Abstract
Purpose
To examine changing patterns of ophthalmic presentations to emergency departments (EDs) during the lockdowns associated with the first wave of the COVID-19 pandemic in Australia and the two months immediately following lockdown relaxation.
Patients and Methods
This was a retrospective audit of triage coding and ICD-10-AM coding for all patient presentations to four Australian EDs from March 29 to May 31 in 2019 and 2020 (the COVID-19 lockdown period and the corresponding period in 2019), and from June 1 to July 31 in 2019 and 2020 (the post-lockdown period and the corresponding period in 2019). Number of ophthalmic presentations triaged per day and number of seven common and/or time-sensitive, vision threatening ophthalmic diagnoses were examined. Differences in mean daily presentation numbers were assessed with non-paired Student’s t-test with Bonferroni correction.
Results
Total ophthalmic presentations per day during COVID-19 lockdowns fell by 16% compared to the corresponding period in 2019 (13.0 ± 4.0 in 2019 vs 10.8 ± 3.3 in 2020, mean ± standard deviation; p=0.01). There was also a significant decrease in presentations of atraumatic retinal detachment, conjunctivitis, and eye pain. In the two months following easing of lockdown restrictions, total ophthalmic presentations per day returned to the same level as that of the corresponding period in 2019 (12.2 ± 4.3 in 2019 vs 12.3 ± 4.1 in 2020, p=0.97).
Conclusion
Total ophthalmic presentations and presentations of atraumatic retinal detachment, conjunctivitis and, eye pain to EDs fell during the lockdowns associated with the first wave of COVID-19 in Australia. These may represent delays in patients seeking appropriate medical attention and may have implications on patient morbidity long after the COVID-19 pandemic.
Introduction
In the face of the COVID-19 pandemic, many countries have taken extraordinary measures to prevent the spread of disease and ensure safety of the general population. In many cases, these measures have included lockdowns, with forced closures of businesses, schools and other public venues, and restrictions on movement and gathering of people. In the state of New South Wales (NSW) in Australia, legislation in the form of Public Health Orders was introduced between March 18 and 26, 2020 requiring: closure of many businesses including bars, clubs, restaurants, cinemas, places of worship, gyms etc; prohibition of nonessential gatherings of more than 100 people and prohibition of gatherings with less than four square meters of space per person.Citation1,Citation2 On March 29, 2020, further Public Health Orders were introduced limiting people leaving home other than for work, study, shopping, access to medical care or exercise.Citation1,Citation2 In addition to legislation, Australian Government public health messaging encouraged high risk groups including people over the age of 70 years, those with chronic medical conditions and, Aboriginal and Torres Strait Islander peoples to specifically stay at home where possible.Citation3 In NSW, lockdown measures were somewhat relaxed on June 1, 2020 with reopening of businesses including pubs, clubs, cafes, restaurants, and museums, lifting of restrictions on the general population for leaving home or intrastate travel (eg the population was allowed to travel to regional areas for holidays etc).Citation4
In preparation for surges of COVID-19 patients, emergency departments (EDs) in many countries increased their patient capacities. Despite increased capacities, many EDs have reported changing patterns of presentations of non-COVID-19 pathologies.Citation5,Citation6 While reductions in some acute presentations have been seen (eg infectious diseases), decreases in certain high acuity presentations such as acute coronary syndrome (ACS) and stroke have also been reported.Citation5–Citation7 A retrospective analysis from Italy of 547 patients revealed a significant reduction in patients admitted with ACS during February and March 2020 (13.3 per day) when compared to the same time period in 2019 (18.9 per day).Citation5 Another example is that of Guglielmo da Saliceto Hospital in northern Italy where stroke presentations in February and March 2020 averaged approximately six cases a month compared to an average of 51 presentations per month over the same period in 2019.Citation6
Similar patterns, if observed for time-sensitive, vision threatening ophthalmic presentations, will be important for guiding public health messaging on timely presentation for emergency treatment, and for informing requirements for and importance of providing continuity of ophthalmic care in the current and future pandemics. Understanding how presentation patterns change in the post-lockdown period, particularly how quickly presentation patterns return to normal and whether any surges in non-COVID pathologies occur, will also be important for public health policy planning.
