Abstract
Purpose
The aim of this study was to show the efficiency of preoperative botulinum toxin A (Botox A) in patients with benign essential blepharospasm who were to undergo ocular surgery with local anesthesia.
Materials and methods
Twenty-eight benign essential blepharospasm patients who were administered unilateral Botox A prior to ocular surgery between January 2004 and May 2011 were included in this study. Eleven cases had pterygiums, ten had cataracts, and four had glaucomas, while the remaining three had aphakia. All cases’ severity of spasm (stage 0–4) and eyelid closing forces (stage 1–4) were evaluated according to the Jankovic scale prior to the injection, at 3 days, 14 days, 1 month, and 3 months after Botox A injection.
Results
Of the patients enrolled in the study, 16 were female and 12 were male, with an average age of 55.52 ± 1.53 years (52–65). Average onset of the Botox injection’s effect was 2.8 ± 0.9 (2–5) days. Its effect lingered for about 11.5 ± 3.6 (8–22) weeks. The severity of spasm and eyelid closing forces of all the patients enrolled were compared prior to the injection at 3 and 14 days and the first and third months after the injection. There were statistically significant differences between prior to the injection and 3 days (P = 0.001), 14 days (P < 0.001) and 1 month after the injection (P < 0.001). There was no statistically significant difference between prior to the injection and 3 months after the injection (P = 0.513). Fourteen days following the injection, the surgeries were successfully performed.
Conclusion
Botox A administered prior to ocular surgery will control both blepharospasm and lower the risks that can be encountered before and during surgery, thus increasing the comfort of the patient and the surgeon.
Introduction
Benign essential blepharospasm (BEB) is thought to be due to overexcitement of the neurons in the brain stem that results from the organic dysfunction of the basal ganglia, characterized by involuntary overcontraction of the orbicularis oculi.Citation1–Citation3 BEB typically has an onset in the sixth decade, and it is more common in women.Citation4 The main symptoms of blepharospasm are grumbling facial expression, fluttering of eyelids, increase in the frequency of blinking, and chronic involuntary contractions that eventually affect both eyes. In cases with BEB, tonic essential spasm of the orbicularis oculi muscle can lead to total closure of both eyelids.Citation5 As a result, activities such as reading, writing, and driving become hard to accomplish for patients, with blepharospasms having a negative effect on the quality of life.Citation6
Botulinum toxin type A (Botox A) enables neuromuscular blockade by preventing acetylcholine secretion from the presynaptic vesicles. Botox A is currently the gold-standard therapy of benign essential blepharospasm due to its efficiency and safety.Citation7,Citation8
Ocular surgeries can be performed by using topical or local anesthetics. However, performing surgery in patients with tonic contraction of eyelids could be hard for both the surgeon and the patient. Additionally, preoperative anxiety of the patient, preoperative pain, and exposure to the light of the surgery microscope can cause an increase in the frequency of blinking and involuntary contractions. Surgery in a patient with persistent involuntary contractions of the eyelids is an undesired condition. The aim of this study was to show the efficacy of Botox A in patients with benign essential blepharospasm who were to undergo ocular surgery under local anesthesia.
Materials and methods
Twenty-eight BEB patients who were administered with unilateral Botox A prior to ocular surgery between January 2004 and May 2011 were included in this study. Eleven cases had pterygiums, ten had cataracts, and four had glaucomas, while the remaining three had aphakia. The diagnosis of BEB was ascertained by detailed ophthalmic and neurological examination. Patients who had systemic and neurological disorders and those who had previous Botox A injections were excluded from the study. Prior to the study, informed consent was obtained from the patients and local ethics committee approvals were completed according to Declaration of Helsinki. Severity of spasm (stage 0–4) and eyelid closing force (stage 1–4) were evaluated according to the Jankovic scale prior to the injection and at 3 days, 14 days, 1 month, and 3 months after Botox A injectionCitation9,Citation10 ().
