Abstract
Background
To determine whether the intraocular pressure (IOP) in diabetic patients is significantly different from that in nondiabetic patients.
Methods
The medical records of all patients who were initially examined in the Department of Ophthalmology, Kansai Medical University, Takii Hospital were reviewed. At the initial examination, patients had a detailed interview and underwent a comprehensive ophthalmic examinations. All patients were over 20 years of age and did not have glaucoma.
Results
A total of 703 patients were evaluated. The mean (±standard error) IOP of the diabetic patients was 15.5 ± 0.2 mmHg (n = 206), and was significantly higher than the 14.0 ± 0.1 mmHg (n = 497) in the nondiabetic patients (P < 0.0001). The IOP was negatively correlated with age (r = −0.202; P = 0.024) in the diabetic patients and was weakly but significantly correlated with the glycosylated hemoglobin (HbA1c) level (r = 0.240; P = 0.015) in the group with diabetic retinopathy.
Conclusion
The significantly higher IOP in diabetic patients and positive correlation of IOP with HbA1c levels in patients with diabetic retinopathy indicate that IOP in diabetic patients is higher, especially in those with poor control of diabetes.
Introduction
Diabetes mellitus is a major public health problem, and a marked increase in the disease burden is projected by 2025.Citation1 Diabetic retinopathy is a serious microvascular complication of diabetes mellitus and is a major cause of adult blindness. Relevant to this study, several cross-sectional studies have found a positive correlation between diabetes and primary open-angle glaucoma.Citation2–Citation6 However, there have been other studies that failed to confirm this association.Citation7–Citation13 Thus, the relationship between diabetes mellitus and open-angle glaucoma has not been established.
Several population-based studies have consistently reported that intraocular pressure (IOP) is significantly higher in subjects with diabetes than in those without diabetes,Citation2–Citation7,Citation9,Citation10,Citation12,Citation14,Citation15 although some of them failed to find a positive correlation between diabetes and open-angle glaucoma.Citation7,Citation9,Citation10 The Japanese population-based Tajimi study reported that diabetic patients had significantly higher IOP, but the presence of diabetes was not significantly associated with the development of open-angle glaucoma.Citation16,Citation17 However, only limited data exist on the relationship between diabetes mellitus and IOP in the Japanese population, and earlier studies have not evaluated diabetic status, such as the glycosylated hemoglobin (HbA1c) level, and the effect of degree of diabetic retinopathy on IOP.Citation16,Citation17
Thus, the purpose of this study was to determine whether a significant correlation exists between IOP and diabetes, the degree of diabetic retinopathy, and the HbA1c level. To accomplish this, we examined the IOP of patients with diabetes mellitus and compared their IOP with that in subjects without diabetes mellitus.
Materials and methods
Participants
The procedures used in this study conformed to the tenets of the Declaration of Helsinki. The medical records of all patients who first visited the Department of Ophthalmology, Kansai Medical University Takii Hospital (Osaka, Japan) between April 2008 and July 2009 were reviewed. At the initial examination, all patients were interviewed regarding their medical history, including past ocular diseases. Patients who underwent a standard ophthalmic examination, including determination of visual acuity, refraction, slit-lamp examination, and fundus examination were included in this study.
IOP was measured routinely three times with a noncontact tonometer (Topcon CT90, Topcon, Tokyo, Japan), and the average of the right eye was used for the statistical analyses. Patients who were <20 years old, had corneal disease, uveitis, ocular inflammatory disease, and fundus diseases except for diabetic retinopathy were excluded. In addition, patients who had undergone any intraocular surgery, eg, for cataract, vitrectomy, glaucoma, or buckling surgery, were excluded. However, patients with mild cataracts in whom the fundus could be examined were included. Patients with definite glaucoma, suspected glaucoma,Citation9,Citation16,Citation17 or other types of glaucoma, including neovascular glaucoma, and those who were receiving IOP-lowering treatments were excluded. HbA1c levels determined by standard laboratory procedures were obtained from medical records.
Classification of diabetic retinopathy
All patients included in this study underwent a standard ophthalmic examination at the initial visit. The stage of diabetic retinopathy was determined by ophthalmoscopy and fluorescein angiography. The patients were classified according to the severity of diabetic retinopathy; ie, no apparent diabetic retinopathy, mild to moderate nonproliferative diabetic retinopathy, severe nonproliferative diabetic retinopathy, and proliferative diabetic retinopathy.Citation18 Patients identified to have proliferative diabetic retinopathy underwent routine gonioscopy to exclude neovascular glaucoma. The association between IOP and the presence or absence of diabetes mellitus, gender, age, stage of diabetic retinopathy, and HbA1c level were evaluated.