The aims of this study were to examine changing patterns of presentations of ophthalmic presentations to EDs during the lockdowns associated with first wave of the COVID-19 pandemic in the Australian context, and the changing patterns of ophthalmic presentations to EDs as these lockdowns were lifted.
Patients and Methods
NSW is the most populous state in Australia with almost a third of the nation’s population (8,129,000 of 25,522,200 people as of December 2019).Citation8 Within NSW is the Western Sydney Local Health District, a publicly funded metropolitan health network with a 1925-inpatient capacity over four hospitals (each with EDs) serving a catchment population of over 950,000 people. It is NSW’s second largest health network by catchment population and is forecast to become the largest by 2021.Citation9 Within the Western Sydney Local Health District and Westmead Hospital is the Westmead Eye Clinic, a quaternary referral ophthalmology unit that serves a broader catchment population of 3,000,000 people, providing over 30,000 patient consultations per year.
To explore changing patterns of presentations of emergent ophthalmic presentations to the district’s EDs and by extension the Westmead Eye Clinic during Australia’s first wave of the COVID-19 pandemic, we retrospectively audited triage coding using the NSW Ministry of Health ED Presenting Problem Code Set (EDPPCS), a code set based on SNOMED CT terminology,Citation10,Citation11 International Classification of Diseases, tenth revision, Australian modification (ICD-10-AM) final diagnosis coding, and separations data for ED presentations to the four hospitals within the Western Sydney Local Health District. Data from March 29 to May 31 in 2019 and 2020 (the COVID-19 lockdown period and corresponding period of the previous year), and from June 1 to July 31, 2019 and 2020 (the post-lockdown period and corresponding period of the previous year) was audited. All patients seen during the period were included in the audit, with no exclusions.
The number of ophthalmic presentations triaged per day (EDPPCS specifying an eye complaint) and number of seven common and/or time-sensitive, vision threatening ophthalmic diagnoses (ICD-10-AM diagnosis) were further examined. These diagnoses were atraumatic retinal detachment, keratitis, glaucoma, uveitis, eye trauma, conjunctivitis, and eye pain (not resulting in another diagnosis). These diagnoses were selected as they have been reported internationally (atraumatic retinal detachment, uveitis, eye trauma),Citation12 they were among most common ophthalmic diagnoses seen in our EDs—eye trauma, eye pain (not resulting in another diagnoses), conjunctivitis—or they did not fall in those categories but were potentially vision threatening without timely treatment (keratitis).
Differences in mean daily presentation numbers for the total number of presentations and for each diagnosis during the COVID-19 lockdowns and post-lockdown period were assessed with non-paired Student’s t-test with Bonferroni correction. All data analysis was performed in Excel (Microsoft). This study was approved by the Western Sydney Local Health District Human Research Ethics Committee as a quality assurance project and was conducted in accordance with the tenets of the Declaration of Helsinki.
Results
Overall, total ophthalmic presentations per day between March 29 and May 31, 2020 (the lockdown period) fell by 16% compared to the corresponding period in 2019 (13.0 ± 4.0 in 2019 vs 10.8 ± 3.3 in 2020, mean ± standard deviation; difference −2.1 presentations per day; 95% confidence interval: −1.6 to −0.5, p=0.01). This fall was reflected across the acuities of presentation (as measured by triage categories) and final dispositions. In particular, there was a dramatic decrease in patients who did not wait to be seen (down 80%, p<0.01) ().