Table 1 Severity of spasm and eyelid closing force scores
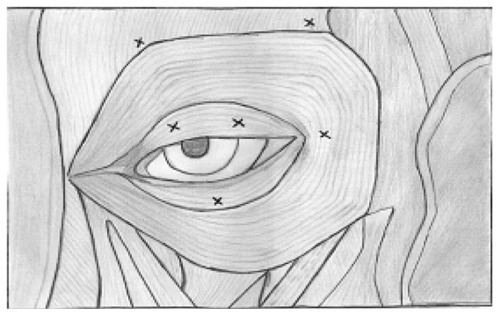
A Botox A vial (100 U) was diluted with 4 mL of saline that included no preservatives (0.9% NaCl). After the dilution, a solution that had 2.5 U of Botox A in each 0.1 mL was obtained. The areas that would be injected were marked after being cleansed by 10% povidone iodine solution. No other drugs were used, in order to prevent drug interaction. From the solution obtained, six injections were made with a 27-gauge insulin syringe. These injections were made to lateral and medial connections of the preseptal and orbital parts of the orbicularis oculi muscle, lateral and medial part of the pretarsal orbicularis oculi muscle of the upper eyelid, lateral part of the lateral canthus, and pretarsal region of the lower eyelid (). Compression was performed in the areas where injections were made. The severity of spasm and eyelid closing force for all the patients enrolled were measured according to the Jankovic scale prior to the injection and at 3 days, and 14 days, 1 month, and 3 months after injection and compared.
Fourteen days after the injection, patients underwent ocular surgery under topical and/or sub-Tenon’s anesthesia by using eye speculum. Topical anesthesia was provided by 0.5% proparacaine drops (Alcaine®; Alcon Laboratories, Inc, Fort Worth, TX), while sub-Tenon’s anesthesia was provided by a 2-cc injection of lidocaine HCl 20 mg/mL, epinephrine HCI 0.0125 mg/mL (Jetocain; Adeka, Samsun, Turkey). No sedatives were used for patients that may have interrupted the blepharospasm symptoms. The patients were evaluated for anterior segment and fundus, and intraocular pressure (IOP) was measured after operation.
Statistical analyses were performed using the Statistical Package for the Social Sciences (version 12.0; IBM, Armonk, NY). The Wilcoxon signed-rank test was used for the statistical analysis of severity of spasm and eyelid closing force prior to the injection and after injection. A P value of <0.05 was accepted as statistically significant.
Results
Of the 28 patients enrolled in the study, 16 were female and 12 were male. The average age of the patients was 55.52 ± 1.53 years (52–65 years). Eye specula were used on all patients without trouble. There were not any complications due to involuntary eyelid contractions during surgery. Eleven eyes of eleven patients underwent pterygium excision and conjunctival autograft surgeries under subconjunctival anesthesia. Ten eyes of ten patients underwent phacoemulsification and intraocular lens implantation surgeries for cataract under topical anesthesia. Four patients underwent trabeculectomy under retrobulbar anesthesia. Three patients underwent secondary intraocular lens implantation under sub-Tenon’s anesthesia ().
Table 2 Subject details
The severity of spasm and eyelid closing forces of all the patients enrolled were compared prior to the injection and at 3 days, 14 days and 1 and 3 months after the injection. There were statistically significant differences between prior to the injection and 3 days (P = 0.001), 14 days (P = 0.001) and 1 month after the injection (P = 0.001). There was no statistically significant difference between prior to the injection and 3 months after the injection (P = 0.513) ().
Table 3 Comparison of severity of spasm and eyelid closing force scores before and after Botox A injection
Corneal sutures of the patients who were given intraocular lenses with scleral fixation due to aphakia were removed in an average of 36.6 ± 6 days (30–42 days).
The average corrected preoperative visual acuity of the patients with cataract was 20/200 (20/640–20/80), while the postoperative value was 20/32 (20/80–20/25). Preoperative and postoperative values for patients who were given intraocular lenses with scleral fixation were 20/400 and 20/50, respectively. Preoperative and postoperative average IOP values for patients with glaucoma were 28.7 ± 3.6 mmHg and 18 ± 3.2 mmHg, respectively. Average onset of the Botox injection’s effect was 2.8 ± 0.9 (2–5) days. Its effect lingered for about 11.5 ± 3.6 (8–22) weeks. In follow-ups, it was determined that the effects of the injections were more evident on the 14th day and that the level of decrease in the blepharospasm degree and eyelid power was sufficient to let the eye speculum to be fastened.
None of the patients experienced diplopia, dry eye, keratitis, pain, lacrimation, blurry vision, or any systemic side effects. Eyelid echimosis was observed in two patients, while there was mild ptosis in one patient on the fourth postoperative day. The ptosis resolved on its own in approximately 2 months.