Statistical analyses
The results are expressed as the mean ± standard error of the mean (SEM), and the data were analyzed statistically using the Mann–Whitney test and one-way analysis of variance with Dunnett’s correction when comparing groups. Associations between the parameters were examined by Pearson’s product moment correlation coefficients (r). The statistical analysis package SPSS 14.0 for Windows (SPSS Inc, Chicago, IL) was used for statistical processing. A P value < 0.05 was accepted as significant.
Results
Of the 703 patients, 206 were diagnosed with diabetes and 497 without diabetes. The mean (±standard deviation) age of the 206 diabetic patients was 61.4 ± 11.9 years with a range of 21 to 85 years. The 206 diabetic patients included 140 men (age 60.6 ± 10.8 years) and 66 women (age 63.2 ± 13.9 years). The mean age of the 497 nondiabetic patients was 61.7 ± 15.6 years with a range from 21 to 95 years. The 497 nondiabetic patients included 210 men (age 58.8 ± 16.2 years) and 287 women (age 63.9 ± 14.8 years).
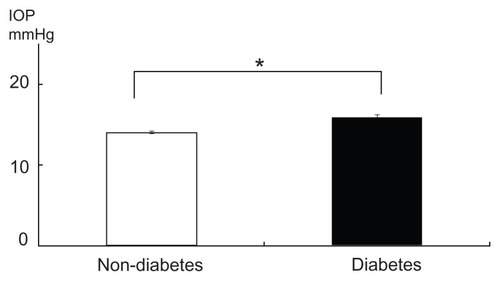
The mean (±SEM) IOP was 14.0 ± 0.12 mmHg in the nondiabetic group and 15.5 ± 0.24 mmHg in the diabetic group (). The IOP in the diabetic patients was significantly higher than that in the nondiabetic patients (P < 0.0001, Mann–Whitney test).
Figure 1 IOP in patients with and without diabetes.
Abbreviation: IOP, intraocular pressure.
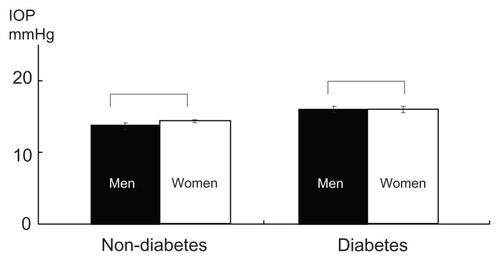
In the nondiabetic group, the mean IOP was 13.9 ± 0.2 mmHg in men (n = 210) and 14.2 ± 0.36 mmHg in women (n = 287); in the diabetic group, the mean IOP was 15.4 ± 0.27 mmHg in men (n = 140) and 15.8 ± 0.46 mmHg in women (n = 66, ). Differences in IOP between the men and women in both groups were not significant (P = 0.17 in nondiabetic group, P = 0.64 in diabetes group, Mann–Whitney test).
Figure 2 Effect of gender on IOP.
Abbreviation: IOP, intraocular pressure.
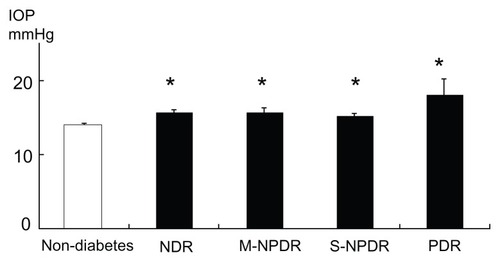
The IOP was 15.6 ± 0.4 mmHg in patients with no apparent diabetic retinopathy (n = 95, age 61.1 ± 13.4 years), 15.7 ± 0.5 mmHg in patients with mild to moderate nonproliferative diabetic retinopathy (n = 46, 65.8 ± 9.16 years), 15.0 ± 0.5 mmHg in patients with severe nonproliferative diabetic retinopathy (n = 41, 60.2 ± 10.8 years), and 18.0 ± 2.2 mmHg in patients with proliferative diabetic retinopathy (n = 24, 56.9 ± 9.19 years, ). The IOP in each diabetic retinopathy group was significantly higher than that in the nondiabetic group (P < 0.001, one-way analysis of variance with Dunnett’s test) but there was no significant difference between the diabetic retinopathy groups.