Table 1 Mean Daily Ophthalmology Presentations to Western Sydney Local Health District Emergency Departments From March 29 to May 31 in 2019 and 2020
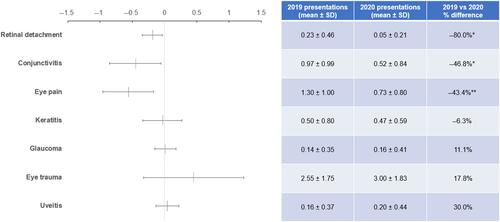
Seven common and/or time-sensitive, vision threatening presentations were examined further (). There was a significant decrease in presentations of atraumatic retinal detachment, conjunctivitis, and eye pain (not resulting in another diagnosis). While average daily presentations with diagnoses of glaucoma, eye trauma and uveitis were higher in 2020 compared to 2019, the differences were not statistically significant.
Figure 1 Difference in Common Ophthalmic Presentations to Emergency Departments in the Western Sydney Local Health District Per Day During Corresponding Two-month Time Periods (March 29 to May 31) in 2019 vs 2020.
Between June 1 and July 31, 2020 (the post-lockdown period), total ophthalmic presentations per day returned to the same level as that of the corresponding period in 2019 (12.2 ± 4.3 in 2019 vs 12.3 ± 4.1 in 2020, p=0.97).
Discussion
Our audit has demonstrated that during the lockdowns associated with the first wave of the COVID-19 pandemic in Australia, there was a fall in the total number of daily ophthalmic presentations to EDs compared to the previous year. In particular, there was a decrease in the number of presentations with atraumatic retinal detachments, conjunctivitis, and eye pain (not resulting in another diagnosis). In the two months following easing of lockdown restrictions, the total number of daily ophthalmic presentations to EDs returned to the same levels as the previous year.
Incidences of the presentations described with year-on-year declines may have truly fallen. For example, social distancing may have limited spread of infectious conjunctivitis. Reductions in presentations of atraumatic retinal detachments and eye pain, however, are harder to explain and may reflect issues beyond decreased incidence.
In the worst case, reductions in presentations of atraumatic retinal detachments and eye pain may represent delays in patients seeking appropriate medical attention for symptoms of visual loss/dysfunction. Suspension/closure of outpatient clinics, elective procedures, non-urgent clinical care, and primary care provision has affected access for patients in health care settings globally.Citation13,Citation14 In the case of urgent/emergent ophthalmic care, reduced access to primary care facilities such as optometrists and general practitioners may have further exacerbated issues around access to service as many patients are familiar with initially seeking advice from primary care practitioners as a pathway to specialist care.Citation12 This may have been further compounded by the general public’s anxiety and the stigma associated with presenting to a hospital during the COVID-19 pandemic.Citation15
Volumes of keratitis, glaucoma, eye trauma and uveitis presentations during the COVID-19 lockdown period were not significantly different to the preceding year. Considering the widespread reduction in outpatient ophthalmic services however, this may also indicate a failure to seek appropriate medical attention as increase in these types of presentations to EDs would be expected if other outpatient services were not available. Interestingly, there was no increase in presentation of any condition, which might have been expected due to decreased non-urgent follow-ups/treatment in the community or delayed non-urgent surgery.Citation16
Our findings in terms of decreased total ophthalmic presentations in the Australian context reflect findings seen in the UK but to a lesser degree. In our study, the number of ophthalmic presentations per day over the lockdown period decreased 16% compared to the preceding year. At the primary campus of Moorfields Eye Hospital in London, UK, total attendances to their accident and emergency department and their emergency telehealth service for the period March 15 to April 25, 2020 fell 60% compared to the previous year.Citation12 The lesser degree to which presentations have fallen in the Australian context may be a reflection in the difference in the impact of COVID-19 in Australia vs the UK. Early in the pandemic, the UK was one of the hardest hit nations, with shortages of personal protective equipment, high daily death rates and, surging intensive care unit demand,Citation17–Citation19 In comparison, Australia achieved relatively rapid control of disease spread and thus potentially lower levels of public anxiety and suspension of normal medical services.Citation1
In terms of reduction in the number of retinal detachment presentations, our findings also reflect those from recent reports from the UK. In our study, the number of retinal detachment presentations per day over the COVID-19 lockdown period fell 80% compared to the preceding year. In the period of March to April 2020, the Moorfields Eye Hospital saw a 62% drop in the average number of retinal detachment operations performed per week.Citation12 Similarly, across all vitreoretinal units in Scotland, a 55% decrease in the number of retinal detachments was seen in the five weeks following introduction of lockdowns (March 25, 2020 to April 29, 2020) compared to the average of the four five-week periods (excluding Christmas and New Year) leading up to March 25, 2020.Citation20 These changes may reflect issues beyond decreased incidence as outlined.