Discussion
Botox A is commonly used in the control of BEB, strabismus hemifacial spasm, cervical dystonia, spasticity, spastic entropion, thyroid-associated upper eyelid contraction, and also it is used as an alternative to surgical tarsorrhaphy in cases with ocular surface disorders.Citation7,Citation8,Citation11–Citation19 The toxin has received Food and Drug Administration approval for treatment of blepharospasm, strabismus, primary axillary hyperhidrosis, cervical dystonia and glabellar wrinkles, and brow furrows.Citation20,Citation21 Our indication for administrating Botox A may be presented as a novel one. BEBs of the patients were controlled by preoperative Botox injection, and the surgeries were performed under local anesthesia. Postoperative examinations of the patients were performed, procedures like IOP value were measured by using applanation tonometer, and the removal of corneal sutures were done easily. There are no reports in literature concerning the anesthesia options for blepharospasm patients who will undergo ocular surgery. Botox A injection prior to ocular surgery will increase the patient and the surgeon’s comfort alike.
Applying an eye speculum is a must in order to perform ocular surgery. However, this may be difficult in cases with blepharospasm. After establishment of the eye speculum in BEB patients during eye surgery, involuntary closure of the eyelid due to blepharospasm will lead to an elevation in intraorbital and intraocular pressure. Periodical contractions of eyelids and fluctuation of IOP due to this contraction are crucial in phacoemulsification because increments of IOP could complicate capsulorhexis, and as a result anterior chamber depth cannot be preserved. Capsular tear and endothelial damage due to reduction in anterior chamber depth can be encountered. In glaucoma surgeries and scleral fixation secondary intraocular lens implantation, there can be rapid decreases in intraocular pressures. In such instances, involuntary contractions of eyelids may pose as a threat for maintenance of anterior chamber depth. It is known that glaucoma and previous anterior vitrectomies and hypotonia are risk factors for expulsive hemorrhage.Citation22 It is important to prevent involuntary eyelid contractions and to avoid complications such as expulsive hemorrhage that can result from pulsatile intraocular pressure elevation. Endothelial damage could occur due to pulsatile contraction of eyelids in the patients who underwent intraocular lens implantation with scleral fixation. Preoperative application of Botox could protect patients having ocular surgery under local anesthesia from these potential risks. Preoperative paralyzation of the orbitacularis oculi by using local anesthetic drugs in ocular surgery of BEB patients was performed easily and safely. General anesthesia can be used as an alternative. With the aid of these procedures, perioperative akinesis was able to be achieved in both groups via safe and comfortable surgery, but long-term symptomatic healing and comfort in postoperative controls cannot be achieved by procedures other than Botox injection in BEB. Moreover, general anesthesia has some disadvantages, including premedication necessity, increase in the duration of the surgery, possible complications of general anesthesia, and increase in hospital admission duration postoperatively.
Average onset of the Botox injection’s effect was 2.8 ± 0.9 (2–5) days in our patients. According to the literature, Botox’s effect starts on the third day; the maximum effect of Botox sets in 14 days after injection.Citation11,Citation23 Therefore, the surgeries were performed 14 days after the injection. However, the time of surgery can be determined according to the patient’s status after day 3, when the effect of Botox starts. Botox’s effect lingered for about 11.5 ± 3.6 weeks. This duration is enough for most eyes’ rehabilitation. Ocular surgery and postoperative examinations of the patients were performed during this period, IOP values were measured, and the corneal sutures were removed easily. In studies in which long-term follow-ups were conducted of blepharospasm patients who had been administered Botox A, it was reported that the effect lasts 14 to 16 weeks.Citation11,Citation17,Citation24 The effect of the drug fades when the axons elongate and new neuromuscular junctions are formed.
In the control of blepharospasm, Botox A can be injected in pretarsal and preseptal regions. In our patients, we preferred the pretarsal injection, due to it being closer to the eyelid, more efficient, and having fewer complications. Some studies report that the frequency of involuntary blinking decreases more and that there are less complications with pretarsal administration, which makes it more efficient than other techniques.Citation25–Citation27 It has been reported that the average initial dose in the control of blepharospasm is between 1.25 and 5 U.Citation28 We used 2.5 U, and this dose was enough for all patients.
After Botox injection, complications such as eyelid ecchymosis, ptosis, diplopia, and watery eyes after injection in medial cantus region were reported. Following injection, there was eyelid echimosis in two patients (7%) and ptosis in one patient (3.6%). In some studies, it was reported that postinjection ptosis rates varied between 10.3% and 9.2%, and chemosis rates were between 7% and 8.2%.Citation11,Citation29 Our ptosis rates were much lower than the previous studies, suggesting these values were due to our preference of pretarsal injection.
Conclusion
Pretarsal Botox A injection in BEB patients prior to ocular surgery is an efficient and safe procedure that helps the surgery to be performed under local or topical anesthesia. Additionally, by using this procedure, postoperative examination and postoperative intervention on the eye can be performed easily.
