scattered flame-shaped and intraretinal hemorrhages; (b) 5 disc diameter white, granular-appearing lesion with intralesional hemorrhage in the superior periphery; (c) Composite image of the same eye.
The patient was started on valganciclovir 900 mg twice daily for 2 weeks, which was then decreased to 450 mg daily. At one month, the left eye vision improved to 20/25, with regression of the retinal lesion.
Discussion
The hematogenous dissemination of CMV is carried out by polymorphonuclear leukocytes and monocytes.Citation1 Endocytosis of infected leukocytes by retinal vascular endothelial cells, with subsequent intracellular replication, endothelial cell damage, and ultimate compromise of the blood-retina barrier is thought to be the primary pathogenic mechanism by which CMV invades the neuroretina.Citation2 However, some autopsy studies of acquired immunodeficiency syndrome (AIDS)- infected patients with CMV retinitis have failed to demonstrate CMV infection within the retinal vascular endothelial cells, suggesting the possibility of an alternative pathogenic pathway in some patients.Citation3,Citation4
It has been suggested that the vascular breaches and leakage from microaneurysms frequently seen in patients with AIDS may facilitate the passage of infected leukocytes through the blood retinal barrier, without infection of endothelial cells.Citation5,Citation6 Mansour et al reported a case of hemiretinal vein occlusion in a patient with AIDS who subsequently developed CMV retinitis in the same neuroretinal distribution.Citation7 The authors speculated that the facilitated passage of infected leukocytes across the blood-retinal barrier in AIDS patients might be further enhanced by the venous stasis and ischemic endothelial damage caused by venoocclusive disease.Citation7
A review of the literature yielded two other cases of venoocclusive events followed by CMV retinitis – both in locally immunocompromised patients. Park and Byeon reported a 77-year-old woman without any known immunocompromising disease state and who was not taking systemic immunosuppressive medications, who was diagnosed with CMV retinitis four months after intravitreal triamcinalone injection for CRVO-related macular edema.Citation8 Similarly, Vertes et al reported an immunocompetent 78-year-old woman who underwent intravitreal triamcinalone injection for a branch retinal vein occlusion, then 3 months later, presented with CMV retinitis in the same hemispheric distribution.Citation9 These reports emphasized the potential of local intravitreal immunosuppression to predispose to CMV retinitis – an occurrence which has been reported elsewhere.Citation8–Citation13 Neither mentioned CRVO-related vasculopathy as a possible contributing factor.
The association of CMV retinitis with systemic immunosuppression following solid organ transplantation is well documented.Citation14–Citation16 This study’s patient was on systemic immunosuppresants for 4 years without complication, then, within 2 months of developing CRVO, developed CMV retinitis in the same eye. While these events could have occurred independently and their sequence may have been coincidental, the authors suggest that the events may support the assertion made by Mansour et al,Citation7 that secondary venous stasis and endothelial damage after venooculsive events may facilitate the development of CMV retinitis in patients already at risk.
Disclosure
The authors report no conflicts of interest in this work.
References
- GernaGBaldantiFRevelloMPathogenesis of human cytomegalovirus infection and cellular targetsHum Immunol200465538138615172435
- BodaghiBSlobbe-van DrunenMEntry of human cytomegalovirus into retinal pigment epithelial and endothelial cells by endocytosisInvest Ophthalmol Vis Sci199940112598260710509655
- HollandGPeposeJPettitTGottliebMYeeRFoosRAcquired immune deficiency syndrome. Ocular manifestationsOphthalmology19839088598736314219
- PeposeJHollandGNestorMCochranAFoosRAcquired immune deficiency syndrome. Pathogenic mechanisms of ocular diseaseOphthalmology19859244724842987769
- GlasgowBJWeisbergerAA quantitative and cartographic study of retinal microvasculopathy in acquired immunodeficiency syndromeAm J Ophthalmol1994118146568023875
- GlasgowBEvidence for breaches of the retinal vasculature in acquired immune deficiency syndrome angiopathy. A fluorescent microsphere studyOphthalmology199710457537609160019
- MansourALiHSegalEPicture resembling hemicentral retinal vein occlusion in the acquired immunodeficiency syndrome: is it related to cytomegalovirus?Ophthalmologica199621021081119148255
- ParkYByeonSCytomegalovirus retinitis after intravitreous triamcinolone injection in a patient with central retinal vein occlusionKorean J Ophthalmol20082221434
- VertesDSnyersBDe PotterPCytomegalovirus retinitis after low-dose intravitreous triamcinolone acetonide in an immunocompetent patient: a warning for the widespread use of intravitreous corticosteroidsInt Ophthalmol201030559559720931263
- SaidelMBerreenJMargolisTCytomegalovirus retinitis after intravitreous triamcinolone in an immunocompetent patientAm J Ophthalmol200514061141114316376669
- Ufret-VincentyRSinghRLowderCKaiserPCytomegalovirus retinitis after fluocinolone acetonide (Retisert) implantAm J Ophthalmol2007143233433517258523
- DelyferMRougierMHubschmanJAouizérateFKorobelnikJCytomegalovirus retinitis following intravitreal injection of triamcinolone: report of two casesActa Ophthalmol Scand200785668168317403022
- SekiryuTIidaTKanekoHSaitoMCytomegalovirus retinitis after intravitreal triamcinolone acetonide in an immunocompetent patientJpn J Ophthalmol200852541441618991048
- WiegandTYoungLCytomegalovirus retinitisInt Ophthalmol Clin20064629111016770157
- PollardREgbertPGallagherJMeriganTCytomegalovirus retinitis in immunosuppressed hosts. I. Natural history and effects of treatment with adenine arabinosideAnn Intern Med19809356556646259979
- EgbertPPollardRGallagherJMeriganTCytomegalovirus retinitis in immunosuppressed hosts. II. Ocular manifestationsAnn Intern Med19809356646706259980