Delayed access to appropriate care due to COVID-19 will likely have long-lasting impacts.Citation15 For example, a recent report across all vitreoretinal units in Scotland found a decrease in the proportion of retinal detachments that are macula-on at presentation from 44.2% in the pre-COVID lockdown period to 34.9% following COVID-19 lockdowns.Citation20 As the visual outcomes of macula-on retinal detachments are superior to macula-off, this is likely to represent a significant ongoing burden of disease.Citation21,Citation22
This study has several limitations. Firstly, as ICD-10-AM coding data was used, there is a potential for coding errors, eg due to coder training, variance in electronic record keeping, and/or misspecification.Citation23 In this study, however, these errors are unlikely to have substantially affected the findings of our study for two main reasons: one, we have a team of professionally trained coders in our hospitals and, two, the rate of errors is likely to be similar between periods. Secondly, due to this study’s focus on ED presentations and diagnoses, it may not accurately reflect the true diagnoses patients have had following specialist review, ie any changes in diagnoses following a patient’s discharge from ED (particularly if they were discharged to the Eye Clinic for input, the final diagnosis would not be reflected in the study data). Finally, as the study was focused on a group of hospitals within a geographically focused metropolitan health-care network, there is a limitation on its validity to the rural Australian context.
There are, however, some strengths to this study. Firstly, it is a multicenter study including all sites of one of the largest health-care networks in Australia, thus increasing its validity to the broader metropolitan Australian context. Secondly, by capturing and studying a period of lockdown easing, this study provides an indication of expected returns of presentation patterns in the post-lockdown period. This will be valuable to services planning their post-COVID recovery strategies.
Conclusion
COVID-19 has profoundly affected health-care delivery globally. Our analysis shows concerning year-on-year reduction in total ophthalmic presentations and selected vision threatening diagnoses in the Australian context. These may represent delays in patients seeking appropriate medical attention and may have implications on patient morbidity long after the COVID-19 pandemic. Further studies of patients presenting to ophthalmic services as they reopen will be required to fully appreciate the lasting implications of the COVID-19 pandemic.
Disclosure
The authors report no conflicts of interest in this work.
References
- McAnulty JM, Ward K. Suppressing the Epidemic in New South Wales [Correspondence]. N Engl J Med. 2020;382(21):e74. doi:10.1056/NEJMc2011592
- Wahlquist C Australia’s coronavirus lockdown: the first 50 days. The Guardian [Australian edition]. 2020. Available from: https://www.theguardian.com/world/2020/may/02/australias-coronavirus-lockdown-the-first-50-days. Accessed December 16, 2020.
- Australian Government Department of Health. Coronavirus (COVID-19) Advice for older people. 2020. Department of Health. Australian Government. Available from: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/advice-for-people-at-risk-of-coronavirus-covid-19/coronavirus-covid-19-advice-for-older-people. Accessed December 16, 2020.
- NSW Health. New COVID-19 Restrictions in Place Across NSW: 1 June 2020. NSW Government; 2020. Available from: https://www.nsw.gov.au/news/new-covid-19-restrictions-place-across-nsw. Accessed December 16, 2020.
- De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy [Correspondence]. N Engl J Med. 2020;383(1):88–89. doi:10.1056/NEJMc2009166
- Morelli N, Rota E, Terracciano C, et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 Era. Eur Neurol. 2020;82(2):1–3.