Figure 3 Effect of progression of diabetic retinopathy on IOP.
Abbreviations: IOP, intraocular pressure; NDR, no apparent diabetic retinopathy; M-NPDR, mild to moderate nonproliferative diabetic retinopathy; S-NPDR, severe nonproliferative diabetic retinopathy; PDR, proliferative diabetic retinopathy.
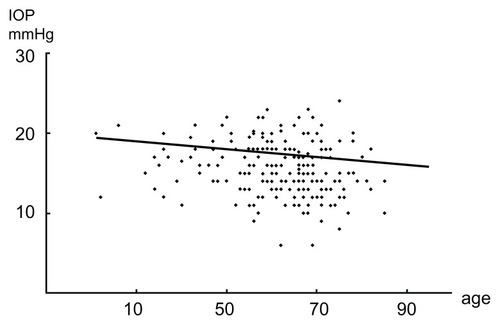
The IOP decreased significantly with increasing age in the diabetic patients, and a calculation of Pearson’s product moment correlation coefficient (r) between IOP and age showed that the correlation was significant (r = −0.202, P = 0.024, n = 206, ). The IOP also decreased with increasing age in the nondiabetic group but the decrease was not significant (r = −0.07, P = 0.12, n = 497).
Figure 4 Effect of age on IOP in diabetic patients.
Abbreviation: IOP, intraocular pressure.
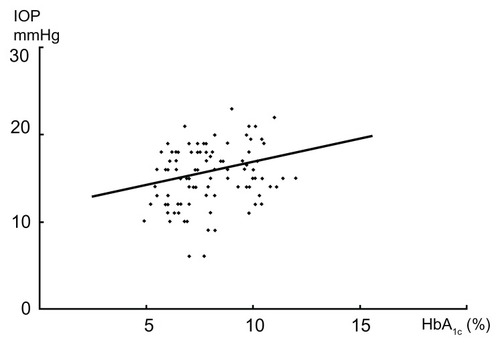
The IOP of diabetic patients increased with increasing HbA1c but the correlation was not significant (r = 0.142, P = 0.058, n = 179). When we examined the IOP of patients with diabetic retinopathy (patients with mild to moderate nonproliferative diabetic retinopathy, severe nonproliferative diabetic retinopathy, and proliferative diabetic retinopathy), there was a significant correlation between IOP and HbA1c level (r = 0.240, P = 0.015, n = 102, ).
Figure 5 IOP and HbA1c in patients with diabetic retinopathy.
Abbreviations: IOP, intraocular pressure; HbA1c, glycosylated hemoglobin; M-NPDR, mild to moderate nonproliferative diabetic retinopathy; S-NPDR, severe nonproliferative diabetic retinopathy; PDR, proliferative diabetic retinopathy.
Discussion
Both glaucoma and diabetic retinopathy are leading causes of irreversible blindness worldwide.Citation19,Citation20 Diabetes mellitus is known to cause microvascular damage and may affect the autoregulatory action of the blood vessels in the retina and optic nerve. Diabetes has been found to be associated with elevated IOP and has therefore been suggested to be a possible risk factor for glaucoma, particularly open-angle glaucoma.Citation2–Citation6
However, the evidence to support this relationship remains inconsistent. The Baltimore Eye SurveyCitation7 and some other studiesCitation10,Citation16 reported that diabetes was significantly associated with higher IOP but not with the development of open-angle glaucoma. In addition, the recent Beijing Eye studyCitation9 reported that ocular hypertension was significantly associated with diabetes as assessed independently in multivariate analysis but the prevalence of glaucomatous optic nerve damage was not associated with diabetes.
The gold standard for the measurement of IOP is the Goldmann applanation tonometer. However, IOP by noncontact tonometer is very popular and widely used for routine ocular examination and correlates well with the Goldmann applanation tonometer. Thus, we reviewed the IOP data from those patients who were examined routinely with a noncontact tonometer. Our results showed that patients with diabetes mellitus had significantly higher IOP than did nondiabetic patients.