Disclosure
The authors report no conflicts of interest in this work.
References
- JankovicJOrmanJBlepharospasm: demographic and clinical survey of 250 patientsAnn Ophthalmol19841643713766144283
- GrandasFElstonJQuinnNMarsdenCDBlepharospasm: a review of 264 patientsJ Neurol Neurosurg Psychiatry19885167677723404184
- VitekJLBakayRAFreemanARandomized trial of pallidotomy versus medical therapy for Parkinson’s diseaseAnn Neurol200353555856912730989
- AndersonRLPatelBCHoldsJBJordanDRBlepharospasm: past, present, and futureOphthal Plast Reconstr Surg1998145305317
- JankovicJHavinsWEWilkinsRBBlinking and blepharospasm. Mechanism, diagnosis, and managementJAMA198224823316031647143695
- ReimerJGilgKKarowAEsserJFrankeGHHealth-related quality of life in blepharospasm or hemifacial spasmActa Neurol Scand20051111647015595940
- OsakoMKeltnerJLBotulinum A toxin (Oculinum) in ophthalmologySurv Ophthalmol199136128461925943
- OzkanSBCanDSöylevMFArsanAKDumanSChemodenervation in treatment of upper eyelid retractionOphthalmologica199721163873909380360
- KhooHMKimJCKhooBSTreatment of blepharospasm and hemifacial spasm with botulinum toxin AKorean J Ophthalmol19903115968
- KimJCKimWSAhnSKShynKHClinical studies in patients with essential blepharospasm and with hemifacial spasmKorean J Ophthalmol19913210837843
- CillinoSRaimondiGGuépratteNLong-term efficacy of botulinum toxin A for treatment of blepharospasm, hemifacial spasm, and spastic entropion: a multicentre study using two drug-dose escalation indexesEye201024460060719648904
- DuttonJJBuckleyEGLong-term results and complications of botulinum A toxin in the treatment of blepharospasmOphthalmology19889511152915343211461
- ScottABRosenbaumACollinsCCPharmacologic weakening of extraocular musclesInvest Ophthalmol197312129249274203467
- KeenMKopelmanJEAvivJEBinderWBrinMBlitzerABotulinum toxin A: a novel method to remove periorbital wrinklesFacial Plast Surg19941021411467995530
- BrandtFSBellmanBCosmetic use of botulinum A exotoxin for the aging neckDermatol Surg19982411123212349834744
- ScottABBotulinum toxin injection into extraocular muscles as an alternative to strabismus surgeryOphthalmology19808710104410497243198
- EllisMFDaniellMAn evaluation of the safety and efficacy of botulinum toxin type A (Botox) when used to produce a protective ptosisClin Experiment Ophthalmol200129639439911778810
- SahlinSChenEKaugesaarTAlmqvistHKjellbergKLennerstrandGEffect of eyelid botulinum toxin injection on lacrimal drainageAm J Ophthalmol2000129448148610764857
- BrashearABotulinum toxin type A: exploring new indicationsDrugs Today (Barc)201046967168220967299
- GürsoyDÖztürkSBotox treatment and common treatment indicationsTurkiye Klinikleri J Med Sci2009291102103
- DurmazlarSPKEskioğluFBotulinum toxin (fundamentals before practice)Turkiye Klinikleri J Med Sci2009293702707
- GoldsmithCReneCMassive spontaneous expulsive suprachoroidal haemorrhage in a blind glaucomatous eye treated with chronic topical steroidEye200317343944012724718
- GillHSKraftSPLong-term efficacy of botulinum a toxin for blepharospasm and hemifacial spasmCan J Neurol Sci201037563163621059510
- AinsworthJRKraftSPLong-term changes in duration of relief with botulinum toxin treatment of essential blepharospasm and hemifacial spasmOphthalmology199510212203620409098314
- CakmurROzturkVUzunelFDonmezBIdimanFComparison of preseptal and pretarsal injections of botulinum toxin in the treatment of blepharospasm and hemifacial spasmJ Neurol20022491646811954870
- JankovicJApraxia of lid openingMov Disord19951056866878552131
- JankovicJPretarsal injection of botulinum toxin for blepharospasm and apraxia of eyelid openingJ Neurol Neurosurg Psychiatry19966067048648354
- KöltringerPHaselwanderHReiseckerFThe treatment of blepharospasm with botulinum toxin AWien Klin Wochenschr199013;10214403407
- YoonJSKimJCLeeSYDouble-blind, randomized, comparative study of Meditoxin versus Botox in the treatment of essential blepharospasmKorean J Ophthalmol200923313714119794937