- Kam AW, Chaudhry SG, Gunasekaran N, et al. Fewer presentations to metropolitan emergency departments during the COVID-19 pandemic. Med J Aust. 2020;213(8):370–371. doi:10.5694/mja2.50769
- Australian Bureau of Statistics. Australian Demographic Statistics, Dec 2019. Canberra, Australia: Australian Government; 2020. Available from: https://www.abs.gov.au/ausstats/[email protected]/Latestproducts/3101.0Main%20Features3Dec%202019?opendocument&tabname=Summary&prodno=3101.0&issue=Dec%202019&num=&view=. Accessed December 16, 2020.
- HealthStats NSW. Population by Local Health District. Sydney, NSW: NSW Government; 2020. Available from: http://www.healthstats.nsw.gov.au/Indicator/dem_pop_lhnmap/dem_pop_lhnmap_snap. Accessed December 16, 2020.
- Hansen DP, Kemp ML, Mills SR, et al. Developing a national emergency department data reference set based on SNOMED CT. Med J Aust. 2011;194(4):S8–10. doi:10.5694/j.1326-5377.2011.tb02934.x
- Berendsen Russell S, Dinh MM, Bell N. Triage, damned triage … and statistics: sorting out redundancy and duplication within an emergency department presenting problem code set to enhance research capacity. Australas Emerg Nurs J. 2017;20(1):48–52. doi:10.1016/j.aenj.2016.09.004
- Wickham L, Hay G, Hamilton R, et al. The impact of COVID policies on acute ophthalmology services—experiences from Moorfields Eye Hospital NHS Foundation Trust. Eye. 2020;34(7):1189–1192. doi:10.1038/s41433-020-0957-2
- Tam -C-CF, Cheung K-S, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi:10.1161/CIRCOUTCOMES.120.006631
- Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;10.
- Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19 [Correspondence]. N Engl J Med. 2020;382(24):2368–2371. doi:10.1056/NEJMms2009984
- Napoli PE, Nioi M, d’Aloja E, et al. Safety recommendations and medical liability in ocular surgery during the COVID-19 Pandemic: an Unsolved Dilemma. J Clin Med. 2020;9(5):1403. doi:10.3390/jcm9051403
- British Broadcasting Network. Coronavirus: intensive care demand surged at peak of crisis. 2020. Available from: https://www.bbc.com/news/uk-scotland-52922818. Accessed December 16, 2020.
- England NHS. COVID-19 Daily Deaths. London, UK: National Health Service; 2020. Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-daily-deaths/. Accessed December 16, 2020.
- Campbell D NHS staff told ‘wear aprons’ as protective gowns run out. The Guardian. 2020. Available from: https://www.theguardian.com/world/2020/apr/17/nhs-staff-to-be-asked-to-treat-coronavirus-patients-without-gowns. Accessed December 16, 2020.
- Shams F, El-Abiary M, Goudie C, et al. Effects of lockdown on retinal detachment incidence in Scotland. Eye. 2020. doi:10.1038/s41433-020-1029-3
- Rezar S, Sacu S, Blum R, et al. Macula-on versus macula-off pseudophakic rhegmatogenous retinal detachment following primary 23-gauge vitrectomy plus endotamponade. Curr Eye Res. 2016;41(4):543–550. doi:10.3109/02713683.2015.1031351
- Borowicz D, Nowomiejska K, Nowakowska D, et al. Functional and morphological results of treatment of macula-on and macula-off rhegmatogenous retinal detachment with pars plana vitrectomy and sulfur hexafluoride gas tamponade. BMC Ophthalmol. 2019;19(1):118. doi:10.1186/s12886-019-1120-3
- O’Malley KJ, Cook KF, Price MD, et al. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40(5 Pt 2):1620–1639. doi:10.1111/j.1475-6773.2005.00444.x