The mechanisms that cause higher IOP in diabetic patients were not determined. An epidemiological study of the association between ocular hypertension and family history of patients with type 2 diabetes mellitus reported that genetic factors may play some role in ocular hypertension.Citation21 Another study showed that dysfunction of the autonomic system in diabetic patients might contribute to increased IOP.Citation22 It has been suggested that elevated blood glucose levels induces an osmotic gradient with consequent fluid shifts into the intraocular space which elevates the IOP.Citation5
In addition, several large population-based cross-sectional studies have documented a significant correlation between elevated blood glucose or HbA1c levels and raised IOP in diabetic patients.Citation2–Citation4,Citation6,Citation10,Citation15 We also found that the IOP was significantly correlated with HbA1c in patients with diabetic retinopathy, although the stage of diabetic retinopathy was not associated with IOP. Thus, high glucose in the blood or some aspects of glucose metabolism could affect IOP. Although a mean difference of 1.5 mmHg may not be clinically irrelevant in nonglaucomatous patients, it should be noted that HbA1c levels raise IOP in diabetic patients.
In this study, IOP was not significantly associated with gender in either the diabetic or nondiabetic group, which is in agreement with the results of earlier studies.Citation19 Many studies have shown that the IOP increases with age.Citation3,Citation11,Citation14,Citation19 However, the recent BeijingCitation9 study did not find any significant correlation between IOP and age. Moreover, the Tajimi studyCitation16 reported a significant negative correlation between age and IOP in the adult Japanese population. Therefore, the relationship between IOP and age is contradictory.
Our finding that the correlation between IOP and age was not significant in nondiabetic patients disagrees with the finding of the Tajimi study,Citation16,Citation17 but IOP decreased significantly with increasing age in patients with diabetes. One reason for this discrepancy in nondiabetic patients is that the Tajimi study was population-based, which was not the case in our study. Another reason may be that patients with glaucoma were excluded from our study.
The present study has some limitations. First, measurement of central corneal thickness (CCT) was not carried out. IOP measurement may depend on CCT,Citation23 and the CCT of diabetic patients has been reported to be greater when compared with that of nondiabetic patients.Citation24,Citation25 Even with use of the noncontact tonometer, the IOP measurement is still affected by CCT.Citation26 Thus, we may be concerned about the influence of a thick CCT on IOP measurement in diabetic patients. IOP is usually examined routinely, but CCT values are not examined routinely, so higher IOP levels in diabetics should be still considerable. In addition, glycation-induced corneal collagen cross-links in diabetes can cause corneal stiffening,Citation27 which has also been shown to increase the value of the measured IOP over the true IOP.Citation28,Citation29 Further, IOP is at least partly genetically mediated.Citation30 We only investigated the Japanese population, so it is possible that data from different genetic populations may yield different statistical results. In addition, this was a retrospective study. However, our results add to the evidence that diabetic patients have significantly higher IOPs, although this study was not designed to determine the mechanism for this relationship.
In conclusion, our findings showed that patients with diabetes mellitus had significantly higher IOP than nondiabetic patients. In addition, there was a significant positive correlation between IOP and HbA1c levels in patients with diabetic retinopathy. These findings indicate that diabetic patients have higher IOP, especially those with poor control of diabetes.
Disclosure
The authors report no conflicts of interest in this work.
References
- KingHAubertREHermanWHGlobal burden of diabetes, 1995–2025: prevalence, numerical estimates, and projectionsDiabetes Care1998219141414319727886
- KleinBEKleinRJensenSCOpen-angle glaucoma and older-onset diabetes. The Beaver Dam Eye StudyOphthalmology19941017117311778035979
- KleinBEKleinRLintonKLIntraocular pressure in an American community. The Beaver Dam Eye StudyInvest Ophthalmol Vis Sci1992337222422281607232
- DielemansIde JongPTStolkRVingerlingJRGrobbeeDEHofmanAPrimary open-angle glaucoma, intraocular pressure, and diabetes mellitus in the general elderly population. The Rotterdam StudyOphthalmology19961038127112758764798
- MitchellPSmithWCheyTWangJJChangAOpen-angle glaucoma and diabetes: The Blue Mountains Eye Study, AustraliaOphthalmology199710447127189111268
- ChopraVVarmaRFrancisBAWuJTorresMAzenSPLos Angeles Latino Eye Study GroupType 2 diabetes mellitus and the risk of open-angle glaucoma the Los Angeles Latino Eye StudyOphthalmology2008115222723217716734
- TielschJMKatzJQuigleyHAJavittJCSommerADiabetes, intraocular pressure, and primary open-angle glaucoma in the Baltimore Eye SurveyOphthalmology1995102148537831041
- QuigleyHAWestSKRodriguezJMunozBKleinRSnyderRThe prevalence of glaucoma in a population-based study of Hispanic subjects: Proyecto VERArch Ophthalmol2001119121819182611735794
- XuLWangYXJonasJBWangYSWangSOcular hypertension and diabetes mellitus in the Beijing Eye StudyJ Glaucoma2009181212519142130
- TanGSWongTYFongCWAungTSingapore Malay Eye StudyDiabetes, metabolic abnormalities, and glaucomaArch Ophthalmol2009127101354136119822853
- LeAMukeshBNMcCartyCATaylorHRRisk factors associated with the incidence of open angle glaucoma: the Visual Impairment ProjectInvest Ophthalmol Vis Sci20034493783378912939292
- EllisJDEvansJMRutaDAGlaucoma incidence in an unselected cohort of diabetic patients: is diabetes mellitus a risk factor for glaucoma? DARTS/MEMO collaboration. Diabetes Audit and Research in Tayside Study. Medicines Monitoring UnitBr J Ophthalmol200084111218122411049943
- de VoogdSIkramMKWolfsRCIs diabetes mellitus a risk factor for open angle glaucoma? The Rotterdam StudyOphthalmology2006113101827183116884777
- WuSYLeskeMCAssociations with intraocular pressure in the Barbados Eye StudyArch Ophthalmol199711512157215769400792
- HennisAWuSYNemesureBLeskeMCBarbados Eye Studies GroupHypertension, diabetes, and longitudinal changes in intraocular pressureOphthalmology2003110590891412750088
- KawaseKTomidokoroAAraieMIwaseAYamamotoTTajimi Study Group; Japan Glaucoma SocietyOcular and systemic factors related to intraocular pressure in Japanese adults: the Tajimi studyBr J Ophthalmol20089291175117918669541
- SuzukiYIwaseAAraieMRisk factors for open-angle glaucoma in a Japanese population: The Tajimi StudyOphthalmology200611391613161716828504
- WilkinsonCPFerrisFL3rdKleinREGlobal Diabetic Retinopathy Project GroupProposed international clinical diabetic retinopathy and diabetic macular edema disease severity scalesOphthalmology200311091677168213129861
- QuigleyHANumber of people with glaucoma worldwideBr J Ophthalmol19968053893938695555
- WongTYLoonSCSawSMThe epidemiology of age related eye diseases in AsiaBr J Ophthalmol200690450651116547337
- ClarkCVMapstoneRThe prevalence of diabetes mellitus in the family history of patients with primary glaucomaDoc Ophthalmol1986621611633956366
- MapstoneRClarkCVPrevalence of diabetes in glaucomaBr Med J (Clin Res Ed)198529164889395
- BrandtJDBeiserJAKassMAGordonMOCentral corneal thickness in the Ocular Hypertension Treatment Study (OHTS)Ophthalmology2001108101779178811581049
- OzdamarYCankayaBOzalpSAcarogluGKarakayaJOzkanSSIs there a correlation between diabetes mellitus and central corneal thickness?J Glaucoma201019961361620051882
- OriowoOMProfile of central corneal thickness in diabetics with and without dry eye in a Saudi populationOptometry200980844244619635436
- DomkeNHagerAWiegandWIntraocular pressure and corneal thickness. A comparison between non-contact tonometry and applanation tonometryOphthalmologe20061037583587 German16786183
- SadyCKhosrofSNagarajRAdvanced Maillard reaction and crosslinking of corneal collagen in diabetesBiochem Biophys Res Commun199521437937977575546
- BromanATCongdonNGBandeen-RocheKQuigleyHAInfluence of corneal structure, corneal responsiveness, and other ocular parameters on tonometric measurement of intraocular pressureJ Glaucoma200716758158818091174
- KruegerRRRamos-EstebanJCHow might corneal elasticity help us understand diabetes and intraocular pressure?J Refract Surg2007231858817269248
- van KoolwijkLMRamdasWDIkramMKCommon genetic determinants of intraocular pressure and primary open-angle glaucomaPLoS Genet201285e1002611 Epub May 3, 201222